Performing cataract surgery on glaucoma patients often involves challenges beyond those we’d en-counter with a healthy patient. That’s especially true if the patient has a pre-existing trabeculectomy or tube shunt. To achieve a successful outcome with these patients we need to devote more time and thought to the surgery, and utilize more of our intraoperative skills.
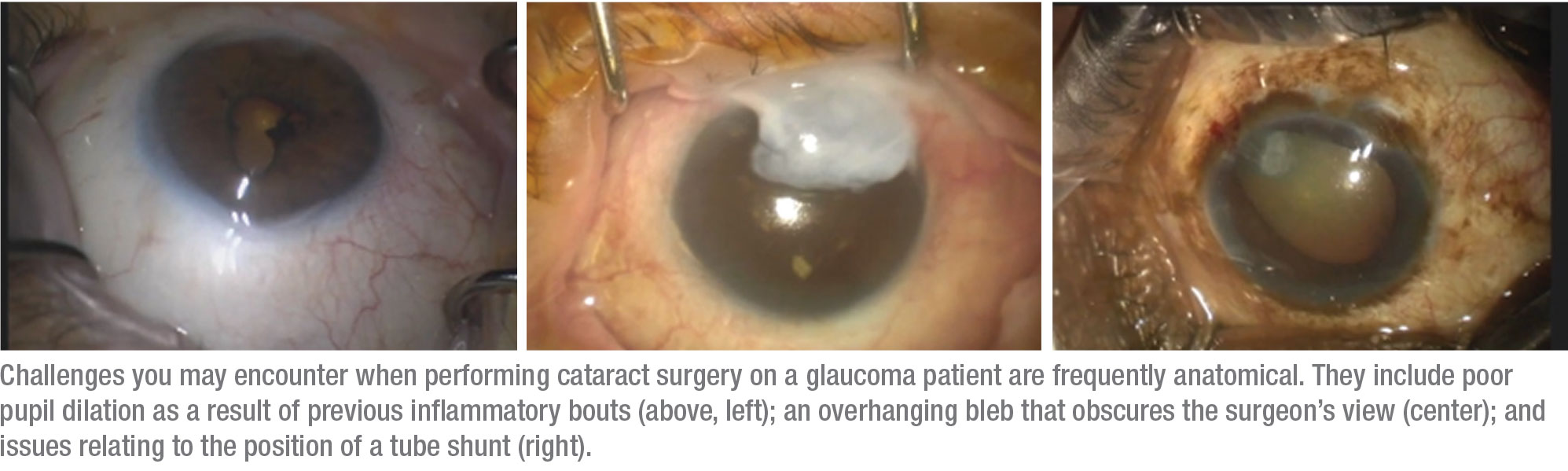
The potential problems associated with performing cataract surgery on a glaucoma patient are typically the result of anatomical factors. For example, previous inflammatory episodes may have left the pupil reluctant to dilate, possibly with posterior and/or anterior synechiae. An overhanging bleb sometimes obscures our view, requiring us to change our incision sites and possibly necessitating the removal of excess bleb tissue. If a tube is present, its position can be problematic; it may be affecting the cornea or cataract, and it may interfere with our view during the procedure. (In some cases, we may be able to work around the tube; in some cases we may need to shorten it.) (See examples, below.)
These eyes also have more post-operative issues than a healthy eye would. Postoperative inflammation is not uncommon, and that can lead to bleb failure. It can also cause postop pressure spikes, resulting in the need for more glaucoma medications. One study found that patients who had prior functional blebs undergoing even uncomplicated cataract surgery could see intraocular pressure rise by 3 mmHg.1
The message is clear: Operating on a patient with glaucoma isn’t your typical cataract surgery. Here, I’d like to offer some suggestions for steps you can take that will help to ensure an optimal outcome when working with one of these patients.
 |
Before the Surgery
When you realize you’re examining a cataract patient who has either a tube shunt or a trabeculectomy bleb, you should consider several issues:
• What’s the stage of the disease? Many choices you need to make will be based around whether the disease is controlled or uncontrolled. For example, if the patient is on one or more medications and the angle anatomy is clearly open, especially nasally, one could consider combining the cataract extraction with a minimally invasive glaucoma surgery to gain additional IOP lowering and potentially reduce the need for medications. The stage of the disease (mild, moderate or severe) can help dictate which MIGS procedure one should choose.
• Check the angle with gonioscopy. This may reveal a specific problem that’s contributing to uncontrolled IOP. For example, if you see appositional angle closure with peripheral anterior synechiae, this can alert you to the need to combine the cataract surgery with goniosynechiolysis. (You’ll find a video that describes this technique at the following link: aao.org/annual-meeting-video/role-of-goniosynechialysis-trabecular-bypass-proce.)
 |
• Look carefully at the condition of the cornea and the pupil. If the corneal endothelium has significant guttata, as in Fuchs’ Dystrophy, one can make additional efforts to protect the cornea intraoperatively with extra use of a dispersive viscoelastic; you should also counsel the patient preoperatively on the potentially longer time for corneal healing and visual recovery. Additionally, if the pupil shows signs of irregularity and poor dilation, you should plan for the possibility of needing extra steps to achieve pupil expansion intraoperatively.
• Consider adding a MIGS procedure to the cataract surgery. Although this might not make sense for every patient with a tube or bleb, many patients would benefit from additional IOP lowering, as noted above, and studies have confirmed that this can happen when a MIGS procedure is performed after a tube shunt or trabeculectomy.2,3 A MIGS procedure can also help to stabilize eye pressure and limit the possible pressure spikes that can occur following this type of surgery in these patients. In addition, many patients would be grateful for being able to use fewer drops every day, a common benefit of MIGS.
When deciding whether to add a MIGS procedure, three factors are key:
— Is the pressure currently controlled? If not, adding a MIGS procedure makes very good sense.
— If the pressure is under control with medications, how many medi-cations is the patient using? If the number of drops is minimal, there may be less need for adding a MIGS procedure. On the other hand, if the patient is taking multiple drops every day, that’s a good reason to consider the benefit of adding a MIGS procedure.
— Does the eye have at least 180 degrees of viable angle tissue available for the MIGS procedure? Without this condition, many MIGS procedures would be off the table.
In terms of which MIGS to consider, I’ve used various procedures, including goniotomy procedures such as Trabectome, Kahook Dual Blade and gonioscopy-assisted trans-
luminal trabeculotomy, stents (including iStent and Hydrus), canaloplasty such as ABiC with iTrack, and conjunctival stents like the Xen. I’ve seen good eye pressure reduction with all of them. I’ve also had success combining canaloplasty and goniotomy procedures, as in the Omni procedure. In short, you have many options to consider that can potentially help your patient.
• Make sure the patient has realistic expectations. Patients with a pre-existing tube or trab may assume that their cataract surgery outcome will be the same as their friends’ outcomes, when in fact their situation is considerably more complex. (The worst scenario is a patient who’s 20/20 but is still unhappy because he thought the visual difficulties caused by the glaucoma were going to be eliminated by the cataract surgery.)
To avoid an unhappy patient postop, I recommend:
— Always show the patient his or her visual field preoperatively. This helps to drive home the reality that the patient has problems that cataract surgery can’t correct.
— Discuss the possibility that the patient may need fewer glaucoma medications, especially if you’re add-ing a MIGS procedure. This benefit may help offset any dismay the patient feels after learning that the surgery won’t cure the glaucoma.
—Explain that the prior glaucoma surgery could fail. While this may be unlikely, it’s better to warn the patient that it’s within the realm of possibility. Also, be sure to explain that additional steps may be required intraoperatively and postoperatively in the unlikely event that this should occur.
• Choose an appropriate intraocular lens. Factors that should influence your choice include the stage of the disease (especially in terms of the visual field); the condition of the ocular surface; and whether the patient has astigmatism. Many surgeons choose aspheric IOLs for these patients because of contrast sensitivity issues. However, these patients can be candidates for astigmatic correction via a toric IOL or a limbal relaxing incision, especially if they’re interested in reduced spectacle dependence and their glaucoma surgery has been stable for some time.
Because these patients have less-than-perfect visual fields, they’re generally not good candidates for extended-depth-of-focus or multifocal lenses; the glaucomatous damage may be encroaching on central fixation. Monovision should be considered
cautiously in patients who have significant field loss in one or both eyes.
Intraop and Postop
During and after the surgery, these strategies will help ensure a good outcome:
• Use topical drops and intracameral medication for anesthesia. This will avoid the risk of a hemorrhage that’s associated with a retro-bulbar block.
 |
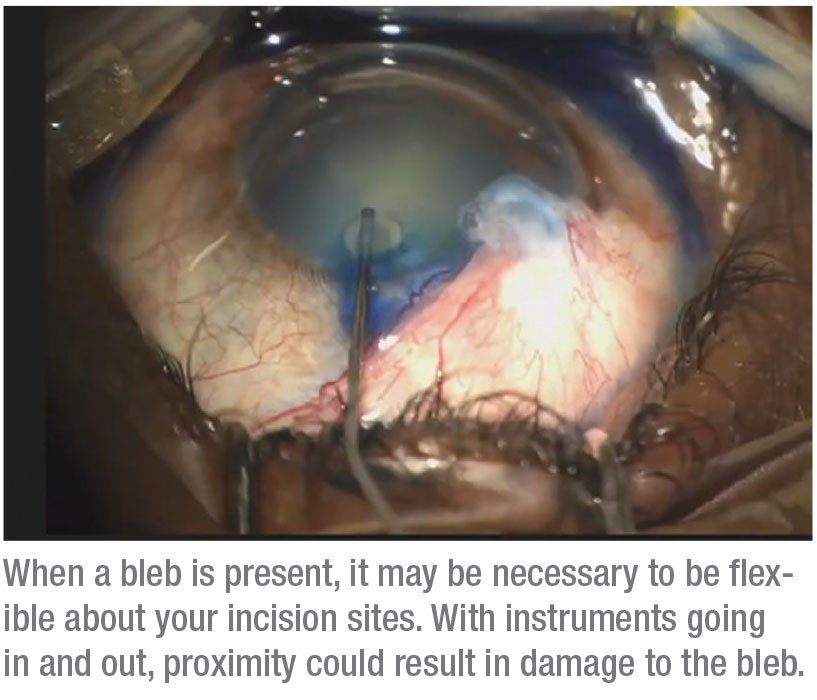
• Be flexible about your incision sites, to avoid the bleb. You’ll be moving instruments in and out of those incisions, so they need to be well away from the bleb to ensure it isn’t inadvertently damaged.
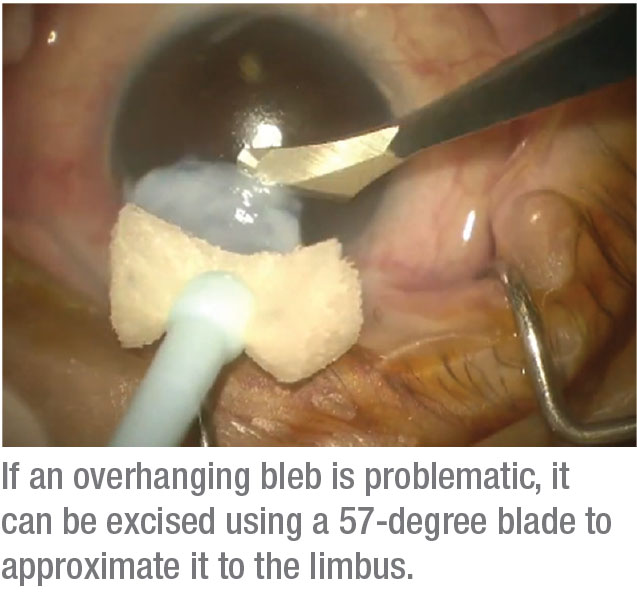
• If an overhanging bleb is interfering with visualization, excise it. Leon Herndon, MD, taught me a simple technique that involves using a 57-degree blade to excise the bleb and approximate it to the limbus. (See picture, right.) Excising the bleb in this manner creates a clean break that allows better visualization both for the cataract surgeon and for the patient postoperatively.
• If a bleb is marginally functioning, consider needling it with or without 5-FU intraoperatively or postoperatively. This approach has been described in the literature, and can be helpful in some patients with marginally-functioning blebs who are being considered for cataract surgery.
• If an existing tube shunt is problematic, consider shortening it. If the tube is long, close to the cornea or pressing against the cataract, you’ll need to shorten it. I sometimes use a Sinskey hook through a paracentesis to stabilize the tube and then use intraocular scissors to cut the tube shorter. I then use Utrata forceps to remove the tube piece from the eye.
If you perform this maneuver, be sure to use copious amounts of Vis-coat to protect the endothelium. Re-apply midway through the procedure if you have any concerns.
• Check the patient frequently after surgery. Be on the lookout for IOP spikes and any sign of a hyphema. Aggressive inflammation control is advisable; that may require the use of low-concentration steroids like loteprednol, as well as increased use of NSAIDs. (I like to use the once-a-day NSAIDS two or three times a day to help reduce the need for steroids.) I also watch for bleb failure and use gonioscopy to monitor for peripheral anterior synechiae formation in the angle with any MIGS procedure.
Staying the Course
Performing cataract surgery on a prior tube or trabeculectomy patient presents challenges beyond those associated with a healthy patient. To address those challenges effectively, devote extra time, thought and preparation to your preop evaluation; make sure you address patient expectations before surgery so that any issues that arise won’t lead the patient to believe you did something wrong; and consider adding a MIGS procedure to the cataract surgery. MIGS procedures can help lower IOP, limit the risk of IOP spikes, reduce the patient’s medication burden and relieve medication-related ocular surface disease.
These strategies should help you achieve the best possible outcomes when working with a patient who has a pre-existing trab or tube, and reduce the likelihood of an unhappy patient postoperatively. REVIEW
Dr. Okeke is an assistant professor of ophthalmology at Eastern Virginia Medical School in Norfolk, and a glaucoma specialist and cataract surgeon at Virginia Eye Consultants. She produces educational glaucoma videos on her iGlaucoma YouTube channel. She is a consultant for Aerie, Alcon Laboratories, Allergan, Bausch + Lomb, Ellex, Glaukos, MST, Novartis, Reichert, Santen, Sight Sciences and Sun Ophthalmics.
1. Swamynathan K, Capistrano AP, Cantor LB, WuDunn D. Effect of temporal corneal phacoemulsification on intraocular pressure in eyes with prior trabeculectomy with an antimetabolite. Ophthalmology 2004;111:4:674-8.
2. Bussel I, Kaplowitz K, Schuman J, Loewen N. Outcomes of ab-interno trabeculectomy with the Trabectome after failed Trabeculectomy. British J Ophth 2015; 99:2:258-262.
3. Mosaed S, Chak G, Haider A, Lin K, Minckler D. Results of Trabectome surgery following failed glaucoma tube shunt implantation: Cohort study. Medicine (Baltimore) 2015; 94:30:e1045.



