This interventional case series included nine patients with bilateral PDR. The nine patients all had a follow-up of at least nine months; five of the patients had 12 months of follow-up. In all nine patients, one eye received intravitreal triamcinolone before PRP (injected eye) and the other, PRP alone (control eye).
The main outcome measures were the change in planimetric area of fluorescein leakage from retinal neovascularization and in central macular thickness on optical coherence tomography at three, six, nine and 12 months. Secondary end points were change in vision, intraocular pressure and cataract progression, according to the researchers.
Initial mean (SD) planimetric area of fluorescein leakage and central macular thickness was 7.22 (5.70) mm2 and 372.11 (91.88) µm in injected eyes, and 9.08 (6.17) mm2 and 355.33 (115.23) µm in control eyes, respectively.
The planimetric area of fluorescein leakage decreased by 86 percent at the nine-month interval and 88 percent at 12 months in injected eyes, and 33 percent and 50 percent, respectively, in controls. Central macular thickness significantly decreased in injected eyes and increased in control eyes; vision slightly improved in injected eyes and worsened in control eyes.
No serious complications occurred in the study. Further studies are needed to assess the efficacy and safety of intravitreal triamcinolone injection as adjunctive treatment to PRP in the treatment of PDR, the researchers say.
The study had a number of limitations, the researchers note, including the relatively small sample size and follow-up period. However, the outcomes noted between the two groups prove the researchers' hypothesis that at least some PDR eyes can benefit from an intravitreal injection of triamcinolone.
(Arch Ophthalmol. 2006;124:643-650)
Bandello F, Polito A, Pognuz DR, Monaco P, Dimastrogiovanni A, Paissios J.
Cup-to-Disc Ratios Differ Among Glaucoma Tests
Measurements of horizontal and vertical cup-to-disc ratios differed significantly across three methods (stereoscopic optic nerve head photographs, confocal scanning laser ophthalmoscopy, and optical coherence tomography) for both glaucomatous and normal eyes, according to a group of Alabama researchers.
For the study, 51 glaucoma patients and 49 control subjects underwent a full ophthalmic examination, including ONHPs, Heidelberg Retina Tomograph (HRT II) scans, and Stratus OCT scans. The intraclass correlation coefficient and Bland Altman plots were used to assess the agreement across the three methods. Repeated measures analysis of variance (ANOVA), Tukey adjustment, and pairwise p values were used to compare the horizontal and vertical cup-to-disc ratio estimates.
The agreement in subjectively assessed HCDR and VCDR was substantial (ICC=0.84 and 0.85, respectively), and for all three methods, overall agreement was good (ICC=0.75 and 0.77 for the HCDR and VCDR, respectively). Stratus OCT provided the largest overall mean +SD: HCDR (0.68 +0.14) and VCDR (0.62 +0.13). The smallest overall mean +SD HCDR was provided by ONHP (0.32 +0.16), and the smallest overall mean +SD VCDR was provided by HRT II (0.26 +0.20). Repeated measures ANOVA test demonstrated significant differences across the three methods for glaucomatous (p=0.0017 and 0.0016, HCDR and VCDR, respectively) and normal (p=0.0001 for both HCDR and VCDR) eyes. Tukey adjustment demonstrated specific statistical differences between pairs of methods.
The researchers say that although the overall agreement between various methods was good, the mean estimates were statistically different. They add that additional studies are needed to evaluate the sources of variability, level of significance, and longitudinal agreement between various methods of the CDR estimation.
(J Glaucoma 2006;15:183-189)
Arthur SN, Aldridge AJ, De León-Ortega J, McGwin G, Xie A, Girkin CA.
Restylane Injections Help Facial Rhytids
Restylane injections are a safe and effective treatment for static wrinkles with a high patient satisfaction rate, according to researchers involved in a multicenter retrospective review.
The researchers studied data from 286 patients treated with Restylane (Medicis Aesthetics, Scottsdale, Ariz.) to review injection techniques and patient satisfaction after the injection in various facial areas. The participants were patients from nine American Society of Ophthalmic Plastic and Reconstructive Surgery practices.
The practices involved in the study performed Restylane injections for an average of 8.8 months; all nine practices injected the nasolabial and melolabial folds and the lips. Six of the nine sites injected the glabella, and two practices injected other fillers concurrently. Botox was injected concurrently by eight of nine practices. Physician-rated patient discomfort was rated 4.6 on average, on a scale of one to 10, with topical anesthesia, and 2.1 with injectable lidocaine, with or without topical anesthesia.
Patient satisfaction on a scale of one to 10 had an average rating of 8.1, compared with that of Botox injection (8.9), upper blepharoplasty (8.9), and collagen injection (6.6). Problematic complications, such as bruising, swelling, bumpiness and redness, each had an incidence of 5 percent or less.
Researchers found injection techniques, volume, end points and anesthesia vary for different facial areas and between different practices. The researchers continue to wait for long-term experience and results from the inclusion of other areas, such as the eyebrows and tear trough.
 |
 |
 |
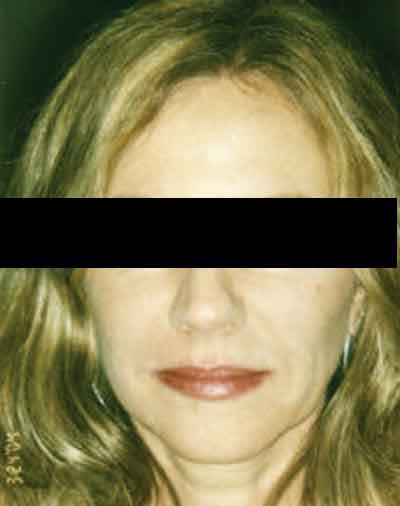
| A female patient before (left) two to three vials of Restylane treatment to the lips, and smile lines between the mouth and cheeks. In the middle image, the patient is seen five minutes post-treatment with makeup. Blue lines indicate treated areas (right). Jemshed Khan, MD |
(Ophthal Plast Reconstr Surg;22: 188-191)
McCracken MS, Khan JA, Wulc AE, Holds JB, Fante RG, Migliori ME, Ebroon DA, Amato MM, Silkiss RZ, Patel BCK.
Postop Bruising Uniform After Bilateral Eyelid Surgery
Although patients frequently perceive asymmetry in healing after bilateral eyelid surgery, a recent study by a group of Massachusetts researchers shows that asymmetry in bruising is actually typically small. The researchers say that since there is little, if any, variation of the procedure between the sides, postop bruising and swelling should be similar on both sides.
The study comprised 19 patients undergoing bilateral ptosis repair, blepharoplasty or both procedures. The patients were provided with questionnaires to determine their perception of the degree of symmetry in healing at four time points after surgery. Researchers used digital imaging analysis to measure the actual amount of bruising present on each side in a separate cohort of 10 patients undergoing bilateral eyelid surgery.
Asymmetry in bruising, swelling, and discomfort was reported by the majority of patients at each time point post-surgery, the researchers report. The number of patients reporting asymmetry peaked at day three postop for all three measures. Objective measurement seven days postop showed half of the patients had more bruising on the right side and half had more bruising on the left. The difference in the average area of bruising between each side was not statistically significant.
(Ophthal Plast Reconstr Surg; 22:266-268)
Hatton MP, Kelley JM, Rubin PAD.




