Here are some of the key results from this year's survey.
Findings
The survey was mailed to 1,500 surgeons, and 167 responded, for an 11 percent response rate.
Refractive lens exchange has become even more popular for the high hyperope (+5 D) and continues to erode the popularity of LASIK for the
+3 D patient. For the high hyperope, 61 percent of surgeons prefer RLE, compared to only 8 percent who say they like LASIK. This is the continuation of a trend in which around 56 percent preferred RLE last year, and only around 42 percent preferred it in 2004. "Waiting" had the second highest percentage of proponents, at 23 percent.
Though LASIK is still the most popular option for the +3 D hyperope, with 66 percent of respondents preferring it, its dominance has been steadily decreasing from its eight-year high of 92 percent in 2002. RLE, conversely, has been on the rise, with the percentage of surgeons choosing it going from just around 10 percent in 2004 to 16 percent this year.
Dr. Duffey says the nature of the hyperopic patient has a lot to do with RLE's popularity in this segment. "Once you get up to 4 and 5 D of hyperopia, the excimer laser just isn't as effective," he says. "And, most of the hyperopes are older patients, so they start getting lens changes that also limit their acuity."
A significant trend has been a movement toward thinner flaps with LASIK, specifically flaps between 120 µm and 130 µm. In 2004, around 46 percent of surgeons chose flaps between 150 µm and 160 µm, and just about 44 percent preferred 120 to 130 µm flaps. In this year's survey, though, only 21 percent chose the thicker flap range, while 53 percent said they use flaps in the thinner range. As for the rest of the surgeons, 20 percent prefer 100-µm flaps, 6 percent like at least 180 µm, and only 1 percent use 80-µm flaps.
"There had been a lot of shying away from thin flaps for various reasons, such as the belief they wrinkled more easily and were prone to complications," says Dr. Duffey. "However, none of that has held true, and people are using them more often now." There are advantages surgeons enjoy with thin flaps, especially leaving a thicker residual bed that both helps lessen the risk of ectasia and leaves more tissue in case an enhancement is necessary. Dr. Duffey thinks that a lot of the better outcomes some surgeons have been experiencing with microkeratome flaps in recent years have been a result of using thin flaps in general, not necessarily from using a particular type of device to make the flaps.
One finding that Dr. Duffey says is interesting is the percentage of surgeons who have had refractive surgery themselves. Nineteen percent have had LASIK, 7 percent have undergone PRK, 3 percent have had limbal relaxing incisions and 3 percent say they've had conductive keratoplasty—32 percent total. "Around a third have had modern refractive surgery done, which doesn't mean radial keratotomy," says Dr. Duffey. "That's a pretty high penetration rate, especially when you consider that only about half of us are eligible for refractive surgery to begin with."
The percentage of surgeons who say they use the IntraLase Pulsion femtosecond laser to make their flaps seems to be leveling out, after posting increases in each of the past surveys. It decreased slightly from around 22 percent last year to 20 percent this year. This finding surprised Dr. Duffey in light of the results of his past surveys. "I thought IntraLase use would have gone way up," he avers. "But, it hasn't changed much on the survey." It still comes in second behind the Bausch & Lomb Hansatome (30 percent). The only other flapmaker in double digits was the AMO Amadeus, with 14 percent of the surgeons saying they prefer it.
As for the preferred residual bed thickness with LASIK, two-thirds of respondents still feel that 250 µm is appropriate. "But, the truth is no one knows," says Dr. Duffey. "However, the thing I find helpful about these surveys is that they provide safety in numbers." He says if someone finds himself in court and has his standard of care called into question, he can point to this survey to show that it's in line with his peers.
Some other interesting findings:
• Ninety-five percent of respondents say they either perform PRK now or plan to do so in the future, a large increase from around 75 percent in 2000. Conversely, only 24 percent say the same about CK, which is down from 44 percent in 2000.
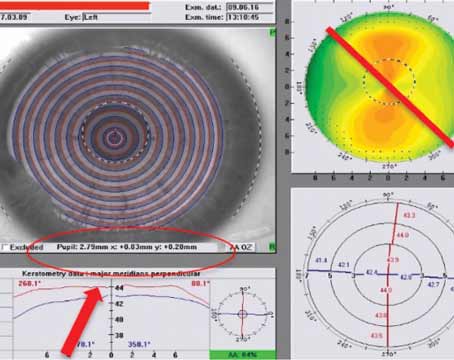
• The Zeiss-Humphrey unit is the most commonly used topographer, chosen by 32 percent of respondents. Twenty-four percent prefer the Orbscan, 12 percent use the EyeSys, 9 percent use the Pentacam, 9 percent use the Nidek OPD-Scan and 7 percent use the Tomey device.
• Refractive surgery monovision is still the overall preferred treatment for presbyopes (42 percent); in terms of the new presbyopic IOLs, the ReSTOR is used by 16 percent of respondents, the ReZoom by 10 percent and the Crystalens by 6 percent.
• The percentage of surgeons who say they use wavefront-guided ablations for 76 to 100 percent of their patients increased to 55 percent from 45 percent last year.
When asked if the survey results sway his practice habits, Dr. Duffey says he often falls on the innovative side of the fence in terms of his practice patterns, but the survey is always good confirmation that he's on the right track. "I tend to stay ahead of the curve by keeping on top of developments in the industry," he says.