|
In October, Alcon’s LenSx femtosecond laser earned a unique distinction by becoming the first laser approved in the United States for LASIK flaps, corneal incisions, anterior capsulotomies and lens fragmentation. This approval gives its users more flexibility in how to use the laser, but also presents them with some tough decisions about how to deploy it effectively in their practices, since cataract procedures are usually performed at a site that’s removed from the LASIK suite. Here’s a look at the new flap creation function of the LenSx, and insights from a surgeon who’s been using it to make flaps.
Making Flaps
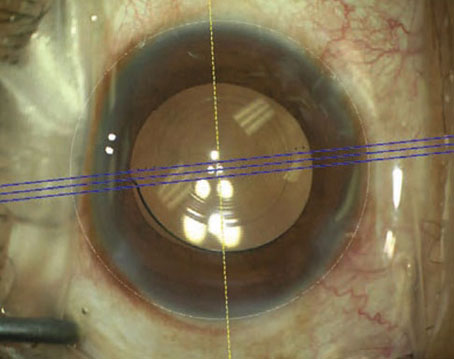
As with any femtosecond procedure, docking is critical for a good outcome. The LenSx uses a disposable patient interface that consists of a curved applanation lens and a suction ring with tubing. The interface sits on the end of the laser arm. To dock with the patient, the surgeon uses the system’s joystick and the video image on the monitor to bring the applanation cone down. The company says an applanation force indicator has been integrated into the system to help the surgeon know when applanation is satisfactory; if the indicator is in the yellow or green zones, the surgeon can apply suction.
“Docking is the same as with LenSx cataract surgery,” says Budapest, Hungary’s Zoltan Nagy, MD, who has used the laser for both LASIK flaps and cataract procedures. “The current patient interface is a bit smaller, and the docking device’s shaft is a bit longer, than what was used previously. Centration is very important in both femtosecond cataract surgery and during the flap creation procedure. We usually use the limbal area as a guide for centration during the LASIK flap procedure, while in cataract surgery we use both the limbal area and the dilated pupil. I know that the company is planning to introduce an automated centration procedure, and I hope to see its availability soon.
“During docking, you can tell when applanation is achieved,” Dr. Nagy continues. “When the patient interface is touching the cornea, a small circle, usually in the center, will be visible. If it’s not, we ask the patient to fixate on the aiming beam and re-dock. It’s usually easy to dock the patient after that. If it doesn’t go well during the first attempt, it’s helpful to calm the patient and inform him that the patient interface will be close to his eye and to not be afraid of it. If you meet the patient before the procedure to reassure him, give enough anesthetic drops and ask him to fixate on the aiming beam, I’ve found the docking procedure isn’t a problem.”
|
Dr. Nagy says he’s currently studying the predictability of flap thicknesses. Though he doesn’t have data from the study just yet, he says, “We checked flap thickness with ultrasound and it was well-correlated with the preset intended thickness. It’s important for a femtosecond laser to create reproducible flaps, and it appears in this case the predictability is accurate.” Alcon says the new flap making capabilities will be added to the laser in 2013.
Thoughts on Logistics
U.S. surgeons excited about the potential of a laser that helps them with both LASIK and cataract surgery are also faced with the challenge of making the laser work logistically, since many don’t perform their refractive procedures and cataract operations in the same place. Dr. Nagy says it may mean a paradigm shift.
“I think it might be a problem for some,” Dr. Nagy says. “They may have to rethink the organization and patient flow of their practices. In my case, I am fortunate that our femtosecond laser’s room is only about five or six meters away from the main OR. I’m lucky that I also had enough room to place the excimer in the room with the LenSx. The LenSx room happens to be a sterile environment, but it doesn’t necessarily need to be, since the cataract wounds don’t open by themselves. So, in practice, if I am performing a LASIK procedure, I just shift the patient bed from the femtosecond laser to the excimer. I do one eye with the femtosecond, perform the refractive treatment, then reposition the flap. I then do the second eye.
“In the case of a cataract procedure,” Dr. Nagy continues, “I use the same room and then walk the patient to the OR. It’s good not having to walk the patient a very long distance because a long distance gives the pupil time to narrow, which makes it difficult to work properly during the cataract procedure. You then have to spend time widening it before surgery. Also, patients have paid a good deal of money for the procedure, and they prefer to have it done within a short time span.”
Dr. Nagy says the placement of the laser depends a lot on the focus of the surgeon’s practice. “The take-home message is that the laser can be either in the main operating theater in sterile conditions, or it can be placed outside in non-sterile, clean-room conditions,” he says. “It depends on which procedure you do more of. If you perform more refractive procedures, it’s probably more useful for you to put it in a clean-room environment. However, if you perform more femtosecond cataract surgeries, it’s advisable to put it in a sterile environment.” REVIEW
Dr. Nagy is a consultant to Alcon.