The goal of the MACRA QPP is to pay for value and better care via two pathways: the Merit-based Incentive Payment System and Alternative Payment Models. The MIPS program combines parts of the Physician Quality Reporting System, the Value Modifier, and the Electronic Health Record incentive programs into one program. MIPS and APMs will go into effect over the next few years, impacting physician payments in 2019.
MIPS
According to a U.S. Department of Health and Human Services press release, most Medicare physicians will initially participate in the QPP through MIPS.2 Consistent with the goals of the new law, the proposed rule would improve the relevancy and depth of Medicare’s quality-based payments and increase physician flexibility by allowing doctors to choose measures and activities appropriate to the type of care they provide. MIPS allows Medicare physicians to be paid for providing high-value care through success in four performance categories: Quality; Advancing Care Information; Clinical Practice Improvement Activities; and Cost.
• Quality will make up 50 percent of a physician’s total score in year one. Ophthalmologists would choose to report six measures from among a range of options that accommodate differences among specialties and practices.
• Advancing Care Information will contribute 25 percent of a physician’s total score in the first year. Ophthalmologists would choose to report customizable measures that reflect how they use technology in their day-to-day practice, with a particular emphasis on interoperability and information exchange. Unlike the existing reporting program, this category wouldn’t require all-or-nothing EHR measurement or redundant quality reporting.
• Clinical Practice Improvement Activities would be 15 percent of the total score in year one. This category would reward clinical practice improvements, such as activities focused on care coordination, beneficiary engagement and patient safety. Ophthalmologists would be able to select activities that match their practices’ goals from a list of more than 90 options.
• Cost would account for 10 percent of a physician’s total score in year one. This score would be based on Medicare claims, which means no reporting requirements for health-care providers. This category would use 40 episode-specific measures to account for differences among specialties.
The purpose of the proposal is to streamline and reduce reporting burden across all four categories, while adding flexibility for practices. CMS would begin measuring performance for physicians and other health-care providers through MIPS in 2017, with payments based on those measures beginning in 2019.
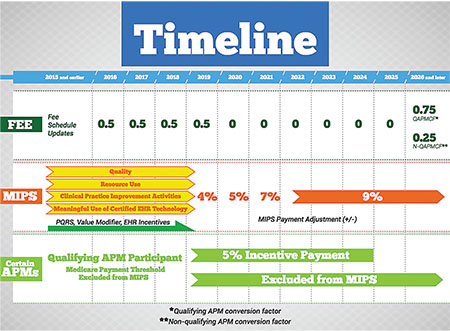 |
| The Quality Payment Program from the Department of Health and Human Services has two paths physicians can follow: The Merit-based Incentive Payment System, in which reimbursement will be based on the four areas in the gold arrows; and the more intensive Advanced Alternative Payment Models, in which physicians belong to entities such as Accountable Care Organizations. The diagram shows the timeline for changes to the fee schedule based on the path taken by the physician. Source: HHS. |
He notes that physician scoring will begin in a few months. “That’s what people are not really up to speed on,” he says. “Ophthalmologists like to be good students, so I think there is going to be frustration with the scoring. Fees can be adjusted ±4 percent in the first year, and that escalates to ±9 percent in the fifth year. It’s designed so that you will have some losers and some winners. There will be some very big winners, and I’m concerned about that.”
According to Donna McCune, CCS-P, COE, CPMA, vice-president of the Corcoran Consulting Group, MACRA was initially good for physicians because it eliminated the Sustainable Growth Rate formula calculation. “This was always flawed and created year-after-year anxiety and angst over what physicians were going to be paid,” she says. “The law itself contains fee-schedule updates, so we know that that is part of the MACRA regulation. The biggest issue is the initiation of MIPS, which is supposed to be implemented as of January 1, 2017. The various components of MIPS and the success or failure of a particular physician or practice will affect their reimbursement rates two years from then, in 2019. All of these programs that are part of MIPS and all of the quality programs that we have been participating in for the past several years always have a two-year look-back. Anything you do in a particular year affects your reimbursement two years later. That has been an issue for some physicians because they don’t realize that what they do this year is going to affect their reimbursement in 2018, or what they did last year will affect their reimbursement in 2017.”
She notes that there is concern about the time frame. There will not be a final ruling on this latest proposal until mid-November, and the implementation date is January 1. “It will be very difficult for practices to be able to pull off a January 1 implementation date with probably only six weeks of notice,” she notes. “Implementation will most likely involve updating and reprogramming EHRs. I personally have concerns about EHR companies being able to update their software programs fast enough to accommodate a January 1 implementation date.”
Additionally, when MACRA eliminated the Sustainable Growth Rate formula approach, it provided for an annual update of 0.5 percent through 2019. “Physicians are realizing that the reimbursement rates are going to pretty much be flat from the Medicare perspective for the next several years, and then go to a 0-percent update in 2020 through 2025,” Ms. McCune avers. “The only way for physicians to increase their Medicare reimbursement is by being successful with this new MIPS program and potentially qualifying for some bonus money. This could be a problem because the costs of running a practice continue to increase year after year. Another concern is that commercial payers tend to follow Medicare’s lead, with regard to increasing reimbursement rates.”
In the past, physicians were paid based on what they did. They saw a patient, submitted a claim, and were paid. “The purpose of these programs is to eliminate the traditional fee-for-service and have a component of a visit or a service provided be fee-for-service, and then link the rest of the payment to quality. So, the existing model that we have had forever is gone,” Ms. McCune adds.
APMs
Increasing numbers of Medicare clinicians are participating in alternative payment models, and MACRA has created additional rewards for physicians who choose this path. According to the U.S. Department of Health and Human Services,2 Medicare clinicians who participate to a sufficient extent in Advanced Alternative Payment Models would be exempt from MIPS reporting requirements and would qualify for financial bonuses. These models include the new Comprehensive Primary Care Plus model, the Next Generation ACO model and other Alternative Payment Models under which clinicians accept both risk and reward for providing coordinated, high-quality care.
However, many physicians who participate to some extent in Alternative Payment Models may not meet the law’s requirements for sufficient participation in the most advanced models. The proposed rule is designed to give these health-care providers some benefits within MIPS, as well as to make it easy for physicians to switch between the components of the QPP based on what works best for them and their patients.
The U.S. Department of Health and Human Services expects the number of clinicians who qualify to participate in Advanced Alternative Payment Models to grow as the program matures.
Global Services Data Collection
Another concern is that Section 523 of MACRA requires CMS to develop and implement a process to gather and analyze the necessary data on preoperative and postoperative visits and other services furnished during global surgical periods other than the surgical procedure itself. CMS recently released a draft proposal to collect data on global surgery codes, which represent about half of all physician-provided services under Medicare. The concern is that, if adopted, the proposal could direct more provider resources toward reporting compliance and away from patient care. CMS is proposing to collect data for all 10- and 90-day global services from every physician who provides these services, rather than from a sample of physicians, as Congress intended under MACRA. Specifically, physicians would be required to report information on every 10-minute increment of care provided before and after each procedure in the hospital, office, or via e-mail or phone, and whether the services were provided by them or their staff.
“If the proposal goes through as planned, it means that, for every postoperative visit, the physician will be scoring the level of complexity of the visit plus the level of complexity for the tech involvement, plus the number of minutes in 10-minute increments. I don’t know if doctors will spend the time to do it correctly or if they will forget to do it,” Dr. Repka says.
The AAO is opposed to this initiative because it’s too broad and inconsistent with what Congress intended when it forced CMS to restore global payments for surgical services last year and study the issue.
According to AAO Health Policy Committee Associate Secretary David B. Glasser, MD, this data collection requirement will affect daily patient care. “Surgeons would be required to keep track of their postop care time in 10-minute increments and report multiples of each postoperative visit code based on time. Literally, this would take a stopwatch. There are approximately 4,200 codes with 10- and 90-day global payments. This would have to be done for every one of these codes, regardless of whether they are frequent or major-dollar codes. The complexity of learning to use the new codes and the data collection burden would guarantee an underestimation of the number of postoperative visits and the time spent delivering postoperative care.” REVIEW
1. www.cms.gov
2. http://www.hhs.gov/about/news/2016/04/27/administration-takes-first-step-implement-legislation-modernizing-how-medicare-pays-physicians.html



