NOW THAT CONDUCIVE KERATOPLASTY has been around for several years, experts say they've learned much about getting the best outcomes with it in presbyopic patients, and fitting it into their practice. In particular, surgeons are excited about a new technique for delivering NearVision CK energy that some say has changed the face of the procedure. Here, several CK veterans share their insights.
|
|
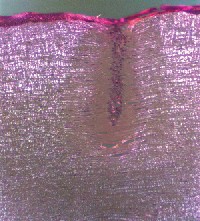
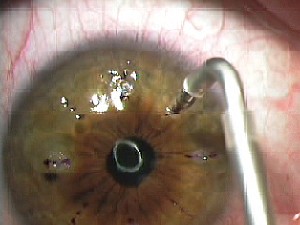
| A discrete, discernible ink mark is crucial to properly center the CK procedure. |
The Right Patient
"The plano presbyope represents the so-called 'sweet-spot' patient for CK," says Brookville, Pa., surgeon Louis D. "Skip" Nichamin. "We initially bridled back on how much pre-existing hyperopia we would tackle. The procedure was originally approved for 3 D, but we found anything over 1.5 D to be a little iffy, so the plano presbyope was ideal." Since the introduction of the light-touch technique, discussed below, Dr. Nichamin says surgeons have gone back up on their treatment range.
Overland Park, Kan., surgeon Dan Durrie says CK is also useful in two other patient groups: post-PRK or post-LASIK patients who have become presbyopic and post-cataract patients who are frustrated with their reading glasses.
"Taken together," says Dr. Durrie, "these groups make up the largest single group of patients seeking refractive surgery, by far."
Since NearVision CK is basically an induction of myopia in a patient's non-dominant eye, surgeons make sure their patients can handle this before performing the procedure. They have a couple ways to do this.
"A certain number of patients will come in and say that they've tried monovision contacts and love them, but their eyes get too dry to wear them," says New Orleans surgeon Marguerite McDonald. "So, of course, for these people you can go right ahead and perform CK."
For the other plano presbyopes with no monovision experience, surgeons say you can use the loose-lens test devised by Texas surgeon Glenn Strauss. In the test, which takes about four minutes, you hold three or four plus lenses in succession in front of the patient's non-dominant eye until he can read J3. The lenses' powers should match the treatment outcomes of CK, such as +0.75 D, +1.75 D, etc. "Usually we're going for J3," says Dr. McDonald. "Many people end up with J2 or J1, but we're trying to get people at least to J3 because that's 'social vision.' The average newspaper is J5, so if they can read J3, that means that, under most lighting conditions, they can read the paper for a while, see who's calling them on their cell phone, and read most restaurant menus and store price tags."
Though some experts rely solely on the loose-lens test, there are still others who will do a monovision contact-lens trial for patients who are on the fence. Dr. Nichamin will usually perform a contact-lens trial in the office, but, if the patient isn't sure about it, will let him or her wear the lenses for a few days or a week. The contact-lens trial isn't foolproof, though.
"The problem is that the monovision contact lenses are nowhere near as good as CK," says Dr. McDonald. "There will be some patients who would have tolerated CK, but didn't like the contacts. The reason is that 85 percent of CK patients have no loss of distance vision, and the other 15 percent have only a slight decrease in their distance acuity. With the monovision lenses, though, there's a significant decrease in distance vision as part of the trade-off."
The Low-Pressure Approach
Probably the most influential change in the way surgeons perform CK is the light-touch technique, developed by Columbia, S.C., surgeon H.L. "Rick" Milne.
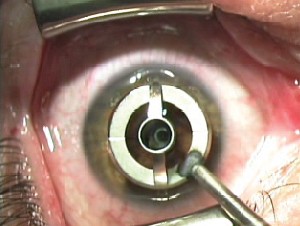
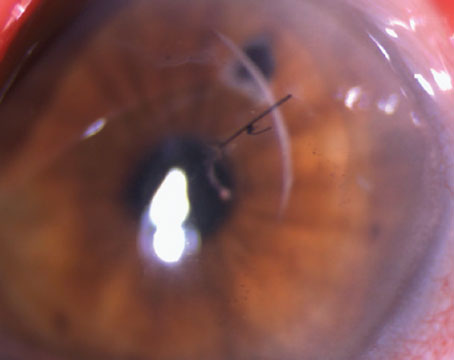
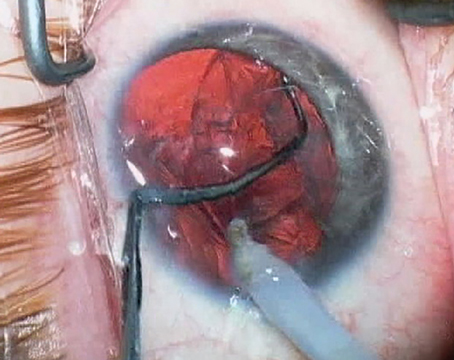
As Dr. Milne explains it, if a surgeon were to press too hard on the CK probe as it delivers its energy, this would push corneal tissue away from the probe. This pushing force actually fights against the probe's energy, which causes the tissue to contract toward the probe. By pressing just enough for the probe to be seated in the cornea, which makes about a 1-mm dimple, surgeons seem to be able to achieve more effect per treatment spot than with the standard CK method, which involves using more force.
"Light touch has two components," explains Dr. Milne. "First, you have to make sure the 450-µm long probe tip is fully seated in the cornea before delivery of a pulse. Second, the probe has to remain seated during the pulse, because the tissue will want to pull away from the probe posteriorly as you indent. The surgeon has to make sure he doesn't indent the cornea too much to cause mechanical stretch of the fibers."
 |
| Light-touch CK involves making only about a 1-mm dimple as the energy is delivered. |
"If you're just barely making a dimple as you hit the footpedal, then the cornea is in its natural state and is capable of shrinking maximally," says Dr. McDonald. "This confers great advantages: greater predictability; less induced astigmatism; greater clinical effect; more space for retreatments; greater patient comfort afterward since there are fewer spots; and faster visual recovery."
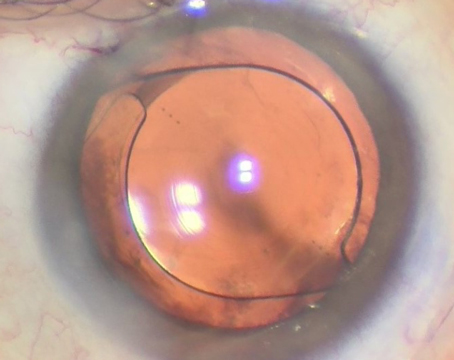
The most popular treatment approach involves using the light-touch technique to make eight spots at the 7- or 7.5-mm zone. Eight spots at
7 mm yields about 1.75 D of effect, a diopter more than it used to with the standard CK protocol. At 7.5 mm, it will yield a little less.
The most popular treatment approach involves using the light-touch technique to make eight spots at the 7- or 7.5-mm zone. Eight spots at
7 mm yields about 1.75 D of effect, a diopter more than it used to with the standard CK protocol. At 7.5 mm, it will yield a little less.
| Table 1. Light-Touch CK Effects |
| Spot Pattern Effect |
| 8 spots at 8 mm 1 D |
| 8 spots at 7 mm 1.75 D |
| 8 spots at 8 mm and 8 spots at 7 mm (16 total) 2.5 D |
| 8 spots at 7 mm and 8 spots at 6 mm (16 total) 3.5 D |
In addition to the light-touch method, Dr. McDonald also recommends making sure your operating microscope is perpendicular to the floor, because this helps ensure the probe is perpendicular to the cornea when it's used. "Most of us who do CK have put a tiny carpenter's level on the microscope head, and check it all the time to make sure we or the cleaners who come in at night haven't knocked it out of position," she says. "That's a huge help."
The Results
Following are the main CK outcomes surgeons are focused on:
• Vision. "You don't really measure CK's outcomes as you do for myopia surgery," says Dr. Durrie. "You don't ask, 'What percentage is J2 for near?' You have to ask what percentage are glasses-free in restaurants, at the store when they're looking at price tags, at home on the computer or when looking up a phone number."