In the United States, managing and minimizing cylinder during phakic intraocular lens implantation can sometimes be an issue, since the currently approved lens, AMO's Verisyse (the "Artisan" outside of the United States), needs to be implanted through a relatively large 5.2- or 6.2-mm incision. In this article, surgeons experienced in phakic lens implantation share their tips for making sure cylinder isn't a problem.
According to Minneapolis surgeon and Verisyse course instructor Elizabeth Davis, in the U.S. Food and Drug Administration study, 2.4 percent of 492 Verisyse eyes had refractive cylinder changes greater than 2 D from preop at one year, 2 percent had such changes at two years (N=355), and 3.5 percent had them at three years (N=226).
Dr. Davis says incision location and suture tension play large parts in inducing or managing astigmatism. "You could induce 3 to 4 D of astigmatism with a Verisyse incision if you really tightened the sutures," she explains. "In general, in the early postoperative period, I get 1 or 1.5 D of induced, with-the-rule astigmatism with the sutures. A lot of this spontaneously decreases in the first couple of weeks. And, the rest will be reduced when I remove the sutures." Her incision of choice is limbal, and she says she tries to make her 10-0 nylon sutures adequately tight, so the wound is approximated and not leaking, but not so tight as to induce astigmatism.
Barcelona surgeon Jose Guell, who also has years of Verisyse/Artisan experience, makes his incision farther back, in the posterior side of the surgical limbus in a superior position. "I like to use a very posterior, bleeding, corneal incision," he says. "This is a two-plane incision. The first, more external plane, is directed toward the posterior part of the sclera. The second plane goes inside the eye, meaning the incision has a cuneiform shape."
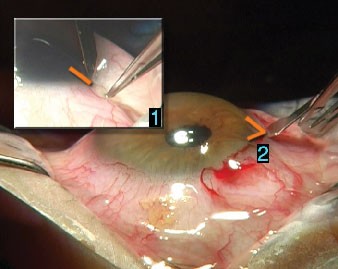 |
| The two steps of Jose Guell, MD's Verisyse incision: 1. The first incision plane is directed toward the posterior sclera. 2. The second plane goes inside the eye, giving the incision a cuneiform shape as depicted by the lines. |
"Our eight years of experience with this incision have proved that it's astigmatically neutral," he avers. As evidence of this, he points to his study of 26 eyes of 18 patients who received both an Artisan and LASIK. In the study, the mean pre-IOL astigmatism was -1.35 D. After Artisan implantation but before LASIK, the mean cylinder was -1.15 D.1
If you don't want to place five or six sutures, but still want to remain astigmatically neutral, Asim Piracha, MD, of Jeffersonville, Ind., says he gets good outcomes using a suture technique he learned during his corneal fellowship under Edward Holland, MD, director of the cornea and external disease service at the Cincinnati Eye Institute.
"After the lens is enclavated, I put one suture in the middle of the incision, then irrigate out the viscoelastic, fill the eye with BSS and put two additional sutures in, using adjustable slip-knot sutures," he explains. "I then reconstitute the anterior chamber with BSS, so it becomes deep. I tie off the sutures with the deep chamber. This is effective because if the eye is soft when you suture it, you'll end up making a tighter wound than if you suture it while the chamber is deep." He says he has yet to do a post-Verisyse LASIK procedure to treat a purely cylindrical error.
Managing Pre-existing Cylinder
In addition to minimizing induced astigmatism, surgeons say you can use such elements as the phakic-lens incision and your sutures to treat pre-existing astigmatism, too. Here are several aspects of the surgery you can use to treat the cylinder:
• Incision options. "If the patient has about 1.5 D or more of astigmatism, I'll place the Verisyse entry incision on the steep axis, and place the lens at 90 degrees away from that, be it horizontal or vertical," explains Dr. Piracha. "I'll combine that with a limbal relaxing incision on the meridian opposite the incision, based on the LRI nomogram of Louis Nichamin, MD." As an example, he says if he had a 30-year-old with 2 D of cylinder, he'd make a 60-degree LRI. He estimates he can treat up to about 2 D with a relaxing incision. If the patient has 2.5 D or more, he'll plan on doing a LASIK down the road.
Dr. Davis says that, in a sub-study of 15 Verisyse eyes (mean cylinder:
-3.43 D) in the U.S. trial who had more astigmatism than the 2.5 D allowed in the trial, Manhattan surgeon Gregory Pamel got an average of 2 D of reduction in cylinder by operating on-axis. Dr. Davis also notes that there is more effect on the cylinder the closer you move toward the visual axis with your incision.
• Sutures. In comparison to placing incisions or doing LASIK postop, adjusting suture tension is more art than science, with surgeons often recommending that the sutures should be just tight enough, but not too tight.
"If you're operating on the steep axis," says Dr. Davis, "and you want to reduce the astigmatism, then you don't want to have really tight sutures. You just make your incision to relax the cylinder, then place sutures that approximate the wound so it won't leak, without making them overly tight so as to induce astigmatism … It's not 100-percent predictable, but I think that, with experience, surgeons get an idea of how tight is tight enough to seal the incision without inducing cylindrical change."
• Postop refractive procedures. Surgeons will also incorporate some refractive procedure into their plan, and some will make it their primary way of correcting any post-implantation refractive error.
"From my point of view," says Dr. Guell, "which isn't the same as all surgeons', the best approach is a two-step surgery. First, implant the phakic IOL. Then, wait for two consecutive, stable refractions, separated by at least four weeks, and proceed with your favorite refractive surgical procedure. This could be astigmatic keratotomy, surface ablation or LASIK.
"I think it's much better to wait several weeks after phakic IOL implantation to proceed with corneal refractive surgery than to do a refractive procedure at the time of lens implantation because the former approach is more predictable. This is the same for pseudophakic IOLs, as well."
Dr. Guell notes that, in some high ammetropic patients with astigmatism, the surgeon may be dealing with a case of frank keratoconus or form fruste keratoconus. In such a case, in order to correct the residual ammetropia and "perhaps" stabilize the cone progression he says the surgeon may want to use intrastromal rings in lieu of another refractive procedure that could weaken the cornea.
Dr. Piracha likes to wait as long as possible before doing LASIK post-Verisyse. "If the patient is comfortable with a three-month wait, I'll wait four," he says. "If he's really pushing me and the refraction is stable, then I'll do the LASIK at three months."
AK is also a possible option in the few cases who have some astigmatism but a plano spherical equivalent after lens implantation, says Dr. Piracha. "AK is a low-cost, in-office option for surgeons who may be more comfortable doing incisional surgery," he says. "The AK will cause coupling, where flattening of the cornea vertically will lead to equal steepening horizontally."
In the end, though, many surgeons like LASIK the best for treating residual refractive error. Dr. Davis says, "Personally, I like the precision of LASIK, and it allows me to treat any residual myopia or hyperopia in addition to astigmatism."
1. Guell JL, Vazquez M, Gris O. Adjustable refractive surgery: 6-mm Artisan lens plus laser in situ keratomileusis for the correction of high myopia. Ophthalmology 2001;108:945-952.