Intrastromal ablation, in which the epithelium is untouched and all the refractive change comes from ablation within the corneal layers, long embodied the ultimate goals of laser refractive surgery: Correct the error and avoid wound healing. Surgeons are closing in on those goals with their use of the Technolas Femtosecond Laser System (Technolas Per-fect Vision,
Intracor Overview
Colombian surgeon Luis Ruiz was the first surgeon to perform the Intracor procedure, and is one of the co-inventors of the procedure along with researchers at Technolas Perfect Vision. "What I like the most about the procedure is how stable it is over time," says Dr. Ruiz.
To perform the procedure, the surgeon enters the patient's keratometry, refraction and corneal thickness data into the laser's computer. As in all refractive surgeries, centration is key to good outcomes, but it wasn't always easy to get. "Centration is quite important," says Dr. Ruiz. "If you didn't have a lot of experience, in the beginning you may have had to place and remove the suction ring several times. But now the system has software to assist you. We put a mark on the center of the cornea, either on the visual axis or in the center of the pupil. Then, once you apply the laser's interface, you can, with software, move the center of the ablation to align with the mark you made. You can recenter it up to 500 µm."
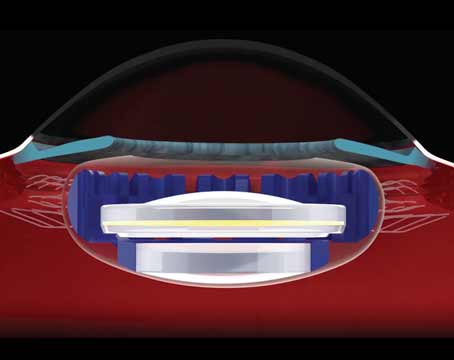
The laser uses a proprietary, curved patient interface to fixate the device. As the company describes it, the interface is a sterile, disposable contact lens that is fixated on the eye with a suction ring. Since the contact lens is curved, the company says the lens helps the cornea maintain its natural curvature, rather than causing it to flatten with fixation. The energy pulses are delivered at a wavelength of 1,053 ±10 nm, with a maximum energy level of 6 µJ.
To treat emmetropic, or slightly hyperopic, presbyopia, the laser creates a series of cylindrical rings, starting in posterior stroma, coming forward through mid-stroma, and stopping in the anterior cornea. This ablation steepens the anterior corneal surface, creating a multifocal hyperprolate shape. According to one study, the variable refractive power of the central cornea improves the eye's depth of focus, which enhances near vision, but also does a good job at preserving distance vision.1 The surgeon adds radial intrastromal ablations in cases of low myopia or astigmatism, though the effects of these are limited. The nomogram for the radial disruptions is proprietary, but Dr. Ruiz says it can vary between 10 and 20 "incisions" depending on the amount of desired effect, corneal curvature, age and other factors. "We haven't been able to correct more than 0.75 D of myopia combined with presbyopic surgery," explains Dr. Ruiz. "In many of these myopic-presbyopia cases, we do PRK first for the myopia and then the presbyopic Intracor procedure three or four months later. With that, we've been able to correct up to 2.5 to 3 D of myopia combined with presbyopia."
Intracor Results
In a study of 245 Intracor procedures Dr. Ruiz performed at his practice, (184 of which reached the one-year follow-up) the average distance vision at 12 months was 1.00 (Snellen: 20/20) and the average near vision was just under J1. Distance-corrected near vision was J1 at 12 months. Overall, 97.8 percent see both 20/25 or better and J3 or better at one year. "Some patients are out of this range," says Dr. Ruiz. "This is because they have some minor myopia and see a little less at distance, maybe 20/30."
In terms of stability, in the 245-eye study, there was a small myopic shift of -0.1 D between one and 24 months. Ninety-five percent of patients are within 0.5 D of the target refraction at one year. As far as safety goes, at six months 2 to 3 percent of patients lost one or more lines, but at one year, only 1 percent had lost one line or more. "At three years, no one has lost any lines," avers Dr. Ruiz, "but there are only 20 eyes at that point. I consider the one-year safety results to be the most representative group."
"Basically, from the first day, we have the final result," says Dr. Ruiz. "At this moment, we're analyzing our results very carefully, because, as with every technique, some patients are underperformers, some are overperformers and some perform normally.
We've been analyzing the preop asphericity of the cornea and corneal shape factors and are finding a very good correlation between these factors and the predictability of the surgery. This means that, in the near future, everyone will have the opportunity to have the very best possible corneal shape postop."
All of the patients report halos after surgery, especially in dark conditions, but many don't have trouble driving at night because of them.1 "If you ask the patients about halo at night, they say, 'Yes, but they don't bother me at night,' " says Dr. Ruiz. "In general, they don't complain about it. They may have them for six to eight months." Near vision is also reduced somewhat in dim lighting due to the dilated pupil undermining the benefit of the hyperprolate cornea.1
The enhancement rate was high for patients in the beginning, but Dr. Ruiz says his and other researchers' investigations into the factors that increase predictability are reducing the need for enhancements. "If you want to select the patients who will do really well—those patients from
Though Intracor is focusing on treating presbyopia at the moment, Dr. Ruiz thinks refractive surgery will eventually move in the direction of intrastromal procedures. "In the near future, probably all femtosecond laser companies will be doing this," he muses.
"With these intrastromal procedures, you don't touch the cornea and you don't have healing problems, a wound or a risk for infection."
1. Ruiz LA, Cepeda LM, Fuentes VC. Intrastromal correction of presbyopia using a femtosecond laser system. J Refract Surg 2009;25:847-54.