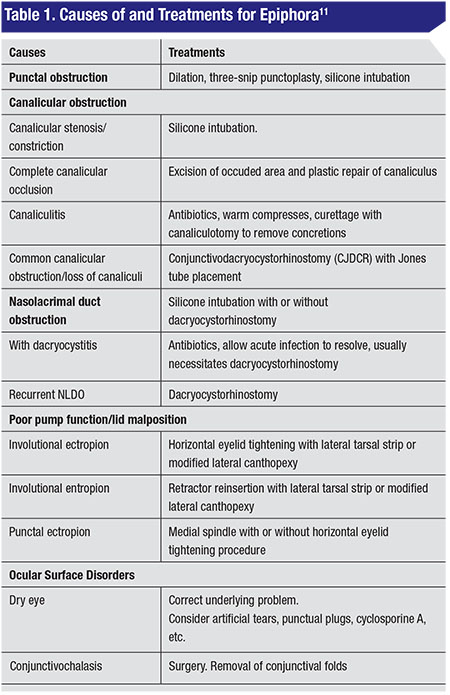
Causes of Epiphora
Though most cases of epiphora are due to non-patency in the lacrimal outflow pathway, others, such as eyelid and adnexal disorders, and corneal and ocular surface pathologies, can also cause watering.1
It’s important, then, to distinguish between the terms epiphora and pseudo-epiphora or hyperlacrimation.1 True epiphora refers to watering due to obstruction in the lacrimal outflow pathway, while hyperlacrimation refers to excessive watering due to irritation of the corneal surface, as in cases of dry eye, corneal abrasion or corneal foreign body.2
Obstructions of the excretory lacrimal system can be either anatomical (referring to any structural pathology in the lacrimal outflow pathway that obstructs tear passage) or functional (where the lacrimal outflow pathway is anatomically normal with a patent syringing, but there’s a failure of the lacrimal pump mechanism elsewhere).2
Pertinent Anatomy
The lacrimal system is divided into the secretory (tear production) and the excretory apparatus (where tears are drained from the eye into the lacrimal sac). Tears are produced by the main and accessory lacrimal glands. Tear quantity and composition are subject to regulatory control and may depend on weather conditions, as well as a healthy eyelid and ocular surface.
 |
Spontaneous blinking (occurring at an average rate of eight to 12 per minute) also plays an important role in tear drainage. Eyelid closure begins at the lateral canthus in order to bring tears into the lacrimal drainage system. During this action, the inferior eyelid is displaced 0.5 mm more medially than the upper eyelid, so that the superior and inferior lacrimal puncta can get in touch. Once the tears are in the punctum and canaliculi, a pumping mechanism caused by the contraction of the palpebral orbicularis oculi muscle (particularly Horner’s muscle) over the lacrimal sac helps to drain the tears into the inferior meatus.4-5 For this reason, it’s very important to evaluate the anatomy and physiology of the patient’s eyelids during your exam, as laxity or malposition may be responsible for tearing.
Contrary to previously held beliefs, recent studies using high-speed video showed that the central portions of the upper and lower eyelids don’t touch during spontaneous blinking.6
Diagnosis
As mentioned earlier, tearing is multifactorial. Ophthalmologists need to differentiate tearing due to an excessive production of tears from tearing that results from an altered excretory system.
 |
| Figure 1A (top). Patient with epiphora. It’s important to evaluate the position of the eyelids and lacrimal punctum, the aspect of the meibomian glands and eyelashes, as well as the presence of blepharitis and trichiasis (Figure 1B, bottom). |
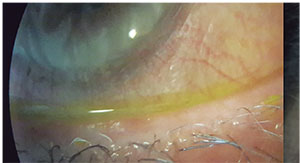
During the slit lamp examination it’s important to document the position and size of the lacrimal punctum, the height of the tear meniscus, evaluation of the eyelid margin (position, aspect of the meibomian glands, presence of trichiasis-distichiasis, blepharitis, etc.) and conjunctivochalasis. (See Figure 1) In addition, mucus secretion or blood in the tear film may indicate infection or malignancy, respectively. Laxity of the eyelids decreases the pump mechanism, so the snap-back and pinch tests have to be performed. (See Figure 2) Sometimes, using a skin tape in the office to simulate the effect of a lateral canthoplasty in the tearing patient may help to diagnose epiphora due to eyelid laxity.
Irrigation of the patient’s lacrimal system will help the clinician determine the site of obstruction. You should suspect canalicular obstruction when you notice clear solution from any of the canaliculi while you’re irrigating, but if regurgitation appears as a mucous secretion, diagnosis is a nasolacrimal duct obstruction. Some patients, however, may complain of a watery eye without any ocular or eyelid abnormality and with a patent lacrimal system during irrigation. This presentation is an entity known as functional epiphora.
Schirmer’s tests 1 and 2,8 tear breakup time,9 ocular surface staining and tear meniscus height are some tests that help to highlight associated ocular surface abnormalities. (See Figure 3) The dye disappearance test is useful for differentiating hyperlacrimation from lacrimal drainage obstruction (whether functional or anatomical). In this
 |
| Figure 2. Eyelid laxity decreases the pump mechanism for lacrimal drainage. The snap back and pinch tests are very useful for determining whether this is the problem. |
Etiology and Treatments
An awareness of the exact cause of the patient’s epiphora will allow you to select the right treatment. Here are the main etiologies to be aware of:
• Punctal stenosis. Punctal stenosis is a common cause of epiphora. It can be congenital, or acquired from infectious and inflammatory eyelid disorders, ocular surface disease, systemic or topical medications (antiviral, anti-glaucoma or anti-neoplastic medications), eyelid tumors or trauma.11-13 It can appear as an isolated disorder or associated with canalicular stenosis, eyelid laxity or malposition. Also, tissue atrophy and involutional changes can cause the dense fibrotic structures of the punctum to be less resilient and the surrounding orbicularis fibers to become atonic, resulting in punctal stenosis.14 (See Figure 5)
The basic principles in the treatment of punctal stenosis include creating an adequate opening while maintaining the position of the punctum against the lacrimal lake and preserving the lacrimal pump function.15-16
Repeated dilation of the stenotic punctum is a simple procedure that may provide temporary improvement in the patient’s symptoms, but recurrences of stenosis are common unless additional procedures are performed.16
Different methods of punctoplasty have been used to augment punctal size, but the two-snip and three-snip punctoplasties have the best outcome. For recalcitrant cases, silicone intubation can be an effective method to help keep the punctum
 |
| Figure 3. Schirmer’s test 2 (with anesthetic). |
• Canalicular stenosis. The frequency of canalicular obstruction has been reported to be between 16 and 25 percent in patients with epiphora. The most common symptom is intermittent or constant tearing. Canalicular obstructions can be anatomically classified as: proximal with involvement of the proximal 2 to 3 mm; mid-canalicular obstructions 3 to 8 mm from the punctum; and distal obstructions as defined by a membrane at the opening of the common canaliculus to the lacrimal sac.18
There are three types of canalicular stenosis: congenital; acquired; and involutional. Many causes have been associated with acquired canalicular stenosis, such as:
• inflammation, specifically blepharitis, canaliculitis, infection, ocular cicatricial pemphigoid, Stevens-Johnson syndrome, trachoma and ectropion;
• traumatic injury to the canaliculus, as in lacerations, chemical burns, thermal burns and radiotherapy;
• drug-induced, by medications such as docetaxel, paclitaxel, pilocarpine, timolol, dorzolamide, idoxuridine, trifluridine, fluorouracil, echothiophate iodide, dipivefrin, betaxolol, mitomycin-C, isotretinoin and verteporfin;
• systemic diseases, such as neoplasms, lichen planus and inflammatory bowel disease; and
• iatrogenic due to punctal plugs, cauterization, surgery, longstanding intubation or radiotherapy.19
The underlying causes of canalicular obstruction must be determined and addressed, as well as the site and extent of stenosis.18
One-snip punctoplasty and canalicular intubation (Mini Monoka) is a simple and effective method
 |
| Figure 4. Dye disappearance test to differentiate hyperlacrimation from lacrimal drainage obstruction. |
• Canaliculitis. Canalicular obstruction caused by a dacryolith often causes pain, redness, purulent discharge and intermittent tearing. Dacryoliths are usually associated with Actinomyces israelii or Candida. Patients under chronic topical medication with epinephrine are more prone to the formation of liths.
Treatment in the acute phase of canaliculitis primarily consists of a course of antibiotics and warm compresses. If obstruction doesn’t clear with those interventions, a curettage with canaliculectomy and drainage of the dacryoliths with antibiotic irrigation of the lacrimal system may be required. Some authors advocate using silicon intubation at the same time but, personally, we don’t think it is necessary.
• Partial and functional nasolacrimal duct obstruction. Functional NLD, by definition, is epiphora without a detectable lacrimal drainage system obstruction. The term “functional obstruction” is confusing, as it implies anatomically patent lacrimal passages with a physiological dysfunction.19
Different
 |
| Figure 5. Stenosis of the lacrimal punctum. |
Management options for partial nasolacrimal duct obstruction include dacryocystorhinostomy, balloon catheter dilation with or without silicone intubation, silicone intubation (monocanalicular, bicanalicular, double bicanalicular) and probing.21 We highly recommend bicanalicular intubation with silicon rods for these patients. We usually leave the tubes in position for three to four months.
The caruncle and bulbar conjunctiva can mechanically occlude the entrance to the lacrimal drainage system. Some patients with true epiphora due to functional lacrimal drainage obstruction have presented with enlarged caruncles. Studies have shown, however, that a carunculectomy can alleviate epiphora in 77 percent of these patients.
Also worth noting is that a case of bulbar conjunctivochalasis occluding the lower punctum must be treated.22-23
• Dacryocystitis. Lacrimal drainage obstruction at the union of the lacrimal sac and the nasolacrimal duct causes fluid to stagnate, with consequent tearing and mucous secretion.
 |
| Figure 6. A young patient with acute dacryocystitis on the right side. |
Once the acute phase of dacyrocystitis has been controlled, there is no recommended subsequent treatment other than a dacryocystorhinostomy, which can be performed via the traditional (external or transcutaneous) or the internal (endonasal) approach. The objective of this procedure is to create an anastomosis between the lacrimal sac and the nose, through a bony opening (10 to 15 mm) at the lacrimal bone. Success rates vary from 70 to 90 percent in different series. Usually, the surgeon stents the canaliculi, though it’s been proven that this may not increase the success rate.
Though getting to the bottom of a patient’s epiphora complaint can be a diagnostic challenge due to the multifactorial nature of the condition, a pertinent history, thorough examination and appropriate testing will help you pinpoint the cause—and the proper treatment—as quickly as possible.10 REVIEW
Dr. Canales is the director of the Orbit and Oculofacial Plastic Surgery Department at the Instituto de Oftalmología Fundación de Asistencia Privada Conde de Valenciana I.A.P.
Dr. Morales is an ophthalmologist in the Orbit and Oculofacial Plastic Surgery Department, and Dr. Velasco y Levy is currently a fellow at that institution.
1. S.Das,MS; Evaluation of epiphora; Principles and Practice of Lacrimal Surgery, Ed. M. Javed Ali, Springer India 2015
2. Hurwitz JJ. The lacrimal system. Philadelphia: Lippincott-Raven Publishers: 1996
3. Basic and Clinical course. Section 7, Orbit, Eyelids and Lacrimal System. American Academy of Opthalmology. 2008-2009:259-64.
4. Meyer-Rüsenberg HW, Emmerich K. Modern lacrimal duct surgery from the Ophthalmological perspective. Dtsch ArzteblInt 2010;107:14:254-8
5. Tucker NA, Tucker SM, Linberg JV. The anatomy of the common canaliculus. Arch Ophthalmol. 1996;114:1231-4.
6. Paulsen F, Thale A, Schaudig U: Ableitende Tränenwege und trock- enes Auge. Ophthalmologe 2002; 99:566-74.
7. Paulsen F: Anatomie und Physiologie der ableitenden Tränenwege. Ophthalmologe 2008;105:339-45.
8. Munk PL, Lin DT, Morris DC. Epiphora: Treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology 1990;177:687
9. Kashkouli MB, Pakdel F, Amani A, Asefi M, Aghai GH, Falavarjani KG. A modified Schirmer test in dry eye and normal subjects: Open versus closed eye and 1-minute versus 5-minute tests. Cornea. 2010;29:384-7.
10. Mainville N, Jordan DR. Etiology of tearing: A retrospective analysis of referrals to a tertiary care ocuplastics practice. Ophthal Plast Reconstr Surg. 2011;27:155-7.
11. Price M, Cristina R, MichaelJ. The tearing patient: Diagnosis and management; Ophthalmic pearls. Eyenet External Disease, June 2009:33-35.
12. Kashkouli MB, Beigi B, Murthy R, Astbury N. Acquired external punctal stenosis: Etiology and associated findings. American J. Ophthalmol. 2003;136:1079-84.
13. Mathew RG, Olver JM. Mini-Monoka made easy: A simple technique for Mini-Monoka insertion in acquired punctal stenosis. Ophthal Plast Reconstr Surg 2011;27:293–4.
14.Takahashi Y, Kakizak H, Nakano T, Asamoto K, Ichinose A, Iwaki M. Anatomy of the vertical lacrimal canaliculus and lacrimal punctum: A macroscopic study. Ophthal Plast Reconstr Surg 2011;27:384-6.
15. Kristan RW, Branch L. Treatment of lacrimal punctal stenosis with a one snip canaliculotomy procedure and temporary punctal plugs. Arch Ophthalmol. 1988;106:878-9.
16. Ma’luf RN, Hamush NG, Awwad ST, Noureddin B. Mitomycin C as adjunct therapy in correcting punctal stenosis. Ophthal Plast Reconstr Surg 2002;18:285-8.
17. Konuk O, Urgancioglu B, Unal M. Long-term success rate of perforated punctal plugs in the management of acquired punctal stenosis. Ophthal Plast Reconstr Surg 2008;24:399-402.
18. Liarakos VS, Boboridis KG, Mavrikakis E, Mavrikakis I. Management of canalicular obstructions. Curr Opin Ophthalmol 2009;20:395-400.
19. Mohsen B,, Farzd P, Kiavash V. Assessment and management of proximal and incomplete symptomatic obstruction of the lacrimal drainage system. Middle East African Journal of Ophthalmolgy 2012:1:60-69.
20. Rosenstock T, Hurwitz JJ. Functional obstruction of the lacrimal drainage passages. Can J Ophthalmol 1982;17:249-55
21. Wormald PJ, Tsirbas A. Investigation and endoscopic treatment for functional and anatomical obstruction of the nasolacrimal duct system. Clin Otolaryngol Allied Sci 2004;29:352–6.
22. Liu D. Conjunctivochalasis. A cause of tearing and its management. Ophthal Plast Reconstr Surg. 1986;2:25–8.
23. Mombaerts I, Colla B. Partial Lacrimal Carunculectomy. A simple procedure for epiphora. Ophthalmology 2001;108:793–7.



