Why Smoothing?
Dr. Vinciguerra says the idea to try smoothing the ablation zone came from observing the effect the laser has on the corneal surface before the healing process starts.
"The key idea is, when you perform a refractive surgery ablation on the surface and then try to measure the topography, you can't, because the surface is no longer regular. And if you try to put the patient in front of the eye chart, he can't read any lines. He can read, though, when the epithelium is smooth again, so the 'smoothing agent' is the epithelium. That means the healing process will play a big role in terms of haze and delayed re-epithelium time." His idea is to help the healing process, and avoid haze and regression, by smoothing the surface right after the procedure. He also believes it can be helpful in some LASIK cases by providing a smoother interface for the flap.
Dr. Vinciguerra began smoothing corneas during some studies of phototherapeutic keratectomy, and was surprised by the results.
"For 100 µm of a PTK ablation, there would be no haze," he says. "But for only 30 µm of refractive ablation I got haze. So I thought I would try adding a few microns of smoothing at the end of refractive surgery with masking fluid. When I did this, the patient could read immediately, the healing process was faster and he returned to his best acuity faster than without smoothing."
After studying irregularities for several years, Dr. Vinciguerra says, "Any laser produces a certain amount of irregularity. A broad beam for example, has a diaphragm that opens and closes, creating steps over the cornea. If you use any flying-spot laser, what you get is like covering your desk with a lot of coins … you can't totally cover it, because there will be spaces between them. That's the source of irregularities with a flying spot. If you try to put on a second layer, you'll have some areas that are ablated twice, and some that are ablated once. Also, micro-movements such as saccadic eye motion and the heartbeat cause shifts the laser can't follow exactly."
To address these, his smoothing technique involves spreading a thin layer of a masking agent over the cornea, then ablating with excimer PTK.
Dr. Vinciguerra describes a prospective study of the technique he performed in which 147 eyes with ablation irregularities after PRK or LASIK were randomized into two groups: 74 would receive smoothing with PTK and a masking agent and 73 were patched immediately with no smoothing. The average preop refraction for the smoothing group was -7.55 D and it was -7.3 D for the controls.
Twelve months postop, the average haze in the smoothing group was 0.5 and the average haze in the control group was 1.2 (p=0.006). The average best-corrected acuity was 1.1 (nearly 20/16) in the smoothing group vs. 0.95 (a little below 20/20) in the control group (p=0.02). Sixty-eight percent of the eyes in the smoothing group were within 1 D of the planned correction vs. only 33 percent in the non-smoothing group.1
Another proof of the concept involved the work of Steven Wilson, MD. Dr. Wilson covered one half of an animal cornea with a metal mesh, then ablated it.2 The mesh led to a rough cornea after the ablation, and, as one might expect, the mesh-covered portion had much more haze than the uncovered half. For some of the mesh portions, however, the surgeon performed a smoothing procedure on the cornea immediately after the ablation, and discovered that those formerly rough corneas had better results than standard treatments with lower ablation levels but with no smoothing. "A 9-D ablation with the mesh and smoothing went better than a standard 3-D ablation," Dr. Vinciguerra says.
Several recent studies have also found smoothing improves results after PRK.3-5
The Technique
The masking agent used is crucial to the success of the smoothing procedure, says Dr. Vinciguerra. To this end, he developed a special masking agent, called Laservis (hyaluronic acid 0.4%, Chemedica, Munich, Germany), to improve the technique. "It's basically hyaluronic acid," he explains, "because you need a solution that has the same ablation rate as the corneal stroma, and because we need a totally transparent fluid. The hyaluronic acid also has a scavenger effect that protects the tissue. In addition, the elastic properties of the viscoelastic solution can reduce the excimer shock waves." He says the superficial tension of the fluid creates an extremely regular surface, and only the irregularities that are emerging will be ablated.
Dr. Vinciguerra begins his smoothing by washing the area with cooled BSS to clear out any ablation debris. He also cools the cornea with chilled BSS to retard corneal heating and any subsequent stromal alterations.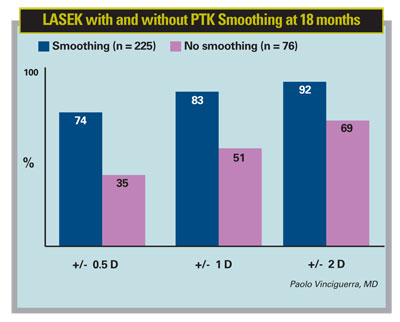
He then places a drop of his masking agent on the cornea, spreading it with a Castroviejo spatula (ASICO). If a dry area appears, he adds some fluid and redistributes it evenly. Dr. Vinciguerra spreads the fluid quickly, occasionally thinning the fluid layer with a slow movement in one direction and a lifting of the spatula.
"You need an even spread of the masking fluid," he says. "If not, there is a risk of having a dry area in which you're not performing smoothing, but rather are changing the shape of the cornea and inducing aberrations."
He says that in the first smoothing step, the layer must be thin to allow the irregularities to emerge and be ablated. In the following stages, when there are only small irregularities left, Dr. Vinciguerra keeps the fluid layer thicker to cover the entire stromal surface. The ablation is then performed on whatever irregularities protrude through the liquid. He recommends using fluorescein to reveal any dry areas as they emerge.
The PTK ablation uses a large diameter, usually 9 mm or larger, to avoid inducing hyperopia. Dr. Vinciguerra recommends performing a 10-µm ablation, which, through masking fluid, will ablate 1 or 2 µm of corneal tissue. "That doesn't change the spherical equivalent or induce hyperopic shift, but removes 1 µm of roughness from the ablation," he says.
Some surgeons remain skeptical of the usefulness or predictability of the technique. However, Dr. Vinciguerra feels it helps him every day. "It was difficult to demonstrate the difference between smoothing and non-smoothing for years, and some surgeons said it appeared 'too easy' to get these results," he says. "But now with our paper comparing smoothing to conventional treatments and Dr. Wilson's animal studies, we have good clinical and histological evidence."
1. Vinciguerra P, Azzolini M, Airaghi P, et al. Effect of decreasing surface and interface irregularities after photorefractive keratectomy and laser in situ keratomileusis on optical and functional outcomes. J Refract Surg 1998;14:S199-203.
2. Netto MV, Mohan RR, Sinha S, et al. Stromal haze, myofibroblasts, and surface irregularity after PRK. Exp Eye Res 2006;82:5:788-97.
3. Lombardo M, DeSanto MP, Lombardo G, et al. Roughness of excimer laser ablated corneas with and without smoothing measured with atomic force microscopy. J Refract Surg 2005;21:5:469-475.
4. Serrao S, Lombardo M, Mondini F. Photorefractive keratectomy with and without smoothing: A bilateral study. J Refract Surg 2003;19:58-64.
5. Serrao S, Lombardo M. Corneal epithelial healing after photorefractive keratectomy: Analytical study. J Cataract Refract Surg 2005;31:930-937.