The Swedish interactive threshold algorithm (SITA) short-wavelength automated perimetry testing is at least as diagnostically sensitive to early glaucomatous field loss as the older and lengthier full-threshold SWAP program, according to two researchers from the Department of Clinical Sciences, Ophthalmology, Malmö University Hospital, Lund University, in Sweden. SITA SWAP could become a useful clinical test for the detection of early glaucoma, the researchers say.
The diagnostic sensitivity of standard automated perimetry (SAP) using the SITA Fast program to detect early glaucomatous visual field loss was not significanty lower than that of the two SWAP programs, they add.
The researchers studied performance comparisons based on strategy-specific significance limits from a group of normal study participants. This cross-sectional, prospective study examined perimetric diagnostic sensitivity in 101 patients as defined by reference limits determined in the same healthy participants for all three test programs. No significant difference in the number of significantly depressed test point locations between the three programs could be detected, neither at the p<5 percent limit nor at the p<2 percent limit.
The difference in number of points depressed below the fifth percentile was 0.5 between full-threshold SWAP and SITA SWAP, 1.09 between full-threshold SWAP and SAP, and 1.04 between SITA SWAP and SAP. The number of eyes showing clusters of significantly depressed points also was similar with all three test programs: full-threshold SWAP identified clusters in 66 eyes; SITA SWAP identified clusters in 67 eyes; and SITA Fast SAP identified clusters in 65 eyes. Average test time was 12 minutes using full-threshold SWAP, 4.1 minutes with SITA SWAP, and 3.5 with SITA Fast.
The SITA SWAP identified at least as much glaucomatous visual field loss as the older full-threshold SWAP, although test time was considerably reduced. Conventional SAP using SITA Fast was not significantly less sensitive than either of the two SWAP programs.
(Ophthalmology 2006;113:1092-1097)
Bengtsson B, Heijl A.
Repeat Injections of Triamcinolone Acetonide for Diabetic ME
Repeat intravitreal injections of triamcinolone acetonide may lead to an improvement in visual acuity and a rise of intraocular pressure in patients with diffuse diabetic macular edema, according to researchers in a retrospective, interventional, comparative study. The German researchers say the duration of the effect after each injection lasts approximately six to eight months.
The study included a group of responders (19 patients, 22 eyes) with diffuse diabetic ME, who showed an improvement in visual acuity after an intravitreal injection of approximately 20 mg triamcinolone acetonide. The patients received a second intravitreal injection 10 ±3.8 months after the first injection. A control group consisted of 31 patients with diffuse diabetic ME without treatment during follow-up.
Follow-up after the second injection was 9.1 ±4.9 months. Four patients received a third injection at 9.7 ±3.7 months after the second injection, with a follow-up after the third injection that was at 7.9 ±11.5 months. After the second and third injections, visual acuity increased significantly (p=0.002 and p=0.068, respectively) by 1.8 ±2.1 and 4 ±2.6 Snellen lines, respectively. Eleven eyes showed an improvement in visual acuity by at least two Snellen lines after the second injection, and three patients (75 percent) experienced a gain in visual acuity by at least two Snellen lines after the third injection.
IOP increased significantly (p<0.01) after each injection, and returned to baseline values before each reinjection, the researchers say. Visual acuity improvement (p>0.05) and IOP rise did not differ significantly (p>0.55) between the various injections. Tachyphylaxis in visual acuity or IOP outcomes was not observed.
(Ophthalmology 2006;113:800-804)
Jonas JB, Spandau UH, Kamppeter BA, Vossmerbaeumer U, Harder B, Sauder G.
Written Instructions Affect Drug Regimen Accuracy
Written instructions from a doctor to a patient are a simple and inexpensive intervention that can have an effect on drug regimen accuracy. That's according to a prospective, case-controlled study from researchers at Wills Eye Hospital in Philadelphia and the Massachusetts Eye and Ear Infirmary in Boston. The study was supported by the National Eye Institute in Bethesda, Md.
The four glaucoma surgeons evaluated the accuracy of self-reporting of the prescribed medication regimen in their glaucoma population of patients in order to identify contributing factors and assess the effect of written instructions.
Questions were administered to the patients involved in the study at an urban resident glaucoma clinic by two interviewers. The questionnaire consisted of six questions regarding the name and dosage of the patients' ophthalmic medications (range: one to four), education level, ability to read, and age of the patient. At the end of the visit, patients were given a written chart describing their ophthalmic medications, frequency and dosage. At their next scheduled visit, the same questionnaire was repeated. The patients' responses from both visits were compared with the regimen they were prescribed and with each other, and this information was then used to determine the accuracy of reporting medications.
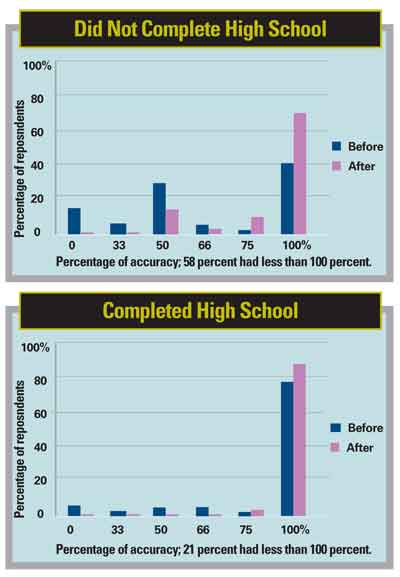
A total of 193 patients were en-rolled in the study; 164 patients (85 women, 79 men) completed both phases. The mean age was 68.40 +11.6 years. Of the patients, 84 had attained less than 12th grade education and 80 had completed high school. On the first visit, 66 patients showed less than 100 percent accuracy and 49 of 84 patients who had not completed high school education showed less than 100 percent accuracy with a mean score of 65 percent; 17 of 80 (21 percent) of patients who had completed high school showed less than 100 percent accuracy with a mean score of 87 percent.
After receiving written instructions, both the patients who had completed high school and those who had not showed improved reporting accuracy. Patients on one medication had 100 percent accuracy in reporting 82 percent of the time, whereas those with four medications had 100 percent accuracy 21 percent of the time. The education level of the patient and the number of medications showed direct correlation with patients' ability to report medications accurately.
The researchers say noncompliance with instructions on the part of the patient may be falsely interpreted as ineffectiveness of the medications, which may result in more invasive treatments such as surgery. The researchers add clinicians should consider employing written instructions for their patients, particularly for patients who use several medications and those with a lower level of education.
(J Glaucoma 2006;15:244-247)
Kharod BV, Johnson PB, Nesti HA, Rhee DJ.



