While the headlines in cataract surgery continue to focus on the rollout of laser cataract technology, researchers at ARVO 2012 are toiling away in some of the more traditional areas of interest, trying to further improve this remarkable procedure.
Intraocular Lens Issues
A group at the University of British Columbia, Vancouver, compared the accuracy and precision of intraocular lens formulas in predicting postoperative spherical equivalent outcomes, as well as the accuracy and precision in three lenses. The retrospective chart review included 90 cataract surgery patients receiving either the Tecnis 1, MIL Akreos or Alcon AcrySof IQ lens. The Holladay 1, Haigis and SRK/T formulas calculated predicted spherical equivalent for each lens. Differences between predicted SE and postoperative SE were analyzed using means (as a measure of accuracy) and standard deviations (as a measure of precision).
The Tecnis 1 lens had the lowest mean using the SRK/T formula and lowest SD using the Holladay 1 formula. All three formulas had near equal means in the Alcon AcrySof IQ lens, however the SRK/T formula had the lowest SD. The MIL Akreos lens had the lowest mean and SD using the Holladay 1 formula. Among the lenses, the lowest means and SD were achieved with the Tecnis 1 lens, while the MIL Akreos lens had the highest means and SD.
The group judged the Tecnis 1 lens to be most accurate with the SRK/T formula, most precise with the Holladay 1 formula, and both most accurate and precise with the Haigis formula. The Alcon AcrySof IQ lens was nearly equal accuracy and precision in all three formulas. The MIL Akreos lens was most accurate and precise with the Holladay 1 formula. Of the three lenses in the study, the Tecnis 1 lens performed better compared to others in accuracy and precision, and the MIL Akreos lens performed poorly compared to others.6735
Surgeons in Frankfurt, Germany say their first-year results provide evidence that the angle-supported phakic AcrySof Cachet IOL (Alcon) is an efficient and safe device to correct moderate to high myopia. (One of the group reports a commercial relationship with Alcon.)
This retrospective study enrolled 72 myopic eyes in which the lens was implanted by the same surgeon. Pre- and postop endothelium cell loss, intraocular eye pressure and visual acuity were compared.
|
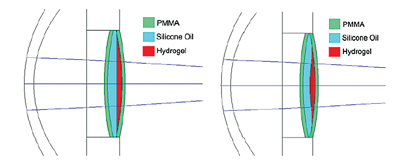
A trio of researchers at the University of Arizona is reporting the accommodative capabilities of a new curvature-changing IOL. Elastic hydrogel material is sandwiched between two PMMA plates. One of the plates has a small aperture through which the hydrogel can be partially extruded when the plates are compressed. The extruded hydrogel takes on a roughly parabolic shape and consequently imparts optical power to the system (See image, above).
Earlier versions immersed in aqueous, despite achieving 8 D of refractive change, worked counter to the natural accommodative mechanism of the eye: The plates were compressed resulting in increased optical power when accommodation was relaxed and a lower power when the eye was accommodated. They learned that immersing the hydrogel interface in a high-index solution such as silicon oil allows the power change to occur in the proper direction. When the aqueous is replaced with silcone oil with a refractive index of 1.52, the same compression leads to a power change of 4.4 D, and the direction the power change works is correct for the eye’s natural accommodation mechanism, the group reports.6331
Surgical Issues
A team from India’s Aravind Eye Hospitals and Johns Hopkins University sought to better elucidate the intraoperative and late postoperative complications of cataract surgery in eyes with pseudoexfoliation. The prospective six-armed study in India enrolled subjects with clinical pseudoexfoliation with or without glaucoma, without preexisting phacodonesis, requiring phaco over 10 months. The control group had phaco but no pseudoexfoliation. All procedures were performed by senior, experienced high-volume cataract surgeons. The present report is limited to intraoperative complications.
PXF patients were randomized to four groups: single-piece AcrySof (Alcon) lens with and without capsular tension ring, and three-piece AcrySof lenses with and without CTR.
Controls were randomized to the same lenses, without CTR. PXF groups totaled 662 eyes and controls, 400; mean age was 61.4 ±7.3; mean IOPs were 14.4 ±3.3 in the PXF groups and 13.9 ±2.9 in controls (p=0.021).
About 55 percent of cataracts were nuclear sclerotic while 0.4 percent had only posterior capsular changes. On LOCS III cataract grading, 65 percent of PXF groups had nuclear color of 3+ or more compared to 50 percent of the controls (p<0.001). Nearly 62 percent of PXF patients had dilated pupils <7 mm. Complications did not differ between groups: zonulodialysis in six PXF (0.9 percent) and two controls (0.5 percent); posterior capsular ruptures in three PXF (0.8 percent) and three controls; vitreous loss in four (0.6 percent) PXF and two controls (0.5 percent); and dropped lens fragments in two PXF (0.3 percent) and one control (0.2 percent).
In this, the first long-term, prospective, controlled randomized study evaluating the effects of different IOL styles and the presence or absence of a CTR on surgical complications in pseudoexfoliation, PXF eyes without preexisting phacodenesis did not differ initially from control eyes with regard to intraoperative complications. Because of the low complication rate, no differences were detected in experienced hands irrespective of IOL type or use of a CTR. Longer follow-up will reveal if lens choice or the use of a CTR is related to clinically significant late complications.6619
Surgeons at two locations in San Antonio studied the visual outcomes of patients with retained lens material after cataract surgery who had early versus late pars plana lensectomy.
The three-year retrospective chart review divided patients referred to a single private retina practice into an early group (1), who underwent pars plana vitrectomy within the first 14 days of surgery, and a late group (2), who had PPL performed greater than two weeks after surgery. Demographics, pre- and postop VA and complications were collected for six months after PPL. There were 15 patients (average age 72) in group one and 11 patients (average age 74) in group two, with a 2:1 female-to-male ratio. Fifty percent of the patients in each group had diabetes. None of the patients had CSME or age-related macular degeneration prior to cataract surgery.
In group 1, the average retina referral time was three days, as was the average time between cataract surgery and retina surgery. In group 2, the average retina referral time was 96 days. The average PPL from referral date was nine days. About 20 percent of patients at the time of retina referral were aphakic in both groups. The preop logMAR VA prior to PPL in group 1 was 1.49 and in group 2, 0.94. Postop acuity was evaluated at one week, and one and six months. Although there was no significant difference in VA outcome between the two groups, there was a trend toward significance at week one (1.14 vs. 0.6; p:0.07) with group 2 having a slightly better VA at week one. Postop VA at six months was 0.81 (group 1) and 0.67 (group 2). One patient in group 1 developed retinal detachment and there was a higher number of patients developing CME in group 2. There was no significant difference in patients’ final VA between the groups. However there was a trend toward a higher rate of CME in patients in group 2. A subgroup analysis of the CME cases in group two revealed that 75 percent had diabetes.6667
A pair of researchers at Columbia University’s Harkness Eye Institute in New York City wanted to determine whether a 2.2-mm corneal incision produced different level of astigmatism from a 2.6-mm incision. Their retrospective study reviewed 344 eyes of 222 patients with a 2.2-mm incision and 406 eyes of 279 patients with a 2.6-mm incision. Before and after surgery, the surgeon measured corneal curvature with a manual keratometer. Data was collected at one day, one week, two weeks, one, two, four and six months, and every six months thereafter up to 30 months. Surgically induced astigmatism for each eye at each time interval was calculated with the Jaffe method. The difference in SIA between the 2.2-mm and 2.6-mm incisions at each follow-up interval was determined with the “two sample t-test,” and one-way ANOVA was used to compare SIA at each postoperative interval within each group.
Mean SIA was greater at all intervals after the 2.6-mm incision than the 2.2-mm incision, but not statistically significantly so (all p>0.05). After one week, including one week, SIA after each incision did not change significantly (p=0.67 for 2.2-mm incision, 0.94 for 2.6-mm incision).
Though the smaller 2.2-mm incision should theoretically accelerate healing and stabilization of the wound and the cornea, this study did not show a significant difference in SIA after these two incisions during the initial 30 months after surgery.6644
Pharmaceuticals
Following the institution of universal perioperative ketorolac use at the local VA Medical Center, surgeons at the University of Florida, Gainesville, conducted a retrospective chart review of all patients who underwent cataract surgery one year prior to and one year after the change. Surgical complications or pre-existing risk factors for cystoid macular edema were exclusions. The study included 157 patients who received perioperative ketorolac and 154 patients who did not. Demographic information and preop VA were recorded, along with postop VA at six time points out to 12 months. Since patients had not been refracted at every time point, a “final visual acuity” was documented for the visit closest to 12 months at which the patient had been refracted. This visit was required to have occurred between six and 18 months postop (See Table 1, below.)
|
Researchers in Brazil have added to the evidence that there is no need to add ketorolac to routine cataract surgery. In a masked single-center, randomized study that comprised 46 patients undergoing cataract surgery, cataract surgery patients with no recognized CME risks were randomized to receive either topical prednisolone acetate 1% q.i.d. plus dextran 70/hypromellose q.i.d. (placebo group; n=25) or topical prednisolone 1% q.i.d. plus ketorolac tromethamine 0.4% q.i.d. (ketorolac group; n=21) for three days preoperatively and four weeks postoperatively. In both groups topical gatifloxacin was administered to the treated eye q.i.d., starting three days before surgery and continuing for seven days. The average age of patients were 67.88 (SD=8.85) in the placebo group versus 67.29 years (SD=12.10) in the ketorolac group (p=0.849). The primary outcome measured on the 30th day after surgery was best-corrected visual acuity. Other outcomes included were intraocular pressure, CME incidence and retinal thickness as measured by spectral-domain optical coherence tomography.
The mean BCVA was 0.086 logMAR (0.82 Snellen decimal scale) in the placebo group vs. 0.167 logMAR (0.68 Snellen decimal scale) in the ketorolac group (p=0.045). The mean IOP was 13.08 mmHg (SD=2.66) in the placebo group versus 13.05 mmHg (SD=2.85) in the ketorolac group (p=0.968). No patient had clinically significant CME. One (4 percent) patient in the placebo group and two (9.52 percent) patients in the ketorolac group had angiographic CME (p=0.584). Mean retinal thickening was 228.56 µm (SD=24.95) in the placebo group versus 224.86 µm (SD=22.33) in the ketorolac group (p=0.602).6683
Prophylactic use of topical NSAIDs may be reserved for patients who are at higher risk of developing CME, and may not be cost-effective for patients undergoing routine cataract surgery, based on a three-year retrospective study at Philadelphia’s Wills Eye Institute.
A total of 925 operated eyes of 700 patients were reviewed, with preexisting macular edema and less than 28 days of follow-up as exclusions. In patients meeting inclusion criteria, 234 eyes (27 percent) did not receive perioperative NSAID, while 648 eyes (73 percent) did. Twenty-nine patients developed pseudophakic CME (3.3 percent). Rates of CME were 3.2 percent in the NSAID group, and 3.4 percent in the non-NSAID group (p=0.55).6691
Miscellaneous
The latest data from the Beaver Dam Eye Study strongly supports the past findings of an association of cataract surgery with late age-related macular degeneration, independent of other risk factors including high-risk genetic status. The authors, from several institutions in Wisconsin and Ohio, suggest the importance of considering these findings when counseling patients regarding cataract surgery. These findings should provide further impetus for the search for measures to prevent or delay the development of age-related cataract.
The 20-year study recruited subjects 43 to 84 years of age in 1987-1988. Participants were followed up at five-year intervals after the baseline examination in 1988-1990. Examinations consisted of ocular examination with lens and fundus photography, medical history, measurements of blood pressure, height and weight. Values of risk variables were updated, and incidences of early and late AMD were calculated for each five-year interval.
After controlling for age and sex, neither cataract nor cataract surgery was associated with increased odds for developing early AMD. Further controlling for high-risk gene alleles and other possible risk factors did not materially affect the odds ratio. However, cataract surgery was associated with incidence of late AMD (OR 1.93). This OR was not materially altered by further controlling for high-risk alleles or for other risk factors. The OR for late AMD was higher for cataract surgery performed five or more years prior as compared to less than five years prior.
The group says these findings should provide further impetus for the search for measures to prevent or delay the development of age-related cataract.1722
|
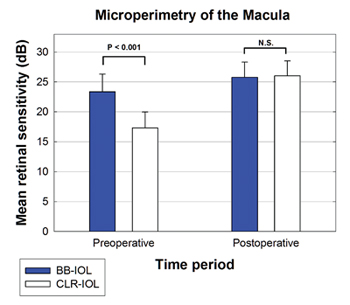
A significant difference between the clear and blue-blocking groups was found preoperatively (p<0.001); no significant difference was evident after surgery, with both groups having normal mean retinal sensitivity (See graphic, right). Both groups showed significant improvement in mean retinal sensitivity due to the cataract removal (p<0.001). Central stimuli data had similar significance. Although the two groups started at significantly different levels of mean retinal sensitivity due to varying cataract densities, the two groups were statistically identical and clinically normal in mean sensitivity after the procedure. The group says the result confirms that there is no significant difference in the ability of patients with clear or blue-blocking IOL to detect threshold white light stimuli.3069
Scientists at McGill University, Montreal, are testing the feasibility of applying acute heat shock before placing an IOL in the capsular bag to reduce lens epithelial cells’ numbers, decreasing their ability to migrate and lead to posterior capsule opacification. The study is partially funded by Alcon.
After determining the optimal temperature and application (60 C applied for 60 seconds) the cell line was cultured according to standard protocols. Media was replaced by pre-heated media (60 C for trials and 37 C for controls). After 60 seconds, the heated media was replaced by 37 degrees C media. The chamber slides were stained with H&E after 0-, two- or four-hour recovery times. Relative cell count by comparing image area covered by cells was measured and an average was obtained.
There was a significant decrease in relative cell count when treated with 60 C media compared to controls for all recovery times (51.3 percent decrease p=0.00081 at 0 hours, 69.3 percent p=0.00007 at two hours, 51.8 percent p=0.00209 at four hours). There were no significant differences in relative cell count between recovery time points. The group proposes heat shock as a simple and successful method to reduce lens cell viability, and that such a decrease may delay the occurrence of PCO. Further studies including an animal model are under way to quantify its benefits and side effects. This strategy could be a straightforward and low-cost improvement on the long-term outcomes following cataract surgery.6674
Intraoperative OCT measurements of the lens capsule allows qualitative morphological as well as quantitative biometric assessment of the anterior segment during surgery, according to surgeons in Vienna, Austria. Their prospective study divided cataract surgery patients into emmetropic, myopic and hypermetropic groups as defined by planned IOL power. A prototype operating microscope with an anterior segment OCT device measured the lens capsule position at different time points during cataract surgery. To improve the quality of the measurements, all patients received a capsular tension ring to result in a taut posterior lens capsule. Anterior chamber depth was measured before and after surgery by partial coherence interferometry.
Fifty eyes of 50 patients were included. Mean axial length was 23.8 mm (r: 20.6 to 29.5 mm); mean planned IOL power was 20.1 D (r: 1 to 31 D). The correlation between the preop, phakic ACD and the intraop OCT at the beginning of surgery was r2=0.6 (p<0.05). Excluding six cases in which the intraop measurement was not centered on the cornea, the correlation was r2=0.85 (p<0.05). The correlation between the postoperative pseudophakic ACD and the intraoperative measurements after implanting a CTR and after implanting the IOL showed a moderate correlation for the posterior capsule position, and a relatively good correlation for the anterior capsule position. The group believes this new surgical tool may help to enhance outcomes for patients undergoing cataract surgery.6718
With the increasing use of intravitreal injection for retinal diseases, surgeons at the Kresge Eye Institute, Detroit, wanted to determine whether the practice contributed to greater complications in cataract surgery. From seven years of billing codes, they selected patients who received IV injections prior to cataract surgery to determine the number of injections, ocular history, preop and postop VA, and any complications during cataract surgery. Exclusions: vitrectomy prior to cataract surgery, chronic recurrent uveitis, and complex cataract procedures. The number of reported complications was then compared to an age-matched control group.
In 46 patients who met the inclusion criteria, three complications of posterior capsule rupture were reported, with two of the patients requiring pars plana vitrectomy for posterior lens dislocation. In the control group of 200 patients, there were four complications of posterior capsule rupture. The complication rate in the injection group was 6.5 percent versus 0.5 percent of the controls. No correlation (p=.3382) was found between IV injections and risk for complications during surgery, although the average number of injections in the group without complications was 2.6 as compared to 15 injections in the complication group. A larger study with stratification of injection frequency is needed, the authors say.6703 REVIEW
Dr. Blecher is in private practice in Philadelphia. He is the co-director of the Cataract Service at Wills Eye Institute and the founding chief medical editor of the Review.