While phaco tools, lenses and surgical techniques have advanced sufficiently to make cataract surgery an outpatient procedure, there's also been a creep up in some post-surgical complications. In this article, Samuel Masket, MD, of Los Angeles, explains the upswing in incidence of late posterior chamber lens dislocation and describes how he approaches each case of a malpositioned intraocular lens.
"We've learned over time that certain conditions, pseudoexfoliation being a primary example, are associated with a progressive contracture of the anterior lens capsule following surgery," says Dr. Masket. He says the ophthalmic literature is finally showing what a number of surgeons have been experiencing: In as few as five, or as many as 10 years following cataract surgery with capsulorhexis, progressive zonular weakness due to anterior capsule contraction with phimosis can lead to late dislocation of the bag/IOL complex.
Dr. Masket attributes late IOL dislocation to the otherwise-positive adoption of capsulorhexis. "Before 1990, most cataract surgeons were making the anterior capsulotomy in a can-opener fashion that removed a larger part of the capsule," he says. "Because no uninterrupted anterior capsule ring was left behind, fibrosis rarely resulted. But now, in some cases, we note that the anterior capsular remnant undergoes fibrometaplasia with potential phimosis and zonular instability."
Those Most at Risk
Among those patients at greater risk for capsular phimosis and fibrosis post-surgery are those with pseudoexfoliation syndrome, followed by patients with chronic anterior segment inflammation or uveitis, retinitis pigmentosa, myotonic dystrophy, some patients with diabetes, and post-vitrectomy patients. In general, Dr. Masket names those with a chronic breakdown in the blood-aqueous barrier.
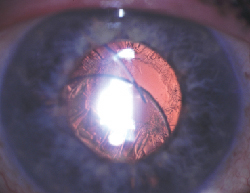 |
| The IOL may be poorly centered early or late after surgery due to iatrogenic causes, previous trauma, capsule contraction, or conditions such as pseudoexfoliation or uveitis. Photo: Samuel Masket, MD |
Patients with any of these conditions should be followed carefully postop for signs that the capsule is contracting. "If one notes significant constriction, I strongly recommend using the Nd:YAG laser to create radial relaxing incisions in the anterior capsule to reduce the effect of the centripetal fibrotic traction," he instructs.
Certainly, however, there are other causes of malpositioned IOLs. Should the original cataract surgery be complicated by rupture of the posterior capsule, dehiscence of zonules, or a poor anterior capsulorhexis, the IOL may be poorly centered early or late after surgery.
The Approach
The essence of Dr. Masket's approach to addressing a malpositioned posterior chamber IOL is to individualize. Given that a surgeon has essentially three options when faced with this complication—observation, removing the IOL or repositioning the existing IOL—Dr. Masket says that it's worth considering closely the details of each case before proceeding. "The needs of each case should be measured individually and surgery or non-surgical treatment applied as appropriate," he says. Non-surgical treatment is generally in the form of pharmacologic pupil miosis.
"My first step is to determine the needs of the patient and the etiology of the problem. If there are no symptoms and the condition has been relatively stable over a period of time, then no immediate action is required." Dr. Masket notes that it is possible for the ophthalmologist to be the first person to notice a dislocation in an asymptomatic patient.
Even if the decentration is not a problem to the patient, the surgeon may recognize it as potentially serious. "The ophthalmologist should determine what is the underlying cause of the dislocation, and if it's likely to be progressive," Dr. Masket instructs. "Some conditions are urgent. If the patient has a large defect in the zonules or in the capsule, a lens can dislocate into the posterior segment rapidly." Conversely, a patient could be symptomatic with a dislocated lens that's in a relatively stable condition. In these latter cases, surgery is more elective than urgent, says Dr. Masket.
IOL dislocation following trauma is a different situation, says Dr. Masket, because it's usually a stable one. "The patient has an injury, a certain amount of damage is done, but it tends not to be progressive," he explains. Trauma is the other side of the coin from capsule constriction and zonulysis due to pseudoexfoliation or a related disorder. "These cases exhibit progressive disease," he says, and should be approached accordingly. This may entail treatment of the primary ocular disease, repositioning of the IOL, and consideration of the complications particular to that disease when making decisions about repositioning procedures.
Surgical Options
Once it's been decided that surgery is indicated, Dr. Masket seeks the least invasive option possible. "If the lens is salvageable and it can be affixed to an appropriate part of the eye in a stable manner, that would be my preference," he relates. "If a patient has a very solid, relatively central and round anterior or posterior capsulotomy, one can capture the optic in front of or behind the capsular opening. That's the simplest solution."
• Iris suture. "The next least invasive procedure is to sew the existing malpositioned IOL to the iris. This assumes that there is adequate iris tissue available. It's generally necessary to remove the implant from the capsular bag because the bag has accumulated regenerating lens material" (e.g. Soemmering's ring). "Unless one removes that material," he says, "there's potential for it to be liberated within the eye, potentially inducing inflammation and elevating intraocular pressure." Dr. Masket prefers to use an automated vitrector device to cut away the capsular bag and then reposition the existing lens by suturing it to the iris.
• Scleral suture. Next on Dr. Masket's increasing scale of invasiveness is sewing the existing lens to the sclera. This may be accomplished by "lassoing" the loops to the sclera with non-absorbable sutures, or by working through sclerotomies made in the pars plana. Posterior segment surgeons generally employ the latter method, and many anterior segment surgeons are less comfortable with it than posterior-segment or vitreoretinal surgeons may be.
"[Anterior segment surgeons] often don't have the tools such as the microforceps to go through small sclerotomies, capture the loop, fix the suture to it and then sew it to the eye wall," says Dr. Masket. Nevertheless, the lasso method, which can be employed by surgeons in either camp, works well for fixating IOL loops or capsular tension rings to the sclera.
Just where to sew the lens to the eyewall depends on whether the lens needs to be sutured on both haptics or just one, says Dr. Masket. "If both need to be sutured, I avoid the 3- and 9-o'clock positions. You don't want to interfere with the long ciliary vessels and nerves, and it cuts down the potential for bleeding." He prefers to tie the sutures in the oblique quadrants. In cases where one haptic is well-positioned in either the sulcus or the capsule bag, and just one loop is free, Dr. Masket sutures that haptic to the sclera "where it lies."
Dr. Masket stresses the need for anterior segment surgeons to become comfortable working through the pars plana to deal with malpositioned posterior chamber IOLs. Other vital techniques are capsule capture, iris suturing techniques, both the McCannel and Siepser methods, and scleral suturing, particularly the lasso technique.
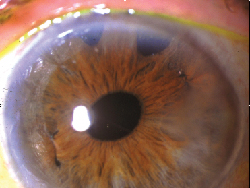 |
| McCannel suture fixation of a posterior chamber lens to the iris requires the least invasive surgery and preserves the conjunctiva. Photo: Samuel Masket, MD |
• IOL removal. A final choice, and certainly the most invasive, is to remove the decentered IOL. "If we can't use the existing lens and sew it to either the iris or the eyewall, then that lens must come out," Dr. Masket explains.
Removal may be necessary if the haptics are severely damaged or have separated from the optic. Furthermore, some IOLs are not well-suited for suturing to either the iris or the sclera, such as one-piece AcrySof IOLs.
Once the dislocated lens has been removed, the surgeon can suture a new implant to the iris, to the sclera, or he may consider using an anterior chamber lens. Approach this choice with caution, advises Dr. Masket. "Most eyes with problems of this nature tend to be already compromised," he explains. "They may have glaucoma, which is common in eyes with pseudoexfoliation syndrome or in cases of trauma. In these eyes, the use of the angle for an anterior chamber lens may be contraindicated." To avoid glaucomatous complications, Dr. Masket thinks patients in this category are best served with new lenses sutured to the iris as a first choice or to the sclera.
Variables
• Implant materials and design. Besides contraction of the capsule, some IOLs themselves may be implicated in the increase in this complication. Dr. Masket has found certain implant materials and styles more likely to generate a fibrotic transformation of the anterior subcapsular lens epithelial cells. "In general, silicone is more likely to incite this fibrometaplasia than is acrylic," he says. He notes that early generation silicone induces more reaction than the later generations, particularly third-generation silicone with an index of refraction of 1.46.
• Suture material. Late dislocation of sutured implants may be attributed to something as simple as a breakdown in the suture material. In younger patients who expect to live as much as 20 years with their implants, biodegradation of the suture has been reported commonly. Dr. Masket believes that, as we are seeing an ever-increasing number of late malposition of lenses, the market is looking anew at suture material. "The only suture that we've had for any period of time has been 10-0 polypropylene. We've learned that it does, very slowly, biodegrade, and that, over time, it can fracture," he says. "My current material of choice is 9-0 polypropylene. Its diameter is at least twice that of 10-0, making it much slower to degrade and less likely to fracture."
• Capsular tension rings. If a patient is identified at the initial cataract surgery to have weak zonules or one of the aforementioned disease conditions that makes later implant dislocation likely, the smart choice may be to insert a capsular tension ring (AMO Santa Ana, Calif., or Morcher, Stuttgart, Germany). The ideal choice of ring would be the Cionni-modified ring, says Dr. Masket, because the added eyelet(s) would provide an excellent base for suturing the capsule to the sclera if late dislocation occurs. (To date, the Cionni CTR is still under FDA review.)
• Working environment. Finally, Dr. Masket likes to point out what he's learned about the working environment for repositioning procedures in these patients who have already had cataract surgery. "Working in low illumination is important. I've seen cases where unfortunately the patient developed a photic maculopathy because the bright light used during the procedure caused damage," he explains. Learning to work under low illumination can help avoid the risk of creating retinal complications from a successful IOL repositioning surgery.
Dr. Masket is a clinical professor of ophthalmology at the Jules Stein Eye Institute, UCLA School of Medicine and is in private practice in Los Angeles.
Recommended Articles:
Chang DF. Siepser slipknot for McCannel iris-suture fixation of subluxated intraocular lenses. J Cataract Refract Surg 2004;30:1170-1176.
Han QH, Wang L, Hui YN. Transscleral suture technique for fixation of a dislocated posterior chamber intraocular lens. J Cataract Refract Surg 2004;30:1396-1400.
In YS, Kim JH, Song BJ. Transscleral fixation of a dislocated IOL through sclerotomy. J Cataract Refract Surg 2004;30:1163-1166.
Lin CP, Tseng HY. Suture fixation technique for posterior chamber intraocular lenses. J Cataract Refract Surg 2004;30:1401-1404.
| Role of the Capsular Tension Ring | |
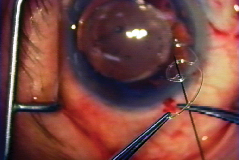 |
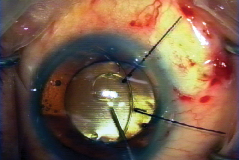 |
| Passing suture through eyelet of CTS. All Photos: Ike K. Ahmed, MD. | Placing CTS within capsular bag. |
|
We know that the capsular tension ring can be of great assistance in augmenting zonular support during cataract surgery. What is the role of such a device in an IOL repositioning procedure? Use Post-dislocation Early Intervention | |



