Despite the fact that glaucoma is not always associated with elevated intraocular pressure, lowering IOP by medical or surgical means is the only approved treatment. Currently, medications for this purpose fall into two categories: those that cause a decrease in aqueous production (including beta-blockers, carbonic anhydrase inhibitors and alpha-2 agonists), and drugs that either increase outflow facility through the trabecular meshwork, such as pilocarpine, or increase uveoscleral outflow, such as prostaglandins and alpha-2 agonists. (The latter cause this as a secondary effect.)
However, none of these medications address the most common cause of glaucoma: resistance to aqueous outflow in the trabecular meshwork, with maximal resistance in the juxtacanalicular region and Schlemm's canal. That could explain why a good percentage of glaucoma patients require more than one class of glaucoma medication—and some of them remain uncontrolled even on maximal medical therapy, thus requiring surgical intervention. When we treat neovascular glaucoma or neovascularization of the retina we know that VEGF is the cause of the damage, and we can target it with anti-VEGF. So far, we haven't been able to direct our treatment of primary open-angle glaucoma with anything approaching that level of specificity.
That may be about to change, thanks to a promising new class of medications: Rho-kinase inhibitors. Rho-kinase is an important downstream regulator of Rho-GTPase proteins, which are known to play a role in many cellular functions, including proliferation and apoptosis. It's been shown that alteration in the level of Rho-kinase plays a role in the pathophysiology of several age-related diseases, including pulmonary hypertension, diabetes and renal disorders. At the same time, inhibitors of Rho-kinase have been shown to play a critical role in regulating the contractile tone of smooth muscle tissue (in a calcium-independent manner), and are being used to treat patients with stroke, or cerebral or cardiac vasospasm—all age-related diseases.
Given that glaucoma is also age-related, it's not surprising that clinical data supports a role for Rho-kinase in this disease. One study demonstrated that sustained activation of Rho-GTPase signaling in the aqueous humor outflow pathway increases resistance to outflow through the trabecular meshwork, by influencing the actomyocin assembly cell adhesive interaction and expression of extracellular matrix protein and cytokinase in trabecular meshwork cells.1 In addition, levels of Rho-GTPase agonists, including endothelial 1 and TGF-beta, have been reported to be elevated in the aqueous humor of glaucomatous patients.2,3
Four Avenues to Success
Because of their involvement in cellular function and their ability to relax smooth muscle tissue, Rho-kinase inhibitors tested in animal models are showing potential for use in glaucoma treatment in four different ways.
First, Rho-kinase inhibitors may be able to increase aqueous outflow by relaxing trabecular meshwork tissue. Studies have demonstrated that selective Rho-kinase inhibitors reduce intraocular pressure and increase outflow facility by altering the behavior of trabecular meshwork cells and relaxing ciliary muscle in bovine and human tissue;4,5 topical or intravitreal or intracameral injection of Rho-kinase inhibitors in rabbits lowers IOP in 30 minutes, with the effect lasting six to 12 hours;4 and a Phase I clinical trial has demonstrated that SNJ-1656, a selective Rho-kinase inhibitor, used topically at different concentrations is safe and effective in reducing IOP in humans.6
Rho-kinase inhibitors may benefit glaucoma patients in a second way: by improving blood flow to the optic nerve. Altered optic nerve perfusion, due either to vasospasm or altered hemodynamics, is believed to play a role in the pathophysiology of certain types of glaucoma—especially normal tension glaucoma—and it is believed that some of these glaucoma patients may have altered blood perfusion in the rest of the body as well.7,8 There is increasing evidence that Rho-kinase plays an important role in cerebral and cardiovascular disease. For example, estrogen can suppress Rho-kinase activity in cerebral circulation, which may contribute to the low incidence of cerebrovascular disease in pre-menopausal females,9 and Rho-kinase inhibitors have shown benefit in treating cardiac vasospasm.10
The third way Rho-kinase inhibitors may help us combat glaucoma is by protecting healthy ganglion cells. Animal studies have shown the involvement of Rho-kinase in induced neurotoxicity, and that Rho-kinase inhibition at the cell body is neuroprotective and overcomes growth inhibition.11,12 In addition, animal studies have shown an increase in retinal ganglion cell survival with Rho-kinase inhibitors.13
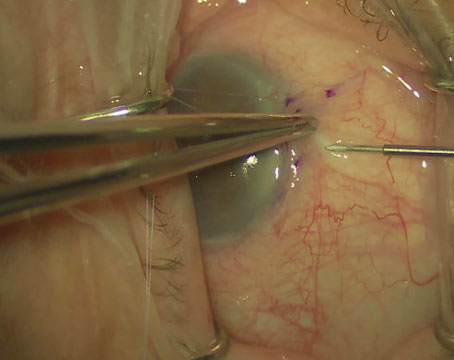
The fourth way Rho-kinase inhibitors may aid us in treating glaucoma is as an antifibrotic agent in glaucoma surgery. One of the main reasons for failure of glaucoma surgery is scarring. Although the use of antimetabolites (5FU or mitomycin C) has decreased the incidence of glaucoma surgery failure, it's associated with a higher incidence of bleb-related complications. In contrast, one study demonstrated that topical use of Y 27632 (a Rho-kinase inhibitor) is associated with reduced subconjunctival scarring in rabbits after filtration surgery and that it was safe and well-tolerated.14 (Further studies are needed to determine optimal dosage and length of use.)
The one notable problem with using Rho-kinase inhibitors to treat glaucoma at this point is that we don't have a selective Rho-kinase inhibitor. Being able to target only the desired cells may be crucial, because increasing the concentration of a non-specific Rho-kinase inhibitor could have undesirable consequences. Given our limited knowledge about the multitude of biochemical systems and interactions taking place inside the eye, it's impossible to know what the exact effect of increasing the level of non-specific Rho-kinase inhibitors might be, but a molecule designed to affect only trabecular meshwork tissue would be a safer alternative.
Another Step Forward
Companies currently developing Rho-kinase inhibitors include Senju Pharmaceuticals (
Given our limited armamentarium of tools for treating glaucoma, a new approach like this could mean a significant improvement in our ability to help our patients. It's still early in the game, but the outlook is promising.
Dr. Al-Aswad is assistant professor of clinical ophthalmology at the Columbia University College of Physicians and Surgeons, Edward S. Harkness Eye Institute. She has no financial interest in any of the products or companies mentioned.
1. Zhang M, Maddala R, Rao PV. Novel molecular insights into RhoA GTPase-induced resistance to aqueous humor outflow through the trabecular meshwork. Am J Physiol Cell Physiol 2008;295:5:C1057-70.
2. Noske W, Hensen J, Wiederholt M. Endothelin-like immunoreactivity in aqueous humor of patients with primary open-angle glaucoma and cataract. Graefes Arch Clin Exp Ophthalmol. 1997;235:9:551-2.
3. Tripathi RC, Li J, Chan WF, Tripathi BJ. Aqueous humor in glaucomatous eyes contains an increased level of TGF-beta 2. Exp Eye Res 1994;59:6:723-7.
4. Honjo M, Tanihara H, Inatani M, Kido N, Sawamura T, Yue BY, Narumiya S, Honda Y. Effects of rho-associated protein kinase inhibitor Y-27632 on intraocular pressure and outflow facility.
Invest Ophthalmol Vis Sci 2001;42:1:137-44.
5. Rao PV, Deng PF, Kumar J, Epstein DL. Modulation of aqueous humor outflow facility by the
Invest Ophthalmol Vis Sci 2001;425:1029-37.
6. Tanihara H, et al. Intraocular pressure–lowering effects and safety of topical administration of selective ROCK inhibition, SNJ-1656 in healthy volunteers. Arch Ophthalmol 2008;126:3:309-15.
7. Delaney Y, Walshe TE, O"Brien C Delaney Y, et al. Vasospasm in glaucoma: Clinical and laboratory aspects. Optom Vis Sci 2006;83:7:406-414.
8. Grieshaber MC, Flammer J. Blood flow in glaucoma. Curr Opin Ophthalmol 2005;16:2:79-83.
9. Chrissobolis, S. et al. Evidence that estrogen suppresses Rho Kinase function in the cerebral circulation in vivo. Stroke 2004; 35:2200-2205
10. Kandabashi, T et al. Evidence for protein kinase C-mediated activation of Rho-kinase in a porcine model of coronary artery spasm. Arterioscler Thromb Vasc Biol 2003;23:12:2209-2214
11. Kitaoka Y, et al. Involvement of RhoA and possible neuroprotective effect of fasudil, a Rho-kinase inhibitor, in NMDA-induced neurotoxicity in the rat retina. Brain Res 2004;1018:1:111-8.
12. Bertrand J, Winton MJ, Rodriguez-Hernandez N, Campenot RB, McKerracher L. Application of
13. Bertrand J, Di Polo A, McKerracher L. Enhanced survival and regeneration of axotomized retinal neurons by repeated delivery of cell permeable C3-like
14. Honjo M, et al,. Potential Role of Rho-Associated Protein Kinase Inhibtor Y27632 in glaucoma filtration surgery. Invest Ophthalmol Vis Sci 2007;48:12:5549-5557.