Optical coherence tomography has given ophthalmologists a window into the eye that they never had before, and the features of the various OCT devices on the market continue to multiply. With OCTs’ new modules and optional features, physicians can use the devices to evaluate the effects of surgery, diagnose conditions and follow the progression of disease and therapies. Here’s a look at the latest features available on OCT units that can help you better manage patients.
Bioptogen
Bioptigen’s Envisu C-Class spectral domain OCT systems are mobile devices with handheld imaging heads that capture images at 32,000 lines per second down to an axial resolution that the company says depends on the unit purchased. The resolution is 5 to 6 µm (high-res light source unit) or 3 µm (very high-res light source unit, but with slightly less depth of field).
|
Dr. Buckland notes that, because of its mobility and handheld imaging head, the Envisu C-Class is the only OCT cleared by the Food and Drug Administration for the imaging of children down to the prematurity age group and the only one approved for use on anesthetized patients. “It’s cleared for use under anesthesia because it can take images from whatever angle is necessary,” he explains. “It has sufficient ergonomics to allow that sort of imaging without any change to the image quality.”
The Envisu, the standard package of which consists of a lens for retinal imaging and one for imaging the anterior segment, provides images only—no normative data or measurements of normative data. “Our system is really a visualization tool,” says Dr. Buckland. “If one wants to image pathology, understand epithelial and stromal thickness, or determine if a candidate is a good candidate for DSAEK or DALK, our system can show them the detail they need.” For information, visit
bioptigen.com.
Carl Zeiss Meditec
|
• Cirrus HD-OCT 5000 and 500. The 5000 model has a feature called FastTrac, which is retina tracking technology that Carl Zeiss Meditec’s U.S. President and CEO Ralf Kuschnereit, PhD, says serves a twofold purpose: “While the OCT scan is being done, the independent system is tracking the retina,” he says. “And if the patient moves or blinks, this is taken care of, corrected or re-scanned so that there is no motion artifact in the final image. This is especially important for subspecialists who may have patients who find it hard to fixate. The other advantage of the tracking is if you have subsequent scans of different visits, you can position the HD high-resolution raster scan in exactly the same position so that you can better track the progression of the disease.” The tracking can also be turned off for speedier imaging in patients who can sit still, since using the tracking can make an exam longer than not using it. The model 500 doesn’t have FastTrac, but has a much faster OCT scanner than previous models, which the company says makes it easier to align a patient to the system for accurate imaging.
• Cirrus photo 800 and 600. These are both combinations of a fundus camera and Cirrus OCT in one unit. The 800 increases the feature count by also offering fluorescein and indocyanine green angiography capability. “If you want to provide advanced care and need versatility but maybe have a space constraint, you might not want to have a separate fundus camera and OCT,” says Dr. Kuschnereit. “By combining Cirrus OCT images with fundus, angiography or autofluorescence images all on one screen, it’s a great way to review the disease state of the patient.”
The new Cirrus models also offer software to analyze such features as the retinal nerve fiber layer, ganglion cell layer and optic nerve head. Available anterior segment imaging allows analysis of the angle and the cornea. For information on CZM’s new OCTs, visit
www.meditec.zeiss.com/Cirrus.
Heidelberg Technology
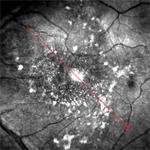
The newest addition to the Heidelberg Spectralis OCT is multicolor scanning laser imaging. Multicolor imaging uses several laser wavelengths (blue, red and green) at the same time to allow the physician to capture and display diagnostic information from different parts of the retina during one OCT exam. “It’s very sharply detailed because the Spectralis is confocal, and blocks light from outside of the focal plane, which allows it to get sharp images,” explains Adam Doherty, Spectralis product manager. “Each laser color goes to a certain depth, giving information from different layers of the retina, with blue being more anterior and red more posterior. The clinician can look at the multicolor image or at each color image separately. The multicolor image is helpful because when you take an image of the fundus and you see blood, cotton wool spots and a vitreous hemorrhage in black and white, sometimes those three things can look very similar. But in multicolor you can see the blood is red and isn’t a cotton wool spot, and the vitreous will be darker and not resemble blood.”
The other feature that’s being manufactured but isn’t released yet is the ultra widefield lens. “The non-contact lens allows the OCT to go out over 100 degrees of the retina,” explains Mr. Doherty. “This makes it easier to get images but also makes getting the images easier on the patient. Normally, a retinal photographer would have to do seven field sweeps, especially for diabetic patients, taking images around the posterior pole with a 30-degree lens, then send the series for studies to get a picture of the whole posterior pole. This lens allows the doctor to perform those sweeps, but now out to the far periphery. This may allow physicians to catch disease states in the periphery, such as choroidal ruptures and retinal tears, earlier. Also, if a physician is going to perform a laser treatment in the periphery, he can use one or two of these images to see where he’s going to do the treatment.” Visit
heidelbergengineering.com or call 1 (800) 931-2230.
Optopol/Canon
| ||||
“Another area where the device’s focusing ability is useful is in the setting of media opacity,” Mr. Chalecki continues. “There are a number of patients with cataract or other media opacities that can block the light from an OCT, making for a diminished signal. This system helps get as much data as possible for the doctor.”
|
Optos
Optos says its OCT SLO helps clinicians make better diagnoses by marrying a confocal scanning laser ophthalmoscope with an OCT. “This generates a fundus image as well as an OCT image,” explains Glenn Erickson, director of North American product specialists at Optos. “What makes the OCT SLO different is that it uses a single light source for the beam that’s sent into the eye, rather than two different ones. This gives us pixel-to-pixel registration on the fly between the SLO and the OCT. So, for the user, the two images, the fundus and the OCT, are registered to each other. Anything the user does to one image, he sees on the other. This is in the hardware, and they don’t need to be married up afterwards in the software. This means you always know exactly where you are in the image. For example, with a macular hole, while scanning through it, because you have the SLO in front of you, you can move your scan line into the hole and you see the OCT on the other side of the screen. It allows you to know whether it’s open or closed, because you’re seeing it on the screen. If you didn’t have this, you wouldn’t know if it were open or closed, because you wouldn’t be sure where you were scanning on the retinal surface during an exam.”
The OCT SLO also has functions for tracking glaucoma progression, though Mr. Erickson says the device does the retinal nerve fiber layer test a little differently. “We use vessel registration and tracking,” he says. “We track back to the same place around the nerve head where the measurement circle was the first time, based on where it was intersecting the blood vessels. This is important because if you’re looking for change you want to go the exact place on the retina—in this case the nerve fiber layer measurement—and look for change over time.” For information, visit
optos.com or call 1 (800) 854-3039.
Optovue
The latest additions to the Optovue line of devices are the Total Corneal Power module and the RTVue VTRAC Premier real-time, active-tracking OCT.
“Total Corneal Power comes in when the surgeon or staff is doing preop IOL calculations in post-refractive surgery patients,” says Mike Scott, senior product marketing manager for Optovue. “Standard keratometry measures the anterior curvature of the cornea and then makes broad assumptions to extrapolate the cornea power to be used in IOL selection. However, in a post-LASIK patient, for example, the anterior curvature has changed, so if you try to use the same assumptions, the surgery may result in an unexpected postoperative surprise. TCP takes a direct measurement of the front surface and a direct measurement of the back surface of the cornea to calculate the anterior, posterior and net cornea powers. Mr. Scott says the surgeon can then take those corneal powers and enter them into a special OCT-based IOL power calculator for eyes with previous refractive surgery that is available at
coollab.net/index.php?id=852.
Though the RTVue system already has vessel registration to allow change and trend analysis, Mr. Scott says that the VTRAC Premier system allows surgeons to get images with even more detail. “It has a scan depth of approximately 3 mm, which gives a larger window into the retina,” he explains. “Combined with its Noise Reduction Technology, the system allows for deep choroidal imaging and measurement, while also providing rich detail in the vitreous. Also, in patients with fixation drift, the real-time, active eye tracking helps capture their images.” The RTVue also has ganglion cell complex analysis, which the company says has been used in more than six years of published studies and clinical use. The GCC and thickness measurements can be compared to a large normative database, as well.
In addition to the RTVue VTRAC Premier, Optovue also offers the iVue, a more compact OCT device. The iVue allows imaging of the anterior segment, posterior pole and optic disc; as well as retinal thickness measurements and optic disk and peripapillary retinal nerve fiber layer assessment. The device’s anterior segment module is offered as standard and provides pachymetric measurements of a 6-mm diameter area of the central cornea, as well as visualization and measurement of the angle. For information visit
optovue.com or call 1 (866) 344-8948.
Topcon
The Topcon 3D OCT combines a high-resolution digital fundus camera with the OCT to give the clinician different views of the retina.
The company says the OCT portion of the exam uses its proprietary FastMap software system to allow dynamic viewing of 2D, 3D and fundus imaging. Topcon says FastMap can help when faced with complex pathologies such as vitreous traction, macular edema and retinoschisis. The software also allows the physician or technician to export its images and 3D movies to other devices for presentation purposes. The OCT system can capture images of the fovea and optic nerve in a single scan, and has a choroid reference mode for providing high-resolution views of the choroid. For capturing exam images of high myopes and hyperopes, the system can work with a diopter compensation lens and can provide an extended scanning depth of 2.3 mm.
By employing a non-mydriatic color fundus camera in the OCT system, clinicians may be able to visualize conditions that might not be picked up on an OCT, such as disc hemorrhages, the company says. The camera has a 45-degree field of view and can also provide stereo photos for analysis of optic disk changes. To help orient themselves to areas of pathology that are displayed in the system, clinicians can use the 3D OCT’s PinPoint Registration to link the location of the OCT data points to specific points in the fundus image.
For following patients with glaucoma or retinal pathology, the FastMap software also uses layer detection algorithms to measure such features as total retinal thickness and retinal nerve fiber layer thickness. The physician or technician can manually adjust the imaging grids that are measured in these exams, and can also manually register serial exams or allow the computer to register them automatically for comparison purposes. For information, visit
topconmedical.com or call 1 (800) 223-1130.
For many ophthalmologists, OCT technology has become an integral part of their day-to-day practice. The new modules and add-ons available on the various OCT devices should help doctors diagnose and manage disease more quickly, and with even more accuracy. REVIEW