When performing refractive cataract surgery, a perfect outcome is always the goal, and the number of patients hitting their refractive target has increased steadily over the years. However, the challenges inherent in operating within a complex, living system have kept the success rate from reaching 100 percent. As a result, surgeons still have to deal with cases of postoperative refractive surprise.
“Tools such as intraoperative aberrometry and better power calculation formulas, like Hill RBF and Graham Barrett’s formulas, have made refractive misses less common,” notes John Berdahl, MD, a corneal, refractive and glaucoma surgeon at Vance Thompson Vision in Sioux Falls, South Dakota, and associate clinical professor at the University of South Dakota. “Nevertheless, today we still enhance 10 to 15 percent of our patients that have a refractive endpoint in mind.”
William B. Trattler, MD, director of cornea at the Center for Excellence in Eye Care in Miami, and a volunteer faculty member at the Herbert Wertheim College of Medicine at Florida International University, agrees. “Refractive surprises are definitely less frequent, but they still do happen,” he says. “Premium IOL patients, in particular, have high expectations. They want to end up on-target.”
When a patient’s outcome isn’t what was hoped for, the surgeon has to make a number of decisions. Is the refractive miss significant enough to require correcting? What, exactly, is the cause of the less-than-ideal outcome? And if I’m going to correct the refractive result, which method makes the most sense for this patient?
Should You Correct It?
“Not all refractive misses have to be surgically corrected,” notes Dean Ouano, MD, a cornea and anterior segment specialist at the Coastal Eye Clinic in New Bern, North Carolina. “Despite advances in optical biometry and IOL formulas, a significant percentage of patients fail to achieve emmetropia. If you look at the Swedish National Registry study published in 2012, 17,000 patients were targeted for emmetropia in cataract surgery, but only 55 percent of them actually achieved it.1 So deciding to correct a refractive surprise is a question of degree. The patient has to be symptomatic, and the refractive miss has to be large enough to justify surgical intervention.
“Deciding to explant or exchange a lens shouldn’t be done lightly,” he continues. “Before you surgically intervene in a refractive miss you have to figure out several things. How big is the miss? Will the patient tolerate the residual refractive error if it’s corrected by spectacles or contact lenses? Have you ruled out any other coexisting problems such as macular disease, ocular surface disease or irregular astigmatism? I think each case has to be examined on its own merits.”
To be certain that you really do need to make a refractive adjustment, surgeons emphasize two points: First, make sure you understand exactly what’s causing the refractive issue. Second, make sure to wait an appropriate amount of time before drawing any final conclusions about the size of the miss.
“There are a couple of things you need to check out,” says Dr. Berdahl. “Is there other pathology going on, such as posterior capsule opacity or a retinal problem? Is the lens tilted? Also, keep in mind that some problems can’t be corrected by adjusting the refraction. Let’s say you implanted a bilateral extended-depth-of-focus lens and the patient’s main complaint is inadequate near vision. Adjusting the refraction isn’t necessarily going to solve that problem. You need to understand the nature of the problem before you try to solve it.”
Bryan Lee, MD, JD, in private practice at Altos Eye Physicians in Los Altos, California, agrees that sometimes the nature of the IOL is the problem. “If the patient’s unhappy after you put in a multifocal or extended-depth-of-focus lens, one of the things you have to figure out is whether the problem is residual refractive error or an optical problem relating to the IOL design,” he says. “Figuring that out may require having the patient wear a pair of glasses or contact lenses to make sure they’re actually happy when the refractive error is corrected. If they are, then laser vision correction makes sense. The main point is that you have to figure out exactly what’s making the patient unhappy.”
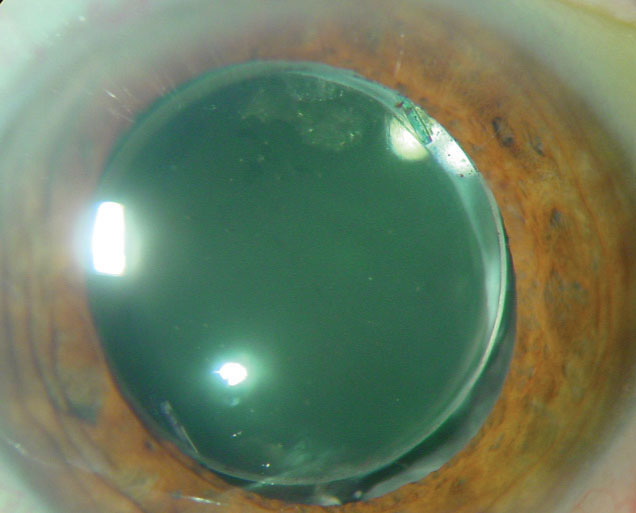 |
|
|
Surgeons also agree that in most cases it’s crucial to wait before making a final determination about the extent of a refractive miss. “I won’t usually make a refractive miss call until three months after surgery, when I feel sure the eye is entirely stable,” says Dr. Berdahl. “You’re probably on reasonably safe ground if you decide as early as three weeks out, but I want the next move I make to be definitive. For that reason, I prefer to wait at least three months for the refraction to settle.”
“It’s important not to make that decision too early,” agrees Dr. Lee. “You need to give the patient at least a couple of weeks to be refractively stable, and some patients may need even more time to get where they’re supposed to be. You don’t want to correct something prematurely.”
Minimizing Alternate Factors
Given that issues besides a refractive power miss can affect vision, and additional surgery should ideally be avoided, you can take several steps to ensure that a surgical adjustment is really necessary.
“One of the things that impacts the final refractive outcome is the ocular surface,” notes Dr. Trattler. “Many patients have mild dry eye or meibomian gland dysfunction before surgery, and those can be worsened by all the drops associated with surgery. That can impact postoperative quality of vision and the refractive error. Eye- care providers can focus on reducing postoperative inflammation, and at the same time treat the underlying ocular surface condition.
“The impact of a condition such as dry eye may not be that obvious, but you’ll be surprised when you treat postoperative patients for dry eye,” he continues. “Some patients may improve enough that they won’t need further surgery to improve their vision—even though you thought they did. For example, let’s say you have a patient who is 20/30 with -0.75 D of cylinder. The patient may say, ‘My vision isn’t what I expected.’ While one might believe the patient’s complaint is due to the small amount of residual astigmatism, further questioning may reveal that it’s actually the result of fluctuating vision caused by dry eye. In my experience, treating dry eye can eliminate 60 to 70 percent of the patients who initially seem to need an enhancement following cataract or lens replacement surgery.
“Make no mistake, patients don’t want to undergo more surgery, so they’ll be happy if you can resolve the problem without it,” he says. “That’s why if the patient is unhappy, my protocol is to first treat for dry eye and meibomian gland disease, even if these conditions aren’t obvious. Increasing tear quality—even if it wasn’t terrible before—can significantly improve their vision.”
Dr. Berdahl agrees. “The first thing to examine and treat is the ocular surface,” he says. “Whatever target you’re shooting for, you don’t want it to be a moving target. As we all know, dryness and ocular surface disease are common in these patients, and those conditions can affect the refraction. If the ocular surface isn’t OK, then we need to treat it and rehabilitate it.”
Dr. Trattler says a second concern is that mild posterior capsular opacification can also impact quality of vision. “Sometimes if we laser the capsule, vision is improved just enough to eliminate the problem,” he says. “The lens may even shift a little bit, changing the refractive outcome a little and improving vision. In some borderline cases, this may avoid any need for fine-tuning.” With this in mind, Dr. Trattler says he routinely performs a YAG when a patient is unhappy with the outcome and he’s planning a refractive surgery enhancement. “Of course, I don’t charge for this because I’m not treating something that’s causing a loss of best corrected visual acuity. But this protocol sometimes makes a real difference.
“The other thing that can happen is, let’s say you don’t YAG and you perform laser vision correction,” he continues. “Three months later the patient’s PCO worsens and they experience capsular contraction, which can shift their refractive error. If you’ve performed a YAG prior to the laser vision correction, the vision is a little bit more stable long-term. Skipping the YAG would be quicker, but we work through all of these steps to make sure we really optimize the patient’s vision. Again, you can’t charge insurance for this without the presence of significant PCO, and I wouldn’t charge the patient either. I just include it as part of the refractive fee because I want to optimize the patient’s vision.
“If you do both things—treat the ocular surface and perform YAG—many patients will be happier with their postoperative visual outcomes,” he concludes. “That’s the protocol I like to follow before moving on to surgical enhancement.”
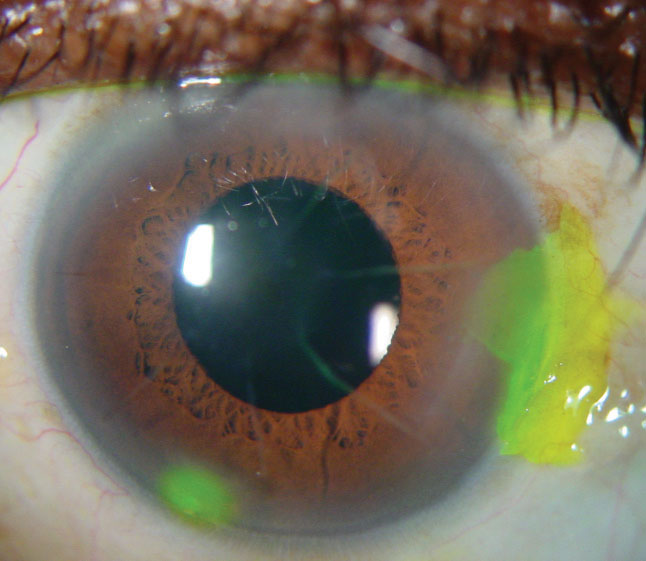 |
|
|
Dr. Trattler explains how this works in terms of timing. “Once it’s clear that a patient is unhappy with his vision following surgery, we first finish the course of postoperative drops and get him through the first month,” he says. “Then we see how he’s doing and re-refract. If he’s still unhappy, then we’ll try to optimize the ocular surface. We initiate dry-eye therapy; if it appears to be meibomian gland disease, we’ll treat with warm compresses, antiseptic sprays for the eyelashes and often a three-week course of a topical steroid. In cases of aqueous-deficiency dry eye, we often start a topical steroid, along with either Restasis or Xiidra, and we may also place punctal plugs. Then we give the patient another month. When the patient returns, we re-refract. We also check the posterior capsule. At two to three months we may do a YAG capsulotomy. After another week or two we check everything again.
“At this point the refraction is relatively final,” he concludes. “This protocol gives the eye time to heal and adjust, and often things have improved enough that the patient is happy. If so, no further correction is necessary.”
Should You Use the Laser?
When choosing a way to adjust the refraction, if you’ve decided that a correction is necessary, the choices can be broadly divided into two categories: IOL-based changes—i.e., replacing the IOL or adding a piggyback lens—and laser refractive procedures.
Deciding whether or not to proceed with corneal laser surgery requires considering numerous factors:
• The size of the adjustment. Dr. Ouano says that if the patient’s spherical error is more than 4 D off in either direction, you should avoid using laser surgery to make a correction. “I think most surgeons would agree that a large refractive miss calls for an IOL-based solution,” he says. “For example, a +4 D hyperopic keratorefractive procedure on an older patient is generally not a good idea. On the other hand, a smaller refractive miss is a gray zone. If the patient is a -2 D myopic miss, you have a lot of options.”
• The direction of the adjustment. “Another thing to take into account is the direction of the refractive error,” notes Dr. Lee. “Lasering someone who is -1 D is easier and more accurate than lasering someone who is +1 D off-target.”
• Accuracy. “A 2013 study in the Journal of Refractive Surgery showed that laser refractive surgery is able to more accurately correct residual astigmatism and refractive errors than an IOL exchange or a piggyback lens,” notes Dr. Ouano.2 “That makes sense, because LASIK and PRK were designed to be accurate. For example, suppose your miss is -3 D sphere and -2 D cylinder. An IOL exchange isn’t going to be very reliable for correcting the cylinder, but a LASIK or PRK procedure could be. In addition, you’d avoid another intraocular procedure.”
• Age of the patient. “The patient’s age has to be considered, because a 75-year-old undergoing LASIK has a much different healing process than a 25-year-old,” notes Dr. Ouano. “Older patients have more ocular surface disease and dry eye.”
Dr. Lee agrees. “Cataract-age patients are older, and they often have a worse ocular surface,” he says. “You have to consider how dry the eyes are and how easily the patient will recover from refractive surgery.”
• Prior laser refractive surgery. “If the patient has had prior LASIK or PRK, I typically wouldn’t want to do further laser correction on that patient,” says Dr. Lee. “Doing PRK over a LASIK flap is less accurate. So in general, if the patient has had laser refractive surgery I’ll do a lens exchange. I think it’s more accurate in that situation.”
• Contraindications. Performing LASIK or PRK on a patient under any circumstances requires that the cornea meet appropriate specifications. “You have to consider the normal contraindications for LASIK or PRK—things like corneal thickness and keratoconus,” Dr. Ouano points out.
• Practical issues, including access to the technology. “Logistics, availability and reimbursement are all issues with PRK and LASIK,” says Dr. Ouano. “For one thing, not every office has access to an excimer laser.”
Dr. Lee agrees. “If you don’t have access to an excimer laser, that may push you towards doing an IOL exchange or piggyback in these situations,” he says. “On the other hand, if you operate in a hospital setting and the cost of doing an IOL exchange is outside of your control, that might push you towards doing an excimer laser treatment. Either choice is probably fine, because clinically, one way isn’t necessarily better than the other.”
Dr. Berdahl says he believes residual refractive error is probably undertreated in general, simply because many surgeons don’t have access to an excimer laser. “If you don’t have access to a laser, you should consider developing a relationship with someone in your community who does,” he says. “Try to work out a system where you either can use their technology, or they’ll do enhancements on your patients for you.”
LASIK or PRK?
If an adjustment by excimer laser seems like the best choice, the next question is whether to opt for LASIK, PRK or another procedure such as SMILE.
“If the patient ends up on the myopic side, I typically perform laser vision correction,” says Dr. Trattler. “We don’t have access to SMILE, but we perform both LASIK and PRK—mostly PRK, although LASIK is certainly an option for myopic or astigmatic fine-tuning.” Dr. Trattler uses epi-Bowman’s keratectomy, performed with a device called EpiClear (ORCA Surgical), which removes the epithelium and collects discarded cells into its tip without touching Bowman’s membrane. Dr. Trattler says that in his experience this is more comfortable for patients than traditional epithelial debridement with alcohol.
Dr. Berdahl says he prefers to do a refractive correction with LASIK rather than PRK. “I think the results are a little bit better in an older population,” he says. “Because these patients are older, their epithelium can be more irregular. Doing a low-correction PRK can unmask that irregular epithelium, leading to more variable results. In fact, epithelial mapping can be very helpful when trying to decide whether you should do LASIK or PRK.
“It’s kind of a conundrum,” he continues. “If the epithelium is very irregular, that might indicate anterior basement membrane disease, which probably should have been treated prior to cataract surgery. But if you’re faced with a very irregular epithelium postoperatively, you should do a superficial keratectomy or phototherapeutic keratectomy and see how it heals; then come back and do LASIK or PRK. If the epithelium is mildly irregular, which is true for a lot of patients, then I’d probably do LASIK. I don’t want to unmask that irregular epithelium with PRK, causing it to be translated into the refractive outcome. If the patient has a very regular epithelium, than either LASIK or PRK is OK.
“I think an irregular epithelium is one of the things that cataract surgeons frequently miss,” he adds. “It’s easy to overlook. I think it’s one of the main reasons surgeons have some dissatisfied patients after receiving a refractive IOL and an enhancement.”
What about using SMILE? “I think it’s too early to tell whether SMILE will be great for refractive enhancements,” says Dr. Berdahl. “What we like about SMILE is that perhaps there’s a little less postoperative dryness—although that may be debatable. The biggest concern with using SMILE to correct a refractive miss is that these are usually very small corrections. Removing a very small SMILE lenticule can be challenging.
“Nevertheless, I think SMILE holds a lot of promise for all things refractive, including enhancements,” he says. “SMILE is a very young procedure, and we’re going to get better at using it as time goes by.”
 |
Laser or IOL-based Correction?
Alternatives to laser refractive correction include an IOL exchange or adding a piggyback lens. Several factors—surgeon preference among them—determine whether an IOL-based change will work better than a corneal laser correction.
Dr. Berdahl observes that some surgeons prefer to go right to an IOL exchange. “That’s reasonable if you’re facile with IOL exchanges,” he says. “That approach can give you good results.” However, Dr. Berdahl says that when he’s considering whether or not to exchange the IOL, corneal stability is a major concern. “If it’s a post-RK patient, I won’t have good laser-refractive-enhancement options,” he notes. “In that situation, I think IOL exchange makes the most sense. That may be true for post-LASIK patients, too, if I’m not comfortable dealing with a previous LASIK flap. Of course, many surgeons don’t have access to an excimer laser, so they’ll do an IOL exchange simply because they don’t have the other option. But if all else is equal, I think in most cases the excimer laser is the most precise way to correct a refractive miss.”
Sometimes if a patient isn’t eligible for the specific laser procedure the surgeon believes will be easiest for the patient, that’s sufficient to cause a shift to an alternative such as IOL exchange. Dr. Lee says that if a patient is a candidate for PRK but not LASIK, he may decide to perform an IOL exchange. “The patient will have a more comfortable and faster recovery with IOL exchange than PRK in many cases,” he explains.
Dr. Ouano says his approach in this situation would depend on the patient’s overall refractive error. “If it was a very large spherical miss, I’d go with a lens exchange, as long as the lens hasn’t been in there too long,” he says. “In early lens exchanges, the bag is more pliable and amenable to exchange.”
Piggyback or Lens Exchange?
If laser correction is off the table, should you opt for exchanging the IOL or adding a piggyback lens?
“A straightforward lens exchange is appealing to me, because you’re going to maintain the desired anatomy of the eye—switching an in-the-bag lens for an in-the-bag lens,” says Dr. Ouano. “You’re not going to have two lenses inside the eye, and you’re not going to disrupt the corneal surface. You can usually use the same entry wound, and it’s a straightforward, safe surgery if it’s done in the early postoperative period, as long as you have an intact rhexis and intact posterior capsule and zonules. An early IOL exchange for a refractive miss after cataract surgery, is, in my opinion, a good procedure. Furthermore, in our experience, the reimbursement pathway for an IOL exchange after a refractive miss is also straightforward. So if there’s a refractive miss following cataract surgery my preference is to do an IOL exchange during the early postoperative period.”
Dr. Ouano says he doesn’t favor the piggyback option, although some surgeons in his practice prefer it. “I understand why they like it,” he says. “Number one, it’s technically easy to do. Two, selecting the lens implant is easy to do because it’s based on the postoperative refractive error. Three, the reimbursement pathway is reasonable. The financial barriers are not as insurmountable as they can be if you do a LASIK procedure on a 75-year-old patient. So the piggyback option has some advantages.
“However, I think the disadvantages are also significant,” he continues. “The patient might have a very shallow anterior chamber, in which case there’s a real possibility of iris chafing, pigment dispersion or UGH syndrome. And a big downside is that we don’t have a lot of choices for a sulcus-fixated IOL in the United States. We currently have two silicone three-piece lenses for the plus powers: the Bausch + Lomb Sofport LI61AO and the Tecnis Z9002. There are minus-power lenses from Johnson & John-son Vision within a certain range. But the lack of an ideal sulcus-fixated IOL is a disadvantage for the piggyback option.
“The biggest problem,” he adds, “is that if you have a large myopic miss—let’s say -9 D—you’re not going to solve that with LASIK or PRK, and you can’t get an IOL that high. You can use an implantable contact lens off-label; they come in powers up to
-16 D. But it raises a big financial issue: Who pays for the ICL? It’s quite a bit more expensive than a standard IOL. So piggybacking in that situation isn’t a good option.”
Dr. Ouano admits, however, that if you’re contemplating a lens exchange instead, timing is a major concern. “Opening a capsular bag late, let’s say six months to a year after the surgery, is more difficult,” he notes. “There are risks involved, depending on the status of the zonules and the posterior capsule, so exchanging the lens isn’t necessarily a slam dunk. It’s not impossible, but it’s more difficult to manage.”
Dr. Lee says that in his experience implanting a piggyback lens usually works well. “Calculating the power is straightforward, and the procedure is straightforward as well,” he says. “However, not every patient can tolerate a piggyback lens, depending on the anatomy of the anterior segment. That’s not totally predictable, so if you put in a piggyback IOL, sometimes it will have to come out later. If I’m planning to use a piggyback lens, I’ll always mention preoperatively that occasionally these piggyback lenses have to be explanted. Fortunately, it’s very straightforward to remove a piggyback IOL.
“I think in general a piggyback lens is a good way to correct refractive error,” he continues. “Again, it depends on the clinical situation. You might have a patient with bad zonules, or one who’s uncooperative during the surgery. Factors like these might push you towards thinking about implanting a piggyback lens instead of performing an IOL exchange, but the anatomy will still be a factor. Just a few weeks ago I had a patient who’d had prior LASIK and was off-target. That patient had already had a YAG laser, so I didn’t want to laser or do an IOL exchange. I did a piggyback, and he’s done very well so far.”
Dr. Trattler says he doesn’t often exchange IOLs. “If the patient’s hyperopic, I prefer to implant a piggyback lens,” he says. “Implanting a piggyback lens is very simple. You make a tiny incision, insert the lens, put Miochol in the eye, and you’re done. It’s very fast and patients have very good outcomes. In contrast, if you have to free-up an IOL, bring it into the anterior chamber, bisect it with scissors inside the AC, remove the IOL fragments and then place a second lens inside the capsular bag, there’s a little more surgery and risk. Of course, you may have to perform an exchange if you implanted a toric lens with the wrong astigmatic power, or the patient is unhappy with the glare and haloes caused by a multifocal lens. But if everything’s fine other than the patient being a little hyperopic, then a piggyback lens can work very nicely.”
Dr. Trattler adds, however, that he generally reserves the piggyback option for refractive surprises that are significantly hyperopic. “For myopia, PRK and LASIK are very effective,” he says. “If we’re talking about 1.5 D of hyperopia or higher, laser vision correction has been a little underwhelming. Of course, if it’s a hyperopic refractive surprise of 0.5 or 0.75 D,
then LASIK or PRK is fine. But if more than 1 D of treatment is needed, I’ll typically use a piggyback lens.”
Some General Advice …
Surgeons offer these suggestions to help things go smoothly:
• First, let the patient know you’re on the case. “When you have a refractive surprise, be sure the patient knows that you care about this, and that you’re going to work to get them where they want to be,” says Dr. Berdahl.
• Don’t shy away from rotating a misaligned toric IOL. Dr. Lee notes that whether or not a toric lens rotational adjustment should be made in a borderline case depends on numerous factors. “If someone has a very high-powered toric lens implanted, like a T6, and the lens is 7 degrees off, that patient’s vision will be affected a lot more than a patient who has a T3 lens but is rotationally further off-target,” he says. “So it depends on the clinical situation—as well as the patient’s personality.
“I know that some surgeons hesitate to go back in to rotate a toric IOL,” he adds. “Aside from having to re-enter the eye, you’re telling the patient that you want to take him back to the OR, and there could be a cost associated with it, depending on whether you operate in a hospital or in a surgery center where you have more control. But surgically it’s not too difficult to rotate a lens, as long as you’re doing it within three or four weeks after the initial surgery. It’s pretty straightforward, and it can help the patient.”
• Keep the lines of communication open. “Be sure to continue to communicate with the patient postoperatively, especially if the patient is unhappy,” says Dr. Lee. “You have to take the initiative to follow-up and keep the communication lines open so you have as good a relationship as possible.”
• Perform a trial correction before proceeding. “Before I actually perform the procedure, whether it’s PRK, LASIK or a piggyback lens, I typically have the patient undergo a contact lens trial to demo what their corrected vision will be like,” says Dr. Trattler. “Patients often assume that altering the outcome won’t change the parts of their visual outcome they already like, which isn’t the case.
“For example, let’s say we have a patient who ends up a little on the nearsighted side,” he continues. “They have good computer vision and reading vision, but they want better distance vision. I’ll have them demo a contact lens to make sure this change in their vision is really what they want, because if they realize what the trade-off is—getting better distance at the expense of near—they may decide they don’t want to have the refractive outcome adjusted after all. That’s why a contact lens trial prior to performing an enhancement is helpful. That trial educates the patient about what to expect.”
“When the patient has a presbyopia-correcting IOL, I wouldn’t make any decision about how to proceed without correcting the refractive miss first,” says Dr. Lee. “This can be done with a pair of glasses or contact lenses. I’ve had many unhappy patients referred to me two or three months after surgery who had never tried a pair of glasses. That’s kind of the first step in figuring out what to do: Correct the residual refractive error. Sometimes if you give them a pair of glasses they’re so happy they can see clearly that they don’t want anything else. And if they still want to have their refractive error corrected, this gives you confidence that the thing that’s making them unhappy really is the refractive error.”
Sometimes the refractive miss is very small, but the patient is still unhappy. “Suppose a patient ends up +0.25 -0.5,” says Dr. Berdahl. “The first thing I want to do in that situation is simulate the adjustment I’d be making, using glasses or contact lenses. The glasses might take the patient from 25/25+1 to 20/15 solid. The patient may put the glasses on and say, ‘Yes, this is what I want.’ In that case, I’ll do the enhancement. But I want to simulate the adjustment first to make sure I’m not doing unnecessary surgery.
“We do a fair number of those simulations,” he adds.
• Take the age of the patient into account. “I would definitely perform a refractive correction on younger patients in their 40s and 50s,” notes Dr. Trattler. “Those patients have very high expectations, so if we’re off-target with one of these patients, we follow our process. We treat their dry eye, perform the YAG capsulotomy, then undergo a contact lens trial, and finally perform the refractive enhancement. As far as which option to use for the adjustment, younger patients are eligible for all of the options; any of them are appropriate.”
Dr. Berdahl notes that—for better or worse—older patients seem more willing to accept imperfection than younger patients. “In general, I find that older patients are easier to work with than younger patients,” he says. “They’ve had a number of procedures over the course of their lives, and not all of them have turned out perfectly. As a result, they’re more willing to accept imperfection than younger patients who haven’t been through multiple diagnoses and medical treatments.”
It’s All Good
Surgeons note that the good thing about most instances of refractive surprise is that multiple corrective options will work, giving the surgeon some leeway.
“The good news is that all of the technologies available to us—IOL exchange, piggyback lens and laser refractive surgery—can be used in almost any refractive-surprise situation,” says Dr. Trattler. “So although I have my own preferences, I wouldn’t fault someone who has a different preference. If a surgeon wants to use a piggyback lens on a -2-D patient, that’s OK. If you want to do PRK on a +1.5-D patient, that could also work. It’s not like anything is set in stone. The bottom line is that we’re using a variety of technologies and procedures to make our patients happy.” REVIEW
Dr. Trattler has consulted for VISX, Johnson & Johnson Vision, ORCA Surgical and Bausch + Lomb. Dr. Berdahl has consulted for Astigmatismfix, Alcon, Johnson &
Johnson Vision, Bausch + Lomb and RxSight. Drs. Lee and Ouano report no financial ties to any product discussed.
1. Behndig A, Montan P, Stenevi U, Kugelberg M, Zetterström C, Lundström M. Aiming for emmetropia after cataract surgery: Swedish National Cataract Register study. J Cataract Refract Surg 2012;38:7:1181-6.
2. Fernández-Buenaga R, Alió JL, Ardoy ALP, et al. Resolving refractive error after cataract surgery: IOL exchange, piggyback lens, or LASIK. J Refract Surg 2013;29:10:676-683.



