Researchers in refractive surgery truly offer a potpourri of studies at this year's ARVO meeting, investigating everything from new ways to measure the thickness of the LASIK flap to a study of the aberrations associated with 20/9 vision, and what that data might mean for our custom procedures. To find out more about these and other intriguing studies, read on.
In a prospective study, researchers analyzed the effect of conventional LASIK on night-driving performance using a night-driving simulator.
In the study, the doctors analyzed 75 subjects before and six months after conventional LASIK with one of four different laser systems. The patients and their surgeries broke down like this:
• 21 patients (41 eyes) with the Alcon LADARVision 4000;
• 18 patients (36 eyes) with the Bausch & Lomb Technolas 217;
• 18 patients (36 eyes) with the Nidek EC-5000;
• 18 patients (36 eyes) with the Visx Star.
Laser-group treatments (sphere, cylinder and manifest refraction) were similar (ANOVA, p>0.7).
The patients were then tested on a night-driving simulator designed by Vision Sciences Research Corp. (San Ramon, Calif.), which allowed surgeons to measure the distances at which patients could detect, then identify, two different road signs and a pedestrian on a rural road at 55 mph.
The researchers found significant differences between the four lasers in terms of night-driving performance. Performance was unchanged for the Visx, slightly reduced for LADARVision, reduced for the Technolas and most reduced in the Nidek group (ANOVA, a=0.05). In the Nidek patients, the average reduction in performance ranged from -29.5 feet to -40.7 feet for detection without glare to identification with glare, respectively.
The change in performance wasn't significantly determined by the type of road hazard (traffic, business sign or pedestrian) or which eye was used. Contrast sensitivity (photopic 5-percent contrast acuity), intensity of treatment (i.e., the extent of myopia) and subjective night glare/halo complaints were all associated with the change in visual performance during the simulation.4344
Surgeons report good initial results in topography-guided LASIK in the treatment of patients with visual complaints after their initial LASIK.
The researchers used the topography-guided LASIK system from WaveLight to treat 17 patients with small and decentered optical zones, as well as vision-quality problems such as glare, halo, loss of contrast sensitivity and night-vision difficulty. The average preop refractive error was -3.5 D (r=plano to -5.5 D). Average preop astigmatism was -3.75 D (r=-1.25 D to -4.75 D) and the average preoperative uncorrected acuity was 20/200.
 |
| Surgeons report promising results with topography-guided LASIK for treating eyes with postop refractive surgery complaints such as glare and halo. |
The researchers say that the topography-guided LASIK appears to be safe and effective in these patients. They note that it required little central tissue removal and could be an effective first stage of a two-step procedure, with the second part being a spherical adjustment.4365
A surgeon from Greece will relate his 12-month experience with epi-LASIK.
The researcher treated 25 consecutive myopic eyes with and without astigmatism with epi-LASIK. The mean preop sphere was -3.08 D (r=-0.25 D to -6 D). The average preop cylinder was -0.80 D (r=zero to -4 D). He created the epithelial flaps with the newly FDA-approved Moria Epi-K device, and performed the ablations with the WaveLight Allegretto Eye-Q excimer laser.
At one year postop, the mean uncorrected acuity had improved from 20/200 to 20/23. Eighty-nine percent of eyes were within ±0.50 D of the intended target. No eye lost more than two lines of vision. The epithelium stabilized, on average, at day five, and patients graded their discomfort as 2.5 on a scale of 1 to 5 (5 being the most pain). Higher-order aberrations increased by an average of 36 percent. The researchers didn't report on the level of haze, if any, in the abstract.4369
Surgeons at the Mayo Clinic College of Medicine in Rochester, Minn., say that, over a five-year span, nerve-fiber bundles return to the sub-basal corneal layer more slowly in LASIK eyes than in those that have undergone PRK.
The surgeons performed LASIK on 16 eyes of 11 patients using 180-µm flaps to correct errors between -2 D and -11 D. Eighteen eyes of 12 patients received PRK for errors ranging from -1.5 D and -5.75 D. They examined the corneas with confocal microscopy before surgery, then at one, two, three and five years postop. They traced the sub-basal nerves and their branches, and measured their lengths with a computer program. Nerve density was expressed as length of nerve per unit area (µm/mm2). The surgeons determined differences between pre- and postop nerve densities with generalized estimating equation models with Bonferroni correction for four comparisons, in order to account for possible correlation between paired eyes.
They found that PRK patients' corneas demonstrated a faster recovery of the nerves. Their findings appear in Table 1.4371
|
Table 1. Sub-Basal Nerve Density Post-Refractive Surgery |
|
Surgey Type |
Preop |
1 year |
2 years |
3 years |
5 years |
|
PRK |
6,786 |
2,764 |
6,242 |
N/A |
5,903 |
|
LASIK |
5,589 |
2,745 |
3,661 |
3,683 |
4,441 |
Patients with visual problems and thin corneas following PRK can be helped by PTK as an alternative to penetrating keratoplasty, says a group of researchers from Italy, Switzerland and the United States.
The doctors retrospectively studied 48 eyes that were treated for complications after PRK (the researchers didn't specify the complications in their abstract). In all of the eyes, greater than 200 µm of stroma had already been ablated. The average pre-PTK best-corrected acuity was 20/100, the average spherical equivalent was -2.53 D ±2.34 D, and the average pachymetry was 390 µm ±38 µm. The surgeons performed the PTK with a Nidek EC-5000 laser, aided by the use of a masking agent and topography. They followed the eyes for five years.
One year after the PTKs, the average best-corrected vision was between 20/32 and 20/40 (0.6 in decimal refraction), the average spherical equivalent was -2.15 D ±1.67, and average pachymetry was 341 µm ±40 µm. At five years, average best-corrected vision was around 20/30 (0.7 in decimal notation), average spherical equivalent was -2.33 D ±1.12 D, and average pachymetry was 339 µm ±48. Best-corrected acuity improved by at least four lines in all eyes, and there were no significant differences between refraction and corneal curvature between the first and the fifth years. No eye developed ectasia.4647
In a prospective, multicenter study, surgeons from Washington's Walter Reed Army Medical Center and San Diego's Naval Medical Center pitted wavefront-guided PRK against custom LASIK, as well as custom procedures vs. conventional ones.
Forty-two PRK patients and 20 LASIK patients underwent surgery with the Alcon LADARVision system, receiving wavefront-guided treatments in their dominant eyes and conventional treatments in their non-dominant ones.
At the six-month follow-up point, there was no difference in uncorrected acuity or high-contrast, best-corrected acuity between the treatment groups. The photopic 5-percent contrast acuity improved by a mean of 0.02 logMAR units after both custom PRK and custom LASIK, compared to an average decrease of 0.03 logMAR units for both conventional procedures. The net difference in postop 5-percent contrast acuity between the custom and conventional groups was half a line. Of the four procedures, only custom PRK improved mesopic 25-percent contrast acuity (improving it by 0.02 logMAR).4335
Surgeons from Saudi Arabia report 18-month results with laser-assisted sub-epithelial keratomileusis in a large group of patients who had been deemed unfit for LASIK.
|
|
|
Surgeons report good results withLASEK on corneas unfit to undergo LASIK. |
• thin cornea (29 percent);
• low residual corneal thickness (23 percent);
• high keratoconus index (16 percent);
• presence of a posterior "hot spot" on topography (14 percent).
Their surgeries were done with the Bausch & Lomb Keracor 217z laser, their mean age was 30 years, and their average preop spherical equivalent refraction was -4.41 D (r=-1 to -12.5 D). The average preop corneal thickness was 529 µm (r=482 to 637 µm) and mean ablation depth was 82.25 µm.
After LASEK, the spherical equivalent was within ±1 D of the target in 200 eyes (96 percent) and within ±0.5 D in 148 eyes (71 percent). One hundred seventy eyes (82 percent) achieved the level of their preop best-corrected acuity with their postop uncorrected acuity, and 29 (14 percent) were within one line of this mark. After six months, 80 percent of the eyes had no corneal haze, while 12 percent had minimal haze and 8 percent had mild haze. Twelve percent reported no pain in the first day postop, 68 percent reported mild pain and 3 percent had severe pain. The mean postop corneal thickness was 417 µm (r=320 to 615 µm) and the average postop posterior surface elevation was 46.24 µm.4342
Flap Investigations
At ARVO, researchers from the Cleveland Clinic will report on the refractive outcomes, complications and flap characteristics of their first 200 cases of LASIK in which the flaps were made with the Intralase Pulsion laser.
Ninety-six percent of the patients had a best-corrected acuity of at least 20/20 postop, and only one patient lost one line of acuity. The flaps were thicker than intended, with a low standard deviation (±16.48 µm). There were excimer laser eye-tracking difficulties in 11 percent of the patients, 19 percent had peripheral diffuse lamellar keratitis postop, 36 percent had mild flap edema, and 23 percent had epithelium in the interface.
The researchers note that though the laser was efficient and provided good refractive outcomes, surgeons need to be aware of the late visual recovery, high rates of flap edema, DLK and tracking issues they experienced.4649
Investigators for Carl Zeiss Meditec say they've developed a non-contact, rapid, repeatable way to use high-speed optical coherence tomography to measure LASIK flap thickness postoperatively.
The corneal and anterior segment OCT system (CAS-OCT) maps the cornea with 8-mm radial lines (256 A-scans) on four meridians centered on the apex reflection. Map acquisition time is half a second.
The researchers used the device on 27 eyes undergoing LASIK (with either a Hansatome or an Intralase flap), scanning the eyes at one day and one week postop. They divided the corneal maps into central (r= <1 mm), pericentral (r=1 to 2.5 mm) and transitional (r=2.5 to 3.5 mm) zones for analysis.
The flap interface was best detected in the pericentral zone; the researchers needed to use interpolation in the central and transitional zones, in which an axial-scan flap measurement was derived from the more reliable axial scans on either side of it. The flap thickness results appear in Table 2. Researchers say the OCT's repeatability is 7 µm in the central and paracentral zones.
|
Table 2. One-Week Flap Central Thickness Measurements |
|
Method |
OCT |
Ultrasound |
|
Hansatome |
148+17 mm |
118+18 mm |
|
Intralase |
158+10 mm |
160+19 mm |
The study doctors say high-speed OCT flap thickness measurements may be valuable for planning LASIK enhancements and characterizing microkeratome performance.1077
Miscellaneous
Surgeons from the University of Chicago say that clear-lens extraction/intraocular lens implantation performed in patients with low to moderate hyperopia preserves contrast sensitivity at a higher rate than LASIK.
The surgeons performed a retrospective review of consecutive patients with mild to moderate hyperopia (+1 D to +6 D). The group consisted of 50 hyperopic LASIK eyes (26 patients), and 50 eyes (25 patients) with hyperopic CLE/IOL.
In both the LASIK and CLE/IOL groups, postop uncorrected acuity was 20/40 or better in all eyes, with a median value of 20/25 (r=20/20 to 20/40). In the LASIK group, postop spherical equivalent was +0.12 D (-0.75 D to +0.75 D), compared to the preop level of +2.75 D. In the CLE/IOL group, postop spherical equivalent was +0.155 D (-0.75 D to +0.75 D), compared to a preop level of +3.59 D. Contrast-sensitivity curves were decreased by two or more lines in only two CLE eyes (4 percent) compared to seven LASIK eyes (14 percent).4361
A group of researchers says that collagen cross-linking treatment using a combination of riboflavin and ultraviolet light may be an effective way to stabilize the progression of keratoconus by reducing corneal elasticity, though further study is needed.
In a prospective, non-randomized pilot study, the physicians treated 27 eyes of 22 patients with moderate to advanced keratoconus. After creating a central corneal abrasion, they applied photosensitizing riboflavin drops to the eyes, and then exposed them to UVA (370 nm, 2 mW/cm2) from a distance of 2 cm for half an hour.
all the eyes, the researchers say the progression of the keratoconus appeared to stabilize over six months. In 12 eyes, there was a reduction of maximal keratometry readings and refractive error by 3.01 D and 2.14 D, respectively. There was no change in corneal or lens transparency, endothelial cell counts or intraocular pressure. Corneal elasticity measurements, as measured by a contact ultrasound device, diminished on average from a more elastic 1.9 (r=1.6 to 2.5) preop to a more stiff 1.2 (0.8 to 1.8) postop. Visual acuity was slightly improved in 15 eyes (65 percent).
Though the treatment appears to offer promise, the researchers say long-term results are necessary to evaluate the duration of the stiffening and to exclude any side effects.4964
Surgeons from the Jules Stein Eye Institute in Los Angeles advise caution when creating a custom nomogram for wavefront-guided LASIK, at least with the Alcon CustomCornea system, as pupil size and spherical aberration can affect the wavefront refraction.
The surgeons performed a retrospective chart review of 74 eyes of 42 patients who underwent wavefront-guided LASIK for myopic astigmatism using the CustomCornea aberrometer and the LADARVision 4000 laser. They recorded pre- and postop manifest refractions and wavefront refractions and root mean square values for spherical aberration across 3-mm,
4.5-mm and 6-mm pupils.
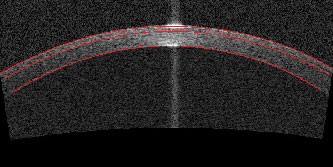 |
| An OCT image of a post-LASIK cornea with lines demarcating the anterior cornea, flap and posterior cornea. The cornea is 474-µm thick with a flap thickness of 135 µm. |
The surgeons say that, because of their findings, others who want to create their own nomograms may need to include pupil size and spherical aberration in their calculations in order to get the best outcomes.4652
Researchers from Spain have made the interesting observation that patients with unusually sharp natural visual acuity may actually have more higher-order aberrations than those with less-acute vision.
The physicians selected a group of 27 patients with excellent natural vision ranging from 20/9 to 20/12. They included another group of 33 normal eyes with visual acuity levels ranging from 20/12 to 20/22 to use as a visual-acuity reference point.
They found that the eyes with unusually good vision had similar amounts of higher-order aberrations to those in the reference group, as expressed in RMS. They didn't find any particular Zernike term (up to the fifth order) with a significantly different value in the better-vision group compared to the reference normals. There was no correlation between high-order aberrations and visual acuity, though astigmatism was correlated with worse acuity when the two groups were combined for analysis.
Within the high-acuity group, the eyes with the best acuity (20/9) actually had a higher RMS value for their aberrations (0.2 µm) at the 6-mm pupil size than many of the other eyes (RMS: around 0.1 µm) with lower acuities (in the range of 20/14).
The researchers say that, since excellent visual acuity can apparently occur naturally in eyes without diffraction-limited ocular optics, it's possible that aiming for a perfect, aberration-free wavefront target with custom refractive surgery may not be the best option for patients. They add that researchers should study the other factors that affect visual performance in eyes with excellent vision, such as optical and neural factors.3615
Dr. Probst is in private practice, and is the Chicago-land regional medical director for TLC Laser Eye Centers.
*Reference numbers noted as footnotes correspond to the abstract numbers in the 2005 ARVO program.




