The most expensive camera in the world is only as good as the lens that's on the front of it, and the same can be said for corneal transplants. You could have a healthy graft, but if the graft's shape isn't conducive to good vision, then the graft is of virtually no use.
This idea is readily apparent when faced with astigmatism post-penetrating keratoplasty; the average post-PK cylinder is 4 to 6 D.
Here's a review of your options for correcting this postoperative error, and a look at the success my colleagues and I have had using surface ablation in these patients.
Correcting the Astigmatism
Before initiating another surgery, the simplest way to manage the patient's astigmatism is selective suture removal. With this method, we remove sutures that are causing a certain amount of astigmatism, let the patient's cornea remold itself over the ensuing weeks, then bring the patient back to check the astigmatism. However, if we remove all the stitches and the patient still has considerable astigmatism (3 D or more), we move on to rigid gas permeable lenses. RGPs can be useful for some patients, but there are still those who can't wear them due to their level of astigmatism or their lack of dexterity. Some older patients simply can't insert these lenses on their own.
At this stage, if the patient can't wear or deal with RGP lenses, I'll talk to her about laser vision correction (discussed in more detail below). However, some patients can't afford refractive surgery or don't want to have it. In such cases, I'll discuss relaxing incisions.
Relaxing incisions are paired incisions placed 180 degrees apart, either in the graft or in the graft/host junction. When placed in the steep meridian, they'll flatten it to some degree. Unfortunately, all of the usual nomograms for relaxing incisions don't apply in transplant patients, and every patient has a different wound-healing response that will alter the effectiveness of the incisions. Though they can correct anywhere from zero to 15 D of astigmatism, their results may be unpredictable in the post-PK patient. (The main complication to watch for when performing relaxing incisions is a corneal perforation. If a perforation occurs, a suture should manage it well, however.)
The counterpart to relaxing incisions is compression sutures. With this management approach, a tight stitch is placed in the flat meridian to steepen it. Some surgeons may even place a pair of relaxing incisions in the steep meridian and a pair of compression sutures in the flat meridian, thereby correcting higher values of astigmatism than either method could do alone.
The Laser Options
For patients with considerable astigmatism who can't tolerate RGPs, refractive surgery may be more predictable than making relaxing incisions. Here are the issues to consider.
• Reimbursement. When discussing the refractive surgery option with post-PK patients, it's important to let them know that they may have to pay for the refractive procedure out of their own pockets, even though they're not the usual elective refractive surgery patient. We always try to get the procedure pre-approved by the patient's insurer, explaining that it's medically necessary due to the patient's inability to wear or handle RGPs; however, insurers will often deny payment and still deem the surgery elective.
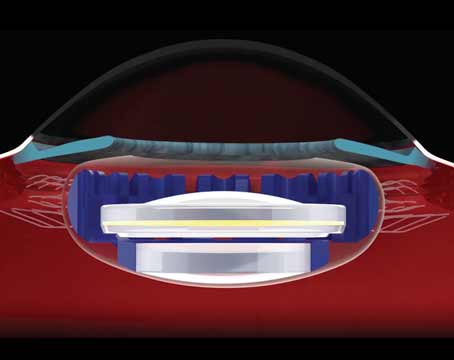
• LASIK. A surgeon who wants to perform LASIK over a PK has to wait 12 to 17 months in order to decrease the risk of graft dehiscence that can occur during flap creation. The risk of dehiscence is the main reason I prefer to perform surface ablation in these patients. The other risk is that of epithelial ingrowth beneath the flap.
The other issue to consider is the staging of the LASIK. Some surgeons do a "one-step" procedure in which they create the flap and perform the laser ablation at the same sitting.
There's another camp, however, that performs "two-step" LASIK, in which the surgeon makes the flap, lays it down, and then waits about three months before performing the refractive ablation. The theory behind the two-step approach is that the creation of the flap itself corrects some astigmatism, so to perform an ablation immediately afterward might be akin to aiming at a target that's moved since you last tracked it. The two-step surgeons follow the changes in the refraction over those intervening three months, and then use the astigmatism value measured at the end of that time period as the target of the ablation.
• PRK. Since I prefer to avoid creating a flap in post-transplant patients and risking a graft dehiscence, I use surface ablation. I also like that PRK gives me more tissue to work with than LASIK, since the creation of a flap isn't necessary, which can be helpful for high amounts of astigmatism. However, for years, surgeons have avoided performing PRK in PK patients because it was associated with regression and haze. The incidence of haze after PRK in the PK patient was found to be 37 percent in one study.1 It also has the usual surface ablation issues of pain and a slower visual recovery when compared to LASIK.
Currently, however, we've been able to surmount problems with haze and regression through the use of mitomycin-C immediately after the ablation. Several studies have found prophylactic mitomycin-C useful in PRK patients,2-4 and one found success with it in surface ablation post-PK.5 In the study of surface ablation and mitomycin-C post-PK, the researchers reported a clear cornea six months post-treatment.
In a study in my previous practice, we performed PRK to correct astigmatism in 15 post-PK patients and then followed it with a 20-second application of 0.02% mitomycin-C delivered with a corneal pledget soaked in the drug. We then removed the pledget and rinsed the corneas thoroughly with BSS. At a follow-up ranging from one to 34 months, (mean: 13 months) the patients all had improvements in uncorrected and best-corrected acuity, a reduction in their manifest and topographical cylinder, improvement in their spherical equivalent refractions and, most important, clear corneas.
Postop, these patients may or may not need more steroids than the typical PRK patient.
This usually takes the form of simply adding to the doses they're already taking due to their post-PK status. Altogether, I want them to be instilling four steroid drops per day for about three months, if the IOP allows, and I'll taper the steroids over the following months to their usual post-PK regimen. I will continually monitor for haze formation and adjust the steroid drops appropriately.
In terms of programming the laser for the post-PK ablation, we usually use the manifest refraction. However, if the patient has more astigmatism when imaged topographically, we'll usually treat a bit more than what appears on the MR. There's no hard-and-fast rule on how much to treat in these cases. We just base it on our experience and the individual patient.
Also, since many of these patients have more than the U.S. Food and Drug Administration-approved treatment level of astigmatism, we may need to break up the treatment into two sessions. Because of this, during the preop discussion you must make the patient aware that she may require two treatments, and that treating this degree of refractive error is an off-label use of the laser.
Dr. Skeens is an assistant professor of ophthalmology at the Medical University of South Carolina in
1. Bilgihan K, Ozdek SC, Akata F, Hasanreisoðlu B. Photorefractive keratectomy for post-penetrating keratoplasty myopia and astigmatism. J Cataract Refract Surg 2000;26:11:1590-5.
2. Anbar R,
Photorefractive keratectomy with mitomycin-C for consecutive hyperopia after radial keratotomy. Cornea 2009;28:4:371-4.
3. Evaluation of the prophylactic use of mitomycin-C to inhibit haze formation after photorefractive keratectomy. Carones F,
4. Bedei A, Marabotti A, Giannecchini I, Ferretti C, Montagnani M, Martinucci C, Barabesi L. Photorefractive keratectomy in high myopic defects with or without intraoperative mitomycin C: 1-year results. Eur J Ophthalmol 2006;16:2:229.
5. Solomon R, Donnenfeld ED, Thimons J, Stein J, Perry HD. Hyperopic photorefractive keratectomy with adjunctive topical mitomycin C for refractive error after penetrating keratoplasty for keratoconus. Eye Contact Lens 2004;30:3:156-8.