Point—A SMILE is My Greatest Asset
In life, when you find something that works, you stick with it. Maybe it’s a restaurant that never fails to deliver a good meal, or an automobile brand that’s never let you down. For me, it’s the SMILE procedure. For several years now, SMILE has been the predominant refractive procedure in my practice, comprising 98 percent of our surgeries. We’ve chosen it simply because of its great outcomes and good safety profile, even when compared to LASIK. Here, I’ll tell you what we like so much about it.
 |
SMILE: The Benefits
From the surgery itself through the postop period, small-incision lenticule extraction has many things to recommend it:
• Fewer variables. Air quality. Temperature. Humidity. Tears. BSS irrigation. All of these variables come into play when you’re performing LASIK, and they can negatively affect your refractive outcome.1 With the SMILE procedure, however, they don’t matter nearly as much. This simplifies the procedure for the surgeon so he can focus on the things that do matter. With SMILE, you simply dock the laser with the suction ring, activate the suction and let the femtosecond laser perform the photodisruption in the cornea independent of these factors.
• Potential optical benefits. Since SMILE involves directly cutting a lenticule within the cornea, you have the opportunity to achieve better optics postoperatively. In excimer-laser surgery, however, there’s some eccentricity to the ablation when the laser hits peripheral positions, and this eccentricity can affect the refractive outcome. SMILE directly cuts the tissue because you’ve drawn the cornea into the patient interface; therefore, in theory, you have a more reproducible lenticule removal.
In terms of postop vision, in the FDA trial of SMILE, none of the 328 patients saw 20/40 or better uncorrected preop. At the six-month visit, however, 98 percent (327 eyes) and 88 percent (287 eyes) saw 20/40 or better and saw 20/20 or better, respectively. Results at the 12-month follow-up were similar. The manifest refraction spherical equivalent was within ±1 D of target in 98 percent of eyes. No fewer than 79 percent of eyes were within ±0.25 D, and 92 percent were within ±0.5 D of target from one week to 12-months postop.2
• Preservation of corneal nerves. With SMILE, the incision is smaller than LASIK’s; creating a LASIK flap involves a large incision that extends almost around the entire cornea. This large incision has the potential to influence, for a while at least, the sensitivity of the cornea—especially the nerves in the anterior cornea. In SMILE, however, the patient has better corneal sensitivity postop and less of a reduction in reflex tearing.
Though we haven’t compared SMILE directly to LASIK, we did perform a study comparing it with femtosecond refractive lenticule extraction—FLEX—which involves creating a full flap similar to a LASIK flap while creating a lenticule. We performed SMILE in one eye and FLEX in the fellow eye. When we subsequently measured sensitivity and measured corneal nerve endings using confocal microscopy, after six months we found that SMILE has an advantage in terms of better preservation of nerves and less of a reduction in corneal sensitivity. We didn’t find a change in the composition or quantity of the tears.3
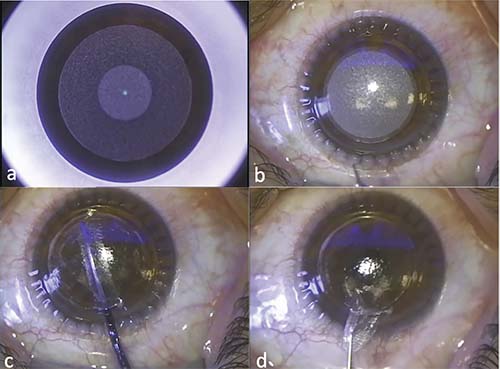 |
| Steps of SMILE. A: The posterior refractive side of the lenticule has been cut and the cap-cut is almost half done. B: Immediately after completion of the lenticule cut by the femtosecond laser. C: Manual dissection of the anterior and posterior side of the lenticule. D: The intrastromal lenticule is being removed with forceps. |
• Retained corneal strength. Also, in theory, since you create a corneal cap in SMILE—not a flap as in LASIK—this should result in a stronger corneal stroma postop. Over the long term, having a small incision rather than a flap reduces the risk of flap slippage if the patient suffers even a small ocular trauma, because flaps can be dislocated even years postop. In a contralateral-eye study in which I participated (N: 10 eyes of 5 patients), we found that flap-based lenticule extraction produced a 49 percent greater reduction (range: 2 to 87 percent) in effective stromal collagen fiber stiffness within the flap region than SMILE procedures in the patients’ fellow eyes. There were also lower stresses and deformations in the residual stromal bed in the SMILE cases, and stromal bed displacements and stresses were more affected by a loading increase in eyes with flaps than in the flapless ones.4 SMILE also helps avoid—but doesn’t eliminate—one of the most dreaded complications associated with LASIK: ectasia.
Responding to Criticisms
Over the past year or so, some surgeons have leveled criticisms at the SMILE procedure. However, these issues aren’t as significant as they’re made out to be:
• SMILE is too difficult. Some surgeons say that working with the SMILE lenticule is much more technically difficult than performing the steps involved with LASIK. Though working with the lenticule is more involved than cutting and lifting a flap, LASIK still has a learning curve of its own. Also, after you’ve performed some SMILE procedures and gotten comfortable with it, you’ll appreciate benefits such as better corneal sensation, stronger corneal structure and excellent predictability, even at high levels of correction.
• Enhancements are a problem. Enhancements haven’t really been an issue for us due to the procedure’s high accuracy, at least in our hands. We haven’t had to do one in the past year.
If an enhancement is required though, it’s not an insurmountable obstacle. If we ever need to enhance a SMILE, our procedure of choice is a PRK procedure on top of the cap with adjunctive use of mitomycin-C. Zeiss has also developed a SMILE enhancement procedure known as CIRCLE, in which you convert the SMILE cap into a flap and then use the excimer laser to ablate the stromal tissue.
In a retrospective study of surface ablation enhancement after SMILE, surgeons performed PRK on 43 eyes out of 1,963 SMILE cases (2.2 percent). Spherical equivalent was -6.35 ±1.31 D before SMILE and -0.86 ± 0.43 D before the PRK. Surface ablation was performed after a mean of 9.82 ±5.27 months, and resulted in a spherical equivalent of 0.03 ±0.57 D at three months (p<0.0001). The number of patients within ±0.5 and ±1 D of their target refraction respectively increased from 23 percent to 80 percent and from 73 percent to 93 percent. In these 43 enhancement eyes, mean uncorrected distance acuity improved from 0.23 ±0.20 logMAR (a little worse than 20/32) to 0.08 ±0.15 logMAR (about 20/20) (p<0.0001). The average best-corrected acuity remained unchanged overall (p=0.99), with 65 percent of patients gaining at least a line. Six eyes (15 percent) lost a line of BCVA, but the final BCVA was 20/20 in four of these cases and 20/25 in the other two.5
Ultimately, for us, SMILE is the effective, safe procedure we’ve relied on for the vast majority of cases for several years and, at this point, it’s hard to argue with 3,000 happy patients. REVIEW
Dr. Hjortdal is a consultant and clinical professor of ophthalmology at Aarhus University Hospital in Denmark and medical director of the Danish Cornea Bank. Aarhus University Hospital has specified research support agreements with Carl Zeiss Meditec.
1. Walter KA, Stevenson AW. Effect of environmental factors on myopic LASIK enhancement rates. J Cataract Refract Surg 2004;30:4:798-803.
2. Summary of safety and effectiveness from the SMILE FDA trial. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040B.pdf. Accessed 5 January 2019.
3. Vestergaard AH, Grønbech KT, Grauslund J, Ivarsen AR, Hjortdal JØ. Subbasal nerve morphology, corneal sensation, and tear film evaluation after refractive femtosecond laser lenticule extraction. Graefes Arch Clin Exp Ophthalmol. 2013;251:11:2591-600.
4. Seven I, Vahdati A, Pedersen IB, et al. Contralateral eye comparison of SMILE and flap-based corneal refractive surgery: Computational analysis of biomechanical impact. J Refract Surg 2017;33:7:444-453.
5. Siedlecki J, Luft N, Kook D. Enhancement after myopic small incision lenticule extraction (SMILE) using surface ablation. J Refract Surg 2017;33:8:513-518.
Counterpoint—LASIK: The Clear Choice
Often, when a difficult problem is finally solved, it turns out that the solution isn’t only effective-—it’s elegant as well, unburdened by unnecessary complexity. For the problem of refractive errors, LASIK remains the most elegant solution, in addition to being very safe and effective. This is why SMILE’s overly complicated approach to treating refractive errors falls short in comparison. Here, I’ll explain why I choose LASIK for my refractive patients.
 |
SMILE’s Shortcomings
Before I delve into the reasons why SMILE isn’t as good as LASIK, I want to say that I’m a big fan of the Zeiss VisuMax laser, and it’s my favorite flap-making laser for LASIK procedures.
That said, I’m not a fan of SMILE. I’ve come to this opinion by monitoring the ophthalmic literature since the procedure was first released. Also, we have the VisuMax in our facility, and one of my partners has been performing SMILE for a couple of years, so I’ve observed the procedure’s results. Here are the issues with SMILE that I’ve noticed.
• It’s more difficult to do. The first, and one of the more important, things I’ve noticed through this observation is that LASIK is a much simpler procedure than SMILE. Because of SMILE’s complexity, you’re much more likely to end up with a problem during surgery. There were even some papers published about how to handle retained lenticules that were either not fully cut by the laser or were torn during the extraction process, trapping a lenticule fragment within the interface. This fragment then has to be removed or the patient will have severe irregular astigmatism. This increased difficulty is one of my major concerns as SMILE seeks acceptance among a wider audience of ophthalmologists.
• SMILE cuts introduce variability. Another one of the major differences between the two procedures is that, when you make a cut with the femtosecond, no two cuts are the same. I’ve used the IntraLase, the Alcon LenSx and the VisuMax, and they all have this issue; when you cut across the cornea to make the LASIK flap, they can skip a spot here or there in a random way or produce other small imperfections. So, when you lift the flap, you notice slight irregularity in the bed. LASIK, however, is very forgiving of this, because as long as you return the flap to its original position, those irregularities are masked and not reflected in the optical surface. Therefore, they don’t affect the patient’s vision.
When you make the two femtosecond cuts necessary to create the lenticule in SMILE, however, you now have two femtosecond-cut surfaces that no longer match up. Then, when you extract that piece of cornea and the two mismatched surfaces are pressed together, they don’t match. That’s what produces the irregularities that result in patients having a delayed visual recovery with SMILE compared to LASIK (LASIK patients see clearly almost immediately, compared to a several-day delay with SMILE reported in several studies).
• More manipulation, more irregularities. It’s not just the laser cuts that introduce vision-affecting irregularities, it’s the extra mechanical manipulation, as well: Once the lenticule is cut by the two laser passes, you still don’t have a free lenticule. Instead, you now have to use a second instrument in the interface, a spatula, both anterior and posterior to the lenticule, to physically break the remaining adhesions between the lenticule and surrounding cornea. By doing that, you induce even more irregularity.
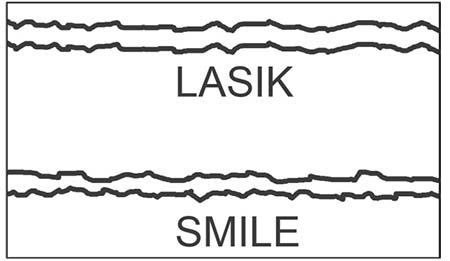 |
| The reason SMILE patients take longer than LASIK patients to recover vision, Dr. Wilson says, is because the interfaces in SMILE don’t line up when the lenticule is removed, resulting in irregularities. |
• The femtosecond is less precise than the excimer. Piggybacking on the previous points, Zeiss will probably say that it has a new spot distribution coming out that will help with the problem of the surface irregularities—and it might—but the irregularities will still be a problem, even with a new spot distribution. Why? Because the femtosecond just doesn’t have the inherent accuracy and precision of an excimer laser: The original IBM researchers who studied the early excimer lasers actually used one to carve the IBM logo onto a human hair—no femtosecond laser will ever match that precision. As a result, SMILE will always have a slower visual recovery, and much less of a “wow” factor, than LASIK.
• Enhancement questions. The flip side to the elegant solution referenced earlier is the problem with multiple solutions; this usually means none of them is ideal. This is the current situation with SMILE enhancements.
LASIK is very easy to enhance. If you perform the enhancement within the first postop year, you can lift the flap without much difficulty and apply additional excimer laser to fine-tune an under- or overcorrection, or treat a little induced astigmatism. With SMILE, though, no one has agreed on the best way to perform a retreatment if the primary procedure gets an undesirable result. You either have to do a surface ablation or try to convert the SMILE to a LASIK, and the company’s actually designed an algorithm to do that. At our facility, we found the SMILE enhancement rate to be higher than LASIK’s, because it’s just not as precise. There’s also the impression a patient gets if he needs an enhancement: Preop, the patient was no doubt told the purported advantages of SMILE over PRK and LASIK, only to find out that, six months later, he needs PRK or LASIK to correct his SMILE procedure that came up short. This isn’t an enjoyable conversation to have.
• SMILE takes more time to do. With all the tissue manipulation involved with SMILE, it ends up taking twice as long as LASIK. This is the last thing a busy surgeon wants to hear. Adding that extra surgery time is a very big deal for the refractive surgeon, because you only have so many surgery slots during a day. If you’re occupying two spots instead of one, you cut down on your productivity, and productivity is a big part of having a successful refractive practice.
• SMILE misses out on surgical advances. About 10 years ago, every other paper presented at the AAO and ASCRS was about the importance of wavefront-driven ablations in LASIK and their ability to reduce visual aberrations. More recently, companies like Alcon have introduced topography-driven ablations and highlighted some of the better results that can be achieved with that technology. Unfortunately, you can’t use either of these approaches with SMILE. So are we suddenly saying that all of that development wasn’t important? On the contrary: Eighty percent of my LASIK patients have wavefront-driven ablations done with the excimer laser.
 |
| Unmatched precision: The excimer laser was once used to carve the IBM company logo onto a human hair. The femtosecond is incapable of such feats, Dr. Wilson says. |
• There’s still ectasia with SMILE. One of the advantages touted for SMILE is biomechanical superiority compared to LASIK, with proponents specifically saying it leaves the anterior cornea basically untouched. This, they say, makes it less likely for patients who have abnormal corneal topography or thin corneas to develop ectasia after SMILE vs. LASIK for the same level of myopia correction. However, there are now several papers from surgeons who’ve used SMILE in place of LASIK for these questionable cases that subsequently developed ectasia.1 Though, theoretically, there may be some biomechanical advantage to SMILE, someone performing the procedure has to be very careful about assuming he’s going to have an advantage in treating those cases with inferior steepening or low corneal thickness, because it could be a trap. Surgeons now recommend using the same screening criteria for SMILE as LASIK when it comes to ectasia risk.
The other biomechanical argument is that there’s no risk of postop flap dislocation with SMILE. Theoretically, this is the case. However, I’ve only encountered one dislocated flap in the 23 years I’ve been doing LASIK. The large-scale data from the military supports this, as the service now allows soldiers and sailors to undergo LASIK due to the real incidence of late flap dislocations being so low.2,3 In theory, a flap could be truncated by a severe enough blow, such as a car’s airbag deploying, but typically that sort of force would be so powerful that it would risk damage to the cornea even if the patient had had SMILE, or no surgery at all.
• Dry-eye considerations. Though it may be true that there’s less dry eye with SMILE than LASIK, I think that given the thin flaps used with today’s LASIK procedure, we don’t have as much of a dry-eye problem as we did in the past. This is especially true if we pretreat patients prior to LASIK with medications like Restasis and other measures—which you’d want to do anyway with SMILE. In my practice, where I do a lot of LASIK and PRK, dry eye isn’t that much of an issue when appropriate precautions are taken.
So, considering all of the reasons listed above, as well as the great outcomes my patients enjoy after LASIK, I’m confident in choosing it over the newcomer, SMILE. REVIEW
Dr. Wilson is a professor of ophthalmology, director of corneal research, as well as the staff of the refractive surgery and cornea sections of the Cleveland Clinic’s Cole Eye Institute.
1. Moshirfar M, Albarracin JC, Desautels JD, Birdsong OC, Linn SH, Hoopes PC Sr. Ectasia following small-incision lenticule extraction (SMILE): A review of the literature. Clin Ophthalmol 2017;15;11:1683-1688.
2. Tanzer DJ, Brunstetter T, Zeber R. Laser in situ keratomileusis in United States naval aviators. J Cataract Refract Surg 2013 Jul;39:7:1047-58.
3. Warfighter Refractive Eye Surgery Program Overview. https://www.crdamc.amedd.army.mil/surgery/lasik.aspx. Accessed 10 January 2019.



