Sticking with Scleral-Sutured IOLs
Gregory S. H. Ogawa, MD, Albuquerque, New Mexico
 |
After 26 years of scleral fixating IOLs, I continue to achieve excellent results by using a scleral-sutured technique. Yes, I keep on top of the innovations that our colleagues introduce, including the use of haptic scleral fixation championed by proponents of the Yamane technique. However, I still don’t see a reason to change my approach, nor do the results of nearly 2,000 cases I have completed suggest that I should do so.
In this point-counterpoint, my point is that my tried-and-true method is still the best one to use when patients experience dislocation problems with their crystalline lenses or original IOLs.
Validating Data
To check the validity of my approach, I evaluated the results of 202 scleral-sutured 9-0 polypropylene posterior chamber IOL surgeries that I completed between 2004 and 2008, the data for which I presented at the 2017 AAO meeting. Indications for surgery included aphakia, dislocated/subluxated IOLs or natural lenses, corneal edema and uveitis/glaucoma/hyphema syndrome. The average time between surgery and data review was 10.8 years.
This series—standardized by the use of data from a single surgeon—showed overall improvement in visual acuity, minor complications (six intraoperative and five postop), sustained IOL fixation and refractive predictability. These results were all with 9-0 polypropylene (Prolene; Ethicon) before transitioning to polytetrafluoroethylene (PTFE) monofilament suture (Gore-Tex; W.L. Gore). The data revealed no cases of IOL tilt, suture erosion or unusual IOP elevation. Additionally, I can’t recall any of my suture-fixated IOL patients needing reoperations related to the IOL fixation, besides the few who had late polypropylene suture breakage. Nor have I seen erosions of sutures coming through my patients’ conjunctiva when the knot is buried inside the eye.
In contrast, professor Shin Yamane, MD, pioneer of the haptic-fixated technique named after him, has only been using his technique since 2014. A sober look at his technique, which, granted, has garnered much excitement, shows no 10-year data supporting its long-term efficacy.1 Also, keep in mind that Dr. Yamane uses an IOL from Santen Pharmaceuticals (Osaka, Japan) that has an optic with a 7-mm diameter, which is 1 mm greater than foldable options available in the United States.
Using Yamane’s smaller-diameter implants increases the potential for symptoms from decentration. The Santen IOL also has a greater overall diameter than IOLs in the United States and offers more haptic material to use, potentially useful in larger eyes. For these reasons, one could argue that using Dr. Yamane’s results to support the use of his technique in the United States may not be valid.
 |
| Watch the video here. |
Right Setting
Besides reliable long-term results, practice environment also plays a role in my decision to keep performing scleral-sutured fixation of secondary IOLs. Here in New Mexico, where the number of doctors per capita is low, we have a population of only 2 million people, including 1 million in metropolitan Albuquerque, where I see patients and perform surgery. If a patient has a problem with a lens or a need for a second surgery, that patient may have to drive up to six hours to get follow-up care. We also have a high concentration of Native Americans, who, by cultural norms, typically don’t return to see us unless they have more serious issues. Imagine that a postop patient has part of a haptic beginning to push through the conjunctiva after use of the Yamane technique. Although the emerging haptic may initially feel like a minor foreign body sensation, it eventually could open a tract for pathogens into the eye, resulting in a case of
endophthalmitis.
We know that we won’t have the opportunity to perform a second surgery or respond to complications easily in our setting. I’m also a surgeon to whom other surgeons send their patients for the last surgery those patients, hopefully, will need. This role compels me to respond accordingly. Currently, I wind up doing about 100 of these procedures each year, with no serious IOL-related complications.
Additional Risks
The longer you expect a patient to have a sclera-friction-supported IOL in place, the more likely the haptic will erode through the conjunctiva or loosen in the sclera. So I think sutured scleral fixation is especially important for younger patients, holding up for multiple decades of lens fixation. This is another reason to fixate with Gore-Tex, which should last a lifetime.
For patients in their 80s and 90s on anticoagulation—who would benefit from a smaller needle pass than is feasible with Gore-Tex—I often use Prolene sutures. Although Prolene degrades over time, the impact of suture degradation is less significant in this age group.
Good to Go
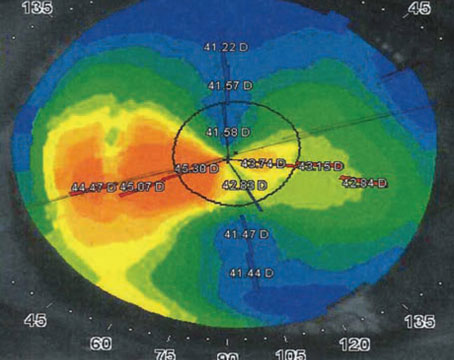
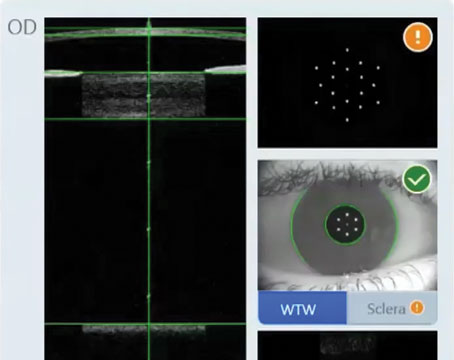
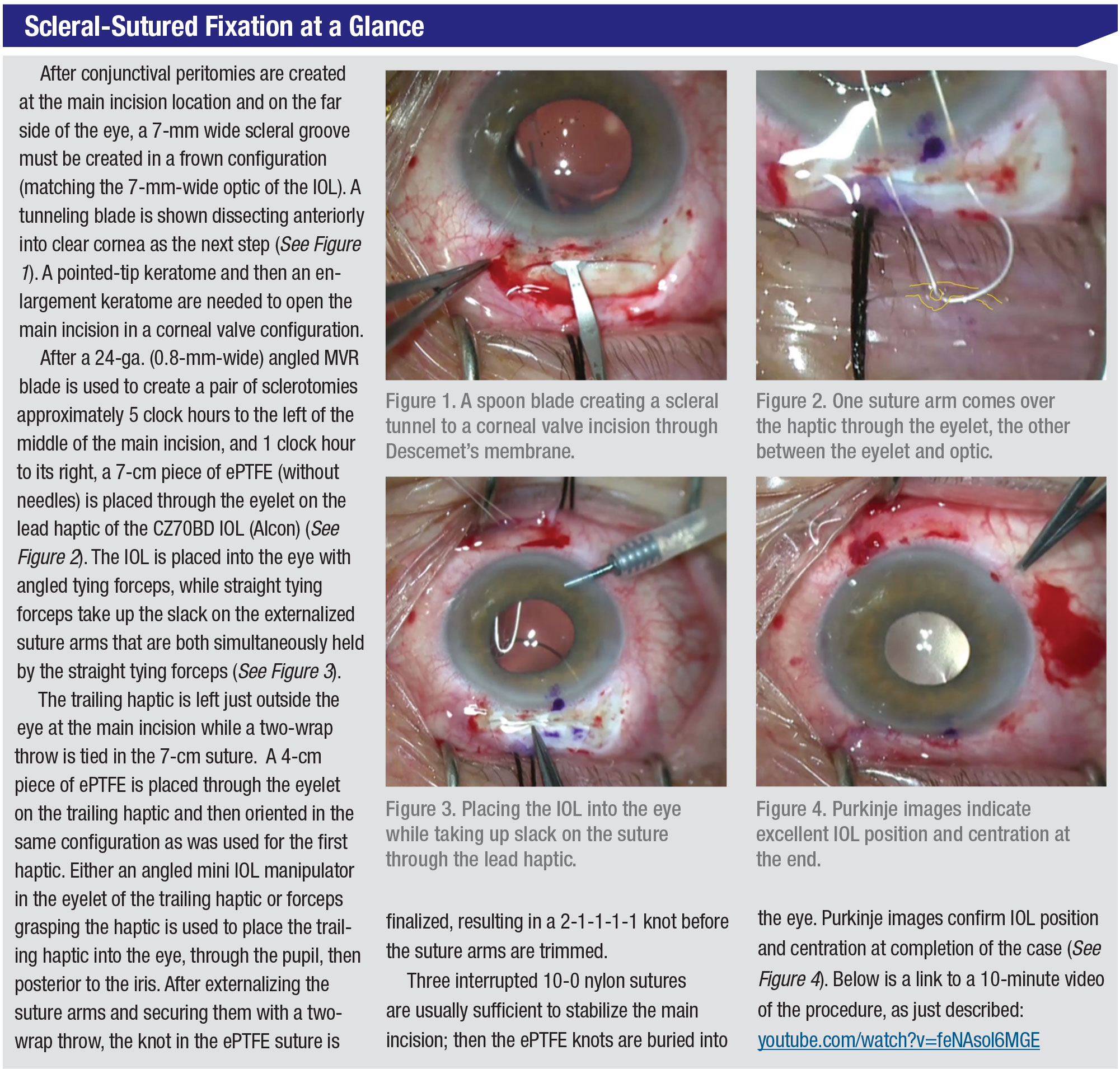
Like most of us, I typically do a lens exchange when a patient’s lens implant has gotten loose or dislocated and the patient doesn’t have a lens capsule to support the secondary IOL. I use a reproducible approach to set up the procedure, make the incision and place the new implant (Alcon CZ70BD) right where I want it to be. The lens is flat and centered. Then I finish tying my sutures and everything is good to go. (See “Scleral-Sutured Fixation at a Glance,” above.)
On the other hand, I recently heard a Yamane-technique expert say in a lecture that he needs to make an extra needle pass (after the initial two needle passes) in 30 to 40 percent of his cases because the patient’s lens is either tilted or not centered. He’s quite comfortable doing this. I like to just do my procedure and have it come out the way it’s supposed to come out on my first try. My rate of making just one additional incision to move a suture is roughly 1 percent.
In certain cases, such as when a patient with a dislocated IOL has a large glaucoma bleb affecting the cornea, or some other anatomic characteristic that prevents me from making an appropriately-sized scleral tunnel incision, I may elect to harness the original lens implant through small incisions instead of replacing it.
By passing the Gore-Tex inside the haptic and through the lens capsule (if there’s no significant Soemmering material), I can refixate this original implant, which can be an effective solution.
Never Say Never?
Would I ever use the Yamane technique? I could see myself performing the procedure for the patient who has an insufficient amount of scleral tissue for a tunnel, prompting me to go through a corneal incision. In such a case, I could take advantage of the Yamane’s 3-mm incision instead of the 7-mm incision required for CZ70BD fixation. That said, I haven’t encountered this situation yet and therefore I haven’t needed to switch to the Yamane technique. In the meantime, I’ll just keep doing what I’ve been doing. Why should I change now?
Dr. Ogawa is a partner at Eye Associates of New Mexico and an associate clinical professor of ophthalmology at the University of New Mexico School of Medicine. He has disclosed no relevant financial relationship.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmolol 2017;124:8:1136-1142.
Make Room for Yamane’s Efficiency
Brandon Ayres, MD, Philadelphia
 |
Colleagues ask me why I choose the Yamane technique for secondary IOLs in eyes that have minimal or no capsular support. The simple answer is that the haptics used to fixate the IOL are stronger than scleral sutures and that the Yamane technique’s 3-mm incision is much better for the patient than the 7-mm incision required to complete the scleral-sutured technique. But there’s more to it than that, as I’ve discovered while doing hundreds of these procedures. I’ll explain the advantages the Yamane technique can provide most of your patients, as well as challenges you need to overcome and contraindications to consider. My argument is this: Shouldn’t more surgeons at least start doing these procedures when appropriate?
Why Yamane?
For many years, surgeons in our practice performed scleral-sutured procedures, using Gore-Tex fixation and a variety of foldable IOLs. We’ve switched to haptic fixation, using the Yamane technique for most cases in part because of the problems we’ve experienced when working with nonabsorbable polytetrafluoroethylene (PTFE) monofilament suture (Gore-Tex; W.L. Gore), including opacification of the lens material and exposure of the Gore-Tex knot. (Remember that Gore-Tex is not approved for use in the eye.) The Yamane technique meets the same objective as scleral-sutured fixation, and it can be used by all surgeons.
You can also use the Yamane technique with almost any three-piece IOL you have in the OR or on standby. Most three-piece IOLs are made of either silicone or hydrophobic acrylic material. It may be wise to stick with the hydrophobic acrylic three-piece IOLs, because using this material is always safe. Even if the patient needs vitreoretinal or corneal surgery, the material will stand the test of time. Silicone three-piece IOLs can be problematic if patients need silicone oil placed for retinal detachment repair. Hydrophilic acrylic IOLs with hydroxyapatite may opacify when exposed to the surgical air or gas used in retinal surgery, as well as lamellar keratoplasty (DSEK and DMEK).
Degradable Sutures
Lack of scleral suture stability has also been a concern for us. Polypropylene (Prolene), the suture material that functions as a frequent alternative to Gore-Tex, can degrade or break, leading to dislocation of secondary IOLs. I’ve already needed to refixate several secondary IOLs that I had sutured into patients’ scleras with polypropylene. A primary concern with Gore-Tex, meanwhile, is that using this stronger material for scleral fixation is significantly more challenging than what we experience when we use the haptic fixation of the Yamane technique. Fixating with Gore-Tex also creates the need for more scleral incisions.
Meanwhile, we’ve found that the haptics of secondary IOLs keep implants in place longer than sutures. With the Yamane technique, you can take advantage of the enduring longevity of fixation. Your patient benefits significantly from the Yamane’s approximate 3-mm incision, which won’t require a single suture. Also, we’re making needle sclerotomies, not large ones, meaning patients on anticoagulants are less likely to experience vitreous hemorrhage. And we can get by with less anesthesia.
Efficiency is probably the biggest advantage, however. Even a very efficient surgeon may require 20 to 25 minutes to suture in an IOL. With haptic fixation, you can be in and out of the eye in 10 minutes, reducing your patient’s exposure to potential infections and time in the OR.
Special Equipment
The Yamane technique does require special equipment. Make sure you have microforceps, low-temperature cautery and the correct needles and/or trocars. A thin-walled 30-ga. needle, or at least a 27-ga. needle, is essential. Your equipment supplier may be able to provide haptic-fixation kits that include an anterior segment pressure maintainer, low temperature cautery, a marking pen and a caliper. With such a kit, your scrub nurse doesn’t have to go picking out these items one at a time.
I will say this: If you’re new to the Yamane technique, you’ll face initial challenges. If a haptic gets kinked when you’re trying to manipulate an implant in the eye, for example, that haptic will be rendered useless. When trying your first few cases, which can be difficult, use a three-piece IOL that has polyvinylidenefluoride (PVDF) haptics.
PVDF haptics don’t kink easily and are much more resilient than other haptics. In the United States, the only available three-piece PVDF IOL is the Zeiss CT Lucia 602. Use it until you’ve developed the necessary dexterity to thread the haptics and manage the procedure. All other three-piece IOLs have PMMA haptics, which you can eventually adapt for this technique.
The benefits of taking this approach? When I compare scleral-sutured fixation patients to haptic-fixated patients, I always find that the haptic-fixated patients are more comfortable after surgery. They also generally seem to recover faster and their implants achieve stability more quickly. We typically produce good results, which satisfies patients,
because we’re using better and more familiar materials. Although applying the haptics of an IOL for scleral fixation is admittedly an off-label use, we’re not using an off-label suture, such as Gore-Tex. So it’s one less off-label issue we need to discuss with the patient as a potential drawback.
Adapting the Technique
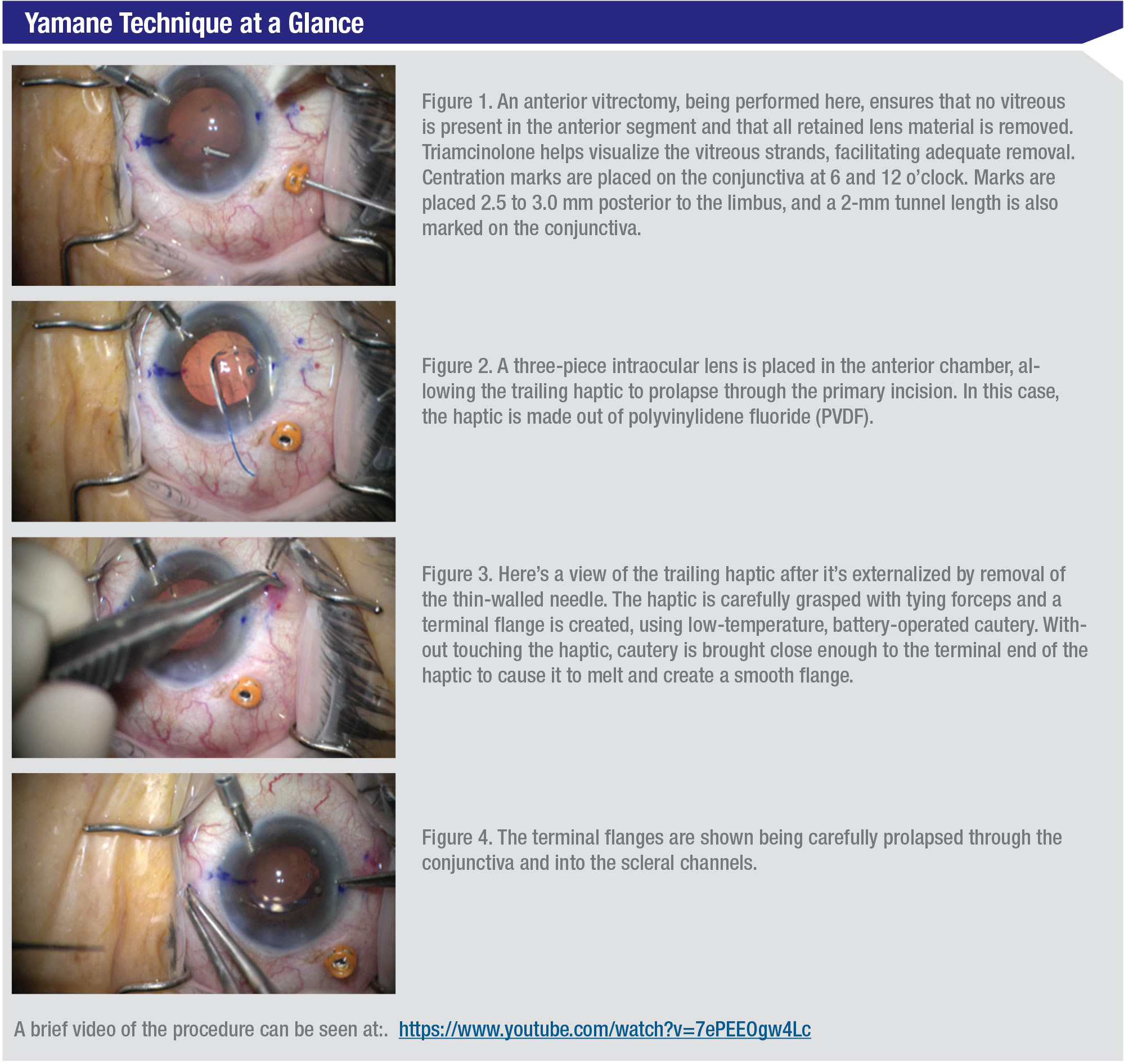
The three most important steps when adapting the Yamane technique are practice, practice and practice—in the wet lab before performing on patients. Make sure you can set up the incisions and make proper measurements. Otherwise, you could end up with a decentered implant. (See “Yamane Technique at a Glance” below.)
Your comfort is an important factor. Many of us are used to scleral-suture-fixating IOLs. With the Yamane approach, understand that getting the haptic-fixated IOL spot on with your first try can be a challenge. I’ve watched beginning surgeons struggle for more than an hour to complete the procedure. So although I assure you that the surgery can be done in 10 minutes, I need to point out this is possible only after doing many cases.
 |
| Watch the video here. |
When Yamane’s Not Ideal
As effective as haptic-fixated surgery may be, I find that I’m able to use it in only 70 percent of my cases of complicated IOLs. Because I know my own nomogram, I can scleral fixate in the remaining cases with sutures. I know I’m accurate when suturing with four-point Gore-Tex in an off-label fashion like this.
I really think that centration and tilt are actually very predictable and better when we use scleral-sutured fixation, which can be one advantage of this technique that sets it apart. I put the IOL in, suture it, then tie my sutures. I usually like the way the implant looks. I don’t have to go back and move a suture or revise it.
Because of these factors, I’m mindful that scleral-sutured fixation might meet the expectations of premium IOL patients better than haptic fixation in some cases. When fixating a premium IOL, I want to at least minimize any need for postop distance glasses. I can help the patient more from a refractive-target standpoint if I use scleral-sutured fixation. This is generally borne out in our patient data, although the data vary among surgeons and procedures.
I’ll also turn to scleral-sutured fixation if I’m managing a complication from another surgeon, and I need to be as precise as possible with my IOL calculation. We’ll consider scleral-sutured fixation as long as the patient has no retinal pathology, which we can confirm because the patient undergoes a vitrectomy before fixation. Other essential prerequisites for scleral-sutured fixation include good corneal cell counts and otherwise healthy corneas.
There are a handful of other situations in which Yamane might not be the preferred approach:
• Disorganized anterior segment. The haptic-fixation technique would be more difficult to perform in the presence of extensive iris damage or aniridia. During the Yamane technique, you’ll tend to rest the three-piece IOL first on the anterior chamber and iris while making your sclerotomies. Having no iris, or no substantial iris, would complicate the procedure. Scleral fixation may have an advantage here.
• Artificial iris procedure. Not many surgeons do this, but if you’re one of them, don’t involve the Yamane technique, for the reasons mentioned above.
• Lack of conjunctival space. You need some real estate on the conjunctiva to succeed with the Yamane technique. The best ergonomic approach is to sit in a temporal position at 6 and 12 o’clock to make the needle sclerotomies, thread the haptics and place the haptics in the anterior segment. Sitting in a superior position and making your sclerotomies at 3 and 9 o’clock also works well. However, if your patient has a trabeculectomy, tube shunt or tube, these areas will already be occupied by other hardware, making it very difficult to shift your incisions to where you need them to fit. Suture fixation may be a better approach.
Achilles Heel
Lens tilt and decentration admittedly are the Achilles heel of the Yamane technique, affecting about 30 percent of my Yamane cases (besides the approximate 30 percent of overall secondary IOL cases for which I elect to perform scleral-sutured fixation from the outset). If I find a lens is too nasal, or imperfect in any other way after fixating it with haptics, I cut the responsible haptic and fixate it again. I don’t see the routine need to revise a surgery as a failure because I can fix the lens during the same procedure, without creating infection and without the patient realizing it. To succeed, you need to be comfortable revising the surgery before finishing it. I should also emphasize that the differences between the outcomes of scleral-fixated versus haptic-fixated secondary IOLs are quite small.
Obvious Benefits
Surgeons are paying a lot of attention to the haptic fixation of the Yamane technique—and rightfully so. It’s been great for our practice, and I’ve come to enjoy the technique because of the benefits it helps me achieve for my patients and my surgery. I just don’t want to oversimplify it and give the impression that the technique is easy and that you can do it with little training and practice.
Any scleral IOL fixation technique for a secondary IOL can be risky if it’s not tackled with the right levels of knowledge, experience and preparation. However, any surgeon who has a sufficient degree of commitment and dedication to mastering a procedure can succeed with the Yamane technique, which I’m advocating for here. REVIEW
Dr. Ayres is part of the Cornea Service at Wills Eye Hospital and Ophthalmic Partners of Pennsylvania. He’s also Co-Director of the Cornea Fellowship at Wills and an instructor at Jefferson Medical College, Thomas Jefferson University in Philadelphia. He is a Consultant for Alcon, Carl Zeiss Meditech and Microsurgical Technology.