Many people likely remember being kept home by parents or sent home by teachers upon developing "pink eye." Conjunctivitis comes in several varieties, and can be caused by many different pathogens, as well as have several degrees of severity. In this article, we'll provide insights on diagnosing the various types of conjunctivitis, with a focus on viral disease.
Symptoms, Diagnosis, and Treatment
Viral conjunctivitis is frequently associated with upper respiratory infections. Adenoviruses are the most common offenders, while herpes viruses are the most problematic. Treatment can be in the form of anti-viral medications, although most cases are self-limiting and resolve within two weeks.1 Staphylococcus and streptococcus are common instigators of bacterial conjunctivitis. With or without antibiotics, the eye usually resumes its natural whiteness in a week.2 The third type of conjunctivitis is allergic, and persistent itching in the presence of pollen, animal dander, dust, etc. distinguishes it from other forms of conjunctivitis. There is no cure for this over-reactive immune response, although topical antihistamine/mast-cell stabilizers can ease symptoms.3
With the exception of the allergic variety, conjunctivitis is highly contagious. Furthermore, viral conjunctivitis can be an indicator of a more serious condition, and if left untreated may lead to loss of vision.4 Unfortunately, the signs and symptoms of all three forms of conjunctivitis often overlap.
Differential diagnosis of conjunctivitis largely relies on clinical signs and symptoms. Medical and personal histories are also important. Allergic conjunctivitis is characterized by itching, chemosis, redness, tearing and eyelid swelling in both eyes. Corneal scrapings and skin prick tests can help to confirm the diagnosis. The patient's personal and clinical history is generally enough to differentiate the allergic type from bacterial or viral conjunctivitis; however, the differentiation between the latter two can be tricky.
Both bacterial and viral conjunctivitis usually begin in one eye and may progress to the other. Redness, tearing and irritation are also characteristic of the two. Luckily, bacterial is often distinguished by conjunctival swelling and a sticky discharge—if patients come in complaining that their lids were stuck together upon waking, then it's almost certainly bacterial. Microedema around the capillary networks that produces a vague hillock and papillary reactions are also seen in bacterial conjunctivitis. Viral conjunctivitis is often characterized by swollen pretragal nodes, particularly if the patient has never had viral conjunctivitis before. It's important to palpate these nodes when a patient presents with conjunctivitis. Still, the symptoms of viral and bacterial conjunctivitis overlap, and not all symptoms are always present.5 A diagnosis based on history and symptoms in an otherwise healthy individual can be challenging.
Unfortunately, the immediate reaction of many doctors when a patient presents with pink eye is to prescribe antibiotics—a route that not only increases bacterial resistance to the drugs, but will not be effective if the infection is viral. Antibiotics also offer questionable effectiveness at speeding recovery from bacterial infections; one study found no significant difference in children's recovery time or adverse events between treatment and placebo groups.6 Furthermore, a systematic literature search of the signs and symptoms of conjunctivitis when compared to culture results suggested an absence of consistent, definitive diagnoses.7 Considering that the condition is self-limiting and symptoms persist for less than a week, antibiotics don't seem necessary. However, there are exceptions: trachoma (chlamydial conjunctivitis) is contagious and is spread through contact with mucosal secretions. It's a form of chronic follicular conjunctivitis, and symptomatic conjunctival scarring and trichiasis often result in corneal ulceration and opacities. The World Health Organization estimates that trachoma causes some 6 million cases of blindness yearly, although the disease has been eliminated in the
Viral Causes
Viral conjunctivitis, as opposed to bacterial, has a longer duration, rendering the hyperemia, chemosis and tearing less bearable to the patient. In addition, viral conjunctivitis has a tendency toward more serious symptoms, making antiviral treatment desirable. DNA viruses from the family adenoviridae are the most common cause of viral conjunctivitis.
The corneal involvement in adenoviral keratoconjunctivitis is unique within the realm of viral conjunctivitis. Corneal subepithelial opacities often develop about 10 days after symptom onset, and they can impair vision for months to years.9 Adenoviral keratoconjunctivitis currently has no specifically indicated antiviral medication; though cidofovir seems to be effective, it causes severe local toxicity in the high doses required to control the infection.10 Pharyngoconjunctival fever (PCF) is also associated with various adenoviruses; fever, pharyngitis and acute follicular conjunctivitis are its main symptoms. It generally clears within a few weeks. Nonspecific follicular conjunctivitis, also caused by an adenovirus, causes even less severe symptoms, although it may leave the eye open to more serious infections.1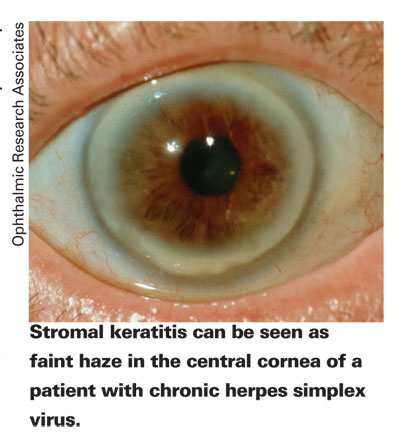
Herpes virus, particularly HSV1, is the most problematic cause of viral conjunctivitis. HSV2, the primary cause of genital herpes, is seldom seen in the eye. Although the initial infection of herpes simplex keratitis is often mild, the ocular symptoms, like the systemic disease, are recurrent, involving latent periods and outbreaks throughout the patient's lifetime. Such symptoms develop in less than 1 percent of general herpes cases.11
Corneal scarring, thinning and neovascularization result from uncontrolled recurrent HSK, eventually resulting in vision loss. The patient will also experience decreased corneal sensation. The virus lies dormant in the trigeminal ganglion, and head trauma may be a reason for the recurrence of symptoms (along with stress, fever, UV light, menstrual cycles and use of immunosuppressants). Topical acyclovir, valacyclovir and famcyclovir are effective at controlling symptoms, especially when combined with a steroid. Oral acyclovir is very effective at preventing recurrences of HSK. Unfortunately, corneal transplant doesn't prevent recurrence of the disease without the concurrent use of topical and systemic antivirals.4 Like the general systemic herpes infection, it's manageable but incurable.
The mode of transmission of viral conjunctivitis is largely dependent on the type of virus. Transmission of adenovirus is easy: Anything that has been in contact with the eye can transmit the virus, and since the virus is generally associated with an upper respiratory infection, it becomes airborne with sneezing and coughing. The entry point is therefore not only the eyes, but also the nose and mouth.12,13 Ocular herpes is commonly transmitted from other parts of a herpes-infected body, particularly lips with open sores, and from contacts after wetting them with saliva.4 Viral conjunctivitis can also be transmitted in pools with inadequate chlorine.1
Though it's rare in immunocompetent individuals, vaccines can result in ocular complications that can include conjunctivitis. For example, smallpox vaccinations, though currently uncommon due to the disease's eradication, result in ocular vaccinia in about one per 40,000 vaccinations.14 Aside from occurring in those with compromised immune systems, blepharitis, conjunctivitis and keratitis can occur from rubbing the vaccination site and then rubbing the eye. Symptoms often resemble ocular herpes, but a thorough patient history and laboratory testing can pinpoint the cause. Treatment consists of topical vidarabine or trifluridine, which limit the duration and severity of the outbreak.
Acute hemorrhagic conjunctivitis is another highly contagious ocular disease whose primary symptom is pink eye. Outbreaks have been reported worldwide.15-19 It's also characterized by rapid onset of ocular pain, tearing, foreign body sensation and photophobia. AHC is primarily caused by the RNA virus coxsackie A24, but enterovirus 70 can cause not only the conjunctivitis but also radiculomyelitis, which involves variable leg weakness, loss of bladder control and saddle anesthesia. The coxsackie-caused version is normally benign and clears up in seven days. The enterovirus version is rare, and the polio-like symptoms only manifest in one in every 10,000 patients. No cure is available for either form of AHC,20 although symptoms usually disappear in two weeks.16
There may be a redeeming quality to all these as-yet untreatable forms of viral conjunctivitis. The hygiene hypothesis, often used to explain the rising prevalence of allergies, holds that today's children grow up in environments that are so hygienic that their immune systems never mature. The balance of the infantile immune system is believed to be towards the Th2-specific response. However, exposure to pathogens and allergens early in life turns on the Th1 non-specific response, thereby building immunity to pathogens and to harmless allergens.
A literature search for viral conjunctivitis turned up a clinical case involving a 9-year-old boy with severe vernal keratoconjunctivitis. Two years after he was diagnosed with VKC, he presented with viral keratoconjunctivitis with subepithelial corneal infiltrates. After six weeks with symptomatic treatment, he experienced a complete recovery. The fascinating aspect is that, in the five year follow-up period after the viral infection, he had no symptoms of VKC. The giant papillae and a mild subepithelial fibrosis that had characterized his VKC diminished.21 This is by no means meant to encourage parents to expose their children to pink-eye to cure their allergies, but it does give support to letting self-limiting and harmless infections run their course. When the clinician suspects more serious forms of viral conjunctivitis, determining the specific pathogen (through immunoassays, polymerase chain reaction and tissue culture) is recommended.
Other Viral Involvement
Many viral manifestations besides conjunctivitis exist. Any sort of an infection, be it viral, bacterial or fungal, can be serious in immunocompromised individuals (such as HIV/AIDS patients), as well as in the very young and the very old. The most serious symptoms of viral diseases of the eye are generally seen in such individuals.
Children and young adults who were once infected with measles rarely have any lingering complications, but one in 100,000 patients develop subacute sclerosing panencephalitis. It is a neurodegenerative disease that leads to death in 95 percent of cases within three years. Remission occurs in the remaining 5 percent. Although the initially noticed symptoms are usually behavioral changes (e.g. irritability, loss of learning ability), ocular malfunctions occur in about half of the cases and precede neurological symptoms by a few weeks or months.22,23 Some suspect that early detection and treatment, before the onset of neurological symptoms, can prevent the full manifestation of the disease. Unfortunately, the initial symptoms of subacute sclerosing panencephalitis vary and can easily be mistaken for a genetic neurological disorder. High levels of measles IgG in cerebral spinal fluid in the presence of macular retinitis, papilledema, chorioretinitis, optic nerve pallor or several other visual disorders is cause for alarm. Isoprinosine and intramuscular beta-interferon therapy has been suggested as a treatment.24 In addition, the measles infection itself can occasionally show ocular symptoms when Koplik's spots appear on the conjunctiva.
Cytomegalovirus and varicella zoster virus are additional herpes viruses that can be problematic. CMV has a knack for resulting in corneal endotheliitis, uveitis25 and retinitis.26 Varicella zoster can quickly cause acute retinal necrosis.27 Again, these conditions are unusual in immunocompetent individuals, but occur more frequently in those afflicted with HIV/AIDS or who have otherwise suppressed immune systems.25,26
Many other viral diseases, especially those with a neurological route of attack (including 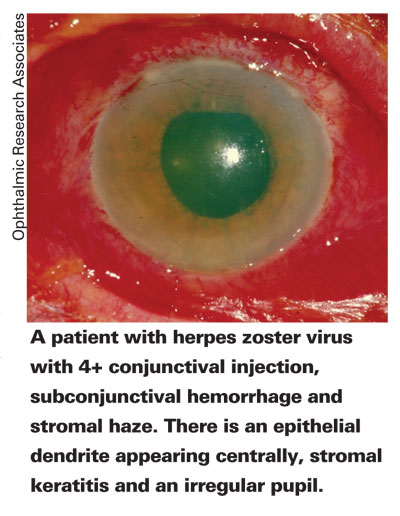
Ocular aberrations can be caused by many different agents that seldom lend the condition to easy diagnosis. Some of the viruses that cause ocular disease are highly contagious yet relatively harmless, while others are non- or minimally contagious but may be indicative of a more serious illness. However, the severity of the condition must be weighed against the benefits of medicating. The issues concerned with overuse of antibiotics are well known, and there is mounting evidence that suggests that overuse of antivirals may encourage viral mutation, resulting in resistance to the medications.30 Accurate and rapid differential diagnosis and the use of appropriate treatments for ocular diseases is vital.
Dr. Abelson, an associate clinical professor of ophthalmology at
1. Pavan-Langston D. Viral Disease of the Cornea and External Eye. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology 2nd Edition, Volume 2.
2. Foulks GN, Gordon JS, and Kowalski RP. Bacterial Infections of the Conjunctiva and Cornea. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology 2nd Edition, Volume 2.
3. Abelson MB, Smith L, Chapin M. Ocular allergic disease: Mechanisms, disease sub-types, treatment. Ocular Surface 2003;1:3:127-149.
4. Kaye S, Choudhary A. Herpes simplex keratitis. Progress in Retinal and Eye Research 2006;25:355.
5. Matoba AY. Harris DJ, Meisler DM, et al. Preferred Practice Patterns. Conjunctivitis. Available at: http://www.aao.org/education/library/ppp/conjunctivitis_new.cfm
6. Rose PW, Harnden A, Brueggemann AB et al. Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: A randomised double-blind placebo-controlled trial. Lancet 2005;366:37-43.
7. Rietveld RP, van Weert HCPM, ter Riet G, Bindels PJE. Diagnostic impact of signs and symptoms in acute infectious conjunctivitis: Systematic literature search. BMJ 2003;327:789.
8. Center for Disease Control, Division of Bacterial and Mycotic Diseases. Trachoma. [Web page].
9. Murrah WF. Epidemic keratoconjunctivitis. Ann Ophthalmol 1988;20:1:36-8.
10. Hillenkamp J, Reinhard T, Ross RS, et al. The effects of cidofovir 1% with and without cyclosporin A 1% as a topical treatment of acute adenoviral keratoconjunctivitis. Ophthalmology 2002;109:5:845-850.
11. Binder PS. Herpes simplex keratitis. Surv Ophthalmol 1977;21:313-331.
12. Bitko V, Musiyenko A, Barik S. Viral infection of the lungs through the eye. Journal of Virology 2007;18:2:783-790.
13. Gala CL, Hall CB, Schnabel KC, et al. The use of eye-nose goggles to control nasocomial respiratory syncytial virus infection. JAMA 1986; 256:19:2706-8.
14. Pepose JS, Margolis TP, LaRussa P, Pavan-Langston D. Ocular complications of smallpox vaccination. American Journal of Ophthalmology 2003;136:2:343.
15. Brandful JA, Yoshii T, Addy ET, Adiku TK, Osei-Kwasi M, Mingle JA. Epidemic acute haemorrhagic conjunctivitis due to Coxsackie virus A24 variant in
16. Tavares FN, Costa EV, Oliveira SS, Nicolai CCA, Baran M, da Silva EE. Acute hemorrhagic conjunctivitis and coxsackievirus A24v,
17. Moura FE, Ribeiro DC, Gurgel N, et al. Acute haemorrhagic conjunctivitis outbreak in the city of Fortaleza, northeast Brazil. Br J Ophthalmol 2006;90:9:1091-3.
18. Karki DB, Shrestha CD, Shrestha S. Acute haemorrhagic conjunctivitis: an epidemic in August/September 2003.
19. Chowell G, Shim E, Brauer F, Diaz-Duenas P, Hyman JM, Castillo-Chavez C. Modelling the transmission dynamics of acute haemorrhagic conjunctivitis: Application to the 2003 outbreak in Mexico. Stat Med. 2006;25:11:1840-57.
20. Wright PW, Strauss GH, Langford MP. Acute hemorrhagic conjunctivitis. Am Fam Physician 1992;45:1:173-8.
21. Sgrulletta R, Bonini S, Lambiase A, Bonini S. Allergy and infections: Long-term improvement of vernal keratoconjunctivitis following viral conjunctivitis. Eur J Ophthalmol 2006;16:3:470-3.
22. Dyken P. Subacute sclerosing panencephalitis. Neurol Clin 1985;3:1:179-196.
23. Santoshkumar B, Radhakrishnan K. Substantial spontaneous long-term remission in subacute sclerosing panencephalitis (SSPE). J Neurol Sci 1998;154:83-88.
24. Serdaroglu A, Gücüyener K, Durson I, Aydin A, Okuyaz Ç. Macular retinitis as a first sign of subacute sclerosing panencephalitis: The importance of early diagnosis. Ocular Immunology and Infiltration 2005;13:405-410.
25. Chee SP, Bascal K, Jap A, Se-Thoe SY, Cheng CL, Tan BH. Corneal endotheliitis associated with evidence of cytomegalovirus infection.
26. Kempen JH, Martin BK, Wu AW, Barron B, Thorne JE, Jabs DA. The effect of cytomegalovirus retinitis on the quality of life of patients with antiretroviral therapy.
27. Yoshida M, Hayasaka S, Yamada T, Yanagisawa S, Hayasaka Y, Nakamura N, Mihara M. Ocular findings in Japanese patients with varicella-zoster virus infection. Ophthalmologica 2005;219:5:272-5.
27. Cinatl J, Michaelis M, Fleckenstein C, et al. West Nile virus infection induces interferon signalling in human retinal pigment epithelial cells. Investigative Ophthalmology & Visual Science 2006;47:2:645.
28. Koevary SB. Ocular involvement in patients infected by the
29. Camelo S, Castellanos J, Lafage M, and Lafon M. Rabies virus ocular disease: T-cell-dependent protection is under the control of signaling by the p55 tumor necrosis factor alpha receptor, p55TNFR. Journal of Virology 2001;75:7:3427-3434.
30. Regoes RR, Bonhoeffer. Emergence of drug-resistant influenza virus: Population dynamical considerations. Science 2006;312:5772:389-91.