Cornea continues to be among the most active areas of research among ARVO scientists and clinicians. Here are some of the results of their recent efforts. Unless otherwise specified, these studies had no commercial support.
Endothelial Keratoplasty
A combined Swiss/Australian team of researchers reports that a handheld optical coherence tomographer can be used during Descemet's stripping automated endothelial keratoplasty (DSAEK) to assess the donor-host interface. The prospective, observational case series included six consecutively scheduled patients undergoing DSAEK. Intraoperative OCT scans of the central 4 mm of the cornea were performed after: insertion of the donor disc; instillation of air in the anterior chamber beneath the disc; vent incisions in the host cornea in each quadrant; air-fluid exchange at the end of the operation; and on the first postoperative day.
Images of the interface between the host and donor were obtained in all patients at each imaging session. No complications resulted from the intraoperative or postoperative use of the handheld OCT. In two patients there was a decrease in the width of the interface fluid after each surgical step documented by OCT scans. At the end of their operation, no fluid was left. In two further patients, fluid disappeared after the stab incisions and did not reappear during the further course of the surgery. In the last two patients, the detectable separation between the host and donor remained unchanged throughout the surgery. All patients had no detectable fluid within the interface one day after surgery. No graft dislocations occurred.766
Surgeons at the
Their retrospective chart review included 60 patients who underwent suture pull-through DSAEK (38 for Fuchs' dystrophy, six for pseudophakic bullous keratopathy, seven for edema, six for failed graft, and three for posterior polymorphous dystrophy).
Forty-one had no diagnosis of glaucoma, 10 developed elevated IOP and nine had glaucoma. Two normal and one glaucoma patients developed primary failure. The average initial and final acuity was 20/100 and 20/30 for normals, 20/70 and 20/60 for elevated IOP, and 20/400 and 20/60 for glaucoma.
All patients with glaucoma maintained IOP with their previous medicines. The majority of the patients with IOP elevations had their prednisolone switched to Lotemax. Three were treated with a prostaglandin analogue and two with beta-blocker. Three of 10 lost acuity.
None of the glaucoma patients lost acuity, while two of 43 normal patients experienced acuity loss. The average percentage endothelial cell loss was 52.4 percent for normals, 51.8 percent for elevated IOP and 53 percent for glaucoma. The three patients with elevated IOP and vision loss had IOP elevations greater than 10 mmHg within six months and endothelial losses of 62.1, 68.9 and 47.8 percent. The average IOP reduction was 22.9 percent with a prostaglandin analogue and 65.3 percent with a beta blocker. This is a small retrospective study and requires further study.757
Investigators from
Twenty-one eyes of 21 patients with endothelial dysfunction due to Fuchs' dystrophy and pseudophakic bullous keratopathy received transplants. All donor tissues were "de-swelled" by immersion in Thin-C media, a solution designed to reduce corneal thickness.
Anterior segment OCT was done using a custom-made adaptor, and confocal microscopy analysis was performed to record donor corneal thicknesses, endothelial cellular density and morphology.
After four hours, before the microkeratome cut, Thin-C reduced the donor corneal thickness an average of 100 µm. After microkeratome cut, on 20 donor tissues, the residual thickness of 10 donor corneas was between 115 and 195 µm and in the other 10 corneas, between 200 and 220 µm. After seven days the thickness decrease was 13 percent on average and after six months, 30 percent. Endothelial cell density decreased on average by 43 percent after six months. Postoperatively, there was one graft failure (4.8 percent) at one month due to intraoperative complications.742
Collagen Cross-Linking
In their prospective, randomized, controlled clinical trial, corneal collagen cross-linking was performed on 59 eyes, 40 with keratoconus and 19 with ectasia. The treatment group received UVA/riboflavin therapy, and the control group received riboflavin therapy alone. Objective corneal densitometry (haze) was measured over a central 4-mm segment of the cornea using Scheimpflug images at baseline, one, three, six and 12 months, and was correlated with clinical outcomes of visual acuity (UCVA and BCVA), manifest refraction, manual and Pentacam topography, and pachymetry. The Pentacam quantifies the haze of the cornea on a scale from 0 to 100.
Preoperative haze was 15.1 ±2.51. Haze peaked at one month (23.6 ±4.97, p<0.001). No significant change was seen at three months (22.3 ±5.16, p<0.001). Haze significantly decreased between three and six months (19.5 ±4.91, p<0.001), and continued to resolve through 12 months (17.1 ±4.41, p<0.001). At 12 months, however, haze had not completely returned to baseline. Analysis of the keratoconus and ectasia subgroups followed a similar course. However, the ectasia group did return to baseline at 12 months (15.8 ±2.30, p=0.27). No significant changes in haze were observed in the control group. Increased haze did not correlate with postoperative clinical outcomes (VA, refraction, corneal curvature changes and corneal thickness).4973
Same-day simultaneous topography-guided PRK and corneal cross-linking appears to be superior to sequential procedures of corneal cross-linking preceding PRK in the visual rehabilitation of progressing keratoconus, according to a large study in
The retrospective study included 325 keratoconic eyes. In Group A, 127 eyes had topography-guided PRK at least six months following cross-linking; in Group B, 198 eyes had PRK first with cross-linking immediately afterward (simultaneous procedure). Mean follow-up was 36 ±18 months (r: 24 to 68). The groups were examined for changes in UCVA and BCVA in logMAR values, mean radial spherical error, refraction, keratometry, topography, central corneal thickness, endothelial cell count, corneal haze grades and ectatic progression.
In Group A, the mean UCVA improved from logMAR 0.9 ±0.3 to 0.49 ±0.25 and BCVA improved from 0.41 ±0.25 to 0.16 ±0.22. Mean spherical equivalent reduction (SER) was 2.5 D ±1.2 D. Mean haze score was 1.2 ±0.5 and mean keratometry reduction was 2.75 D ±1.3 D.
In Group B, mean UCVA improved from 0.96 ±0.2 to 0.3 ±0.2, and mean BCVA improved from 0.39 ±0.3 to 0.11 ±0.16. Mean SER was 3.2 D ±1.4 D and mean haze score was 0.5 ±0.3. Mean keratometry reduction was 3.5 D ±1.3. Cell count was unchanged (p<0.05) in both groups. Group B had greater improvement in mean UCVA and BCVA, as well as a greater reduction in mean SER and mean keratometry. Mean corneal haze grade was also lower in Group B. All comparisons were statistically significant (p<0.05 for all comparisons).4967
Since collagen cross-linking results in increased collagen autofluorescence, investigators at the
They studied rabbit eyes separated into four groups (three eyes each) including control 1 (intact epithelium), control 2 (epithelium removed), riboflavin control, and riboflavin with UVA treatment for 15 and 30 minutes. Riboflavin-5-phosphate solution (0.1%) was applied every two minutes for 30 minutes prior to and during UVA irradiation. Corneal stiffness after cross-linking was measured by indentation after corneal removal. Corneas were fixed in 2% paraformaldehyde, washed and sectioned at 300 µm thickness using a vibratome. Tissue sections were then scanned using a confocal laser scanning microscope and femtosecond laser to generate two photon-excited CAF signals; and the image was collected and fluorescence intensity was analyzed.
The indenting force at 500 µm depth was 0.97 mN (SD 0.15) for control 1, 0.77 mN (SD 0.15) for control 2, and 1.17 mN (SD 0.23) for riboflavin-alone treated corneas, and no CAF was detected. Indenting force increased to 2 mN (SD 0.26) and 2.5 mN (SD 0.62) and CAF was detected to a depth of 308 µm (STD 15) and 307 µm (SD 18) in the 15-minute and 30-minute UVA-irradiated groups. No autofluorescence was detected in the control groups. The overall intensity of autofluorescence was 7,805 (SD 5,421) arbitrary units (au) x µm in the 15-minute and 11,406 (SD 5,693) au x µm in the 30-minute UVA treatment groups. There was a significant relationship between CAF and change in stiffness (R2=0.81, p<0.001)
The group says the findings indicate that CAF signal might be used to assess UVA cross-linking in the cornea, especially the depth and amount of cross-linking induction by irradiation-dependent cross-linking variables such as intensity and duration of irradiation.4985
Surgeons in
They performed cross-linking on 59 eyes (50 patients), 40 eyes with keratoconus and 19 eyes with ectasia and assessed clinical outcomes including UCVA, BCVA, manifest cylinder, and manifest refraction spherical equivalent pre- and one year postoperatively. Topography changes using the Pentacam (Kmax and Kavg) were also determined.
In the entire cohort, mean UCVA preoperatively was 20/149 and postoperatively was 20/133 (p=0.11). BCVA was significantly improved from 20/47 to 20/35 (p<.001). MRSE improved by 1.9 D (p=0.04), although manifest cylinder remained unchanged after cross-linking. Topographically, Kmax flattened by 2.5 D (p=0.01) and Kavg flattened by 0.8 D (p<.001) at one year. Corneal hysteresis and corneal resistance factor (by Ocular Response Analyzer) did not significantly change following cross-linking.
In the stratified subgroups, keratoconus eyes showed no significant change in UCVA while BCVA improved from 20/51 to 20/37 (p<.001). MRSE improved by 1 D (p=0.11), but failed to reach statistical significance. Manifest cylinder remained unchanged after cross-linking. Topographically, Kmax flattened by 3.1D (p=0.02) and Kavg flattened by 0.8D (p<.001). No significant changes in CH or CRF were seen.
Similarly, ectasia eyes showed no significant change in UCVA while BCVA improved from 20/38 to 20/30 (p=0.003). MRSE improved by 1.5D (p=0.21) but failed to reach statistical significance. Manifest cylinder remained unchanged after cross-linking. Topographically, mean Kmax decreased by 1.1D (p=0.08), and Kavg failed to reach significance as well. No significant changes in hysteresis and resistance factor were seen.3474
Another group evaluated a novel, reproducible corneal OCT (cOCT) findings the first six months and at least three years following collagen cross-linking for keratoconus.
The study enrolled 125 keratoconus patients in
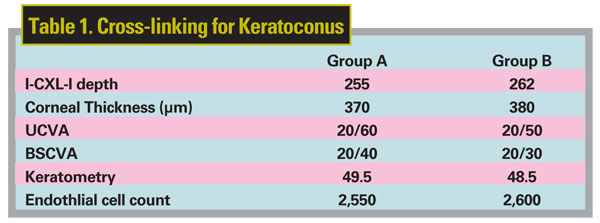
The mean follow-up time was seven months (Group A) and 38 months (group B). In Group A, 68 of 71 patients demonstrated I-CXL-l; in Group B, 51 of 54 did so. The mean values for group A and group B are shown in Table 1, above.
cOCT appears to demonstrate reproducible early and long-term corneal findings in eyes treated with CXL, suggesting the use of cOCT as a possible novel non-invasive measurement to evaluate and titrate intrastromal effects of this treatment in keratoconus eyes, the researchers conclude.4993
Lamellar Keratoplasty
Fibrin glue may be used as a modified technique to attach the corneal button in DALK without the use of sutures, say surgeons at the
The researchers performed deep anterior lamellar dissection on 10 human eye globes and 10 eye bank donor corneas using the Anwar big-bubble technique. Microkeratome-cut lamellar buttons were then placed on the recipient residual stromal bed. In five of the eyes, 16 sutures were placed to secure the button; in the other five eyes, they used fibrin glue to oppose the wound edge. They took high-resolution images of the wound edges and interface with the anterior segment OCT .
OCT evaluation demonstrated that the corneal wound edges in DALK that were applied with fibrin glue showed a smooth and regular surface comparable to the traditional 16-suture method. The fibrin glue method also resulted in reduced operation time.
Future experiments utilizing this technique with the femtosecond laser-assisted cut may show even better results by providing more precise approximation of the wound edge.735
Investigators at the
Injection of air or collagenase into the deep corneal stroma did not result in a reproducible separation of the stroma/Descemet's junction. In contrast, deep stroma and Descemet's membrane were easily and reproducibly separated using a combination of Collagenase and air injection. The separation was confirmed using Visante OCT, light microscopy and electron microscopy. The cleavage plane seems to be located between the junction of the posterior stroma and the anterior banded layer of Descemet's membrane.
The group says future applications include harvesting of Descemet's membrane for endothelial transplantation, and the technique may be considered as an adjuvant for the big-bubble technique.739
The big-bubble technique, as originally described by Dr. Mohammed Anwar, achieves successful DALK with excellent clinical results. The comparatively fast visual recovery is attributed to the deep dissection achieved with this technique that presumably creates a clean plane of separation between the corneal stroma and Descemet's membrane. A group from Devers Eye Institute, Portland, Ore., and Washington University, St. Louis, performed OCT and histologic assessment of eye bank corneas on which DALK was performed, utilizing both big-bubble and manual dissection techniques, to assess precisely the depth of the dissection plane.
Human corneoscleral rims were mounted on an artificial chamber and the big-bubble technique attempted. After surgical preparation, the specimens remained mounted on artificial anterior chambers for photographic and anterior segment OCT evaluation. The specimens were fixed in formalin and histologic assessment was performed.
In three corneas, the big bubble was successfully achieved with clinically apparent baring of Descemet's. In one of those three, the big bubble ruptured through Descemet's during the manual dissection of the overlying stromal tissue. Intraoperative and OCT examination revealed that the rupture occurred at the site of a prior cataract surgery wound. In a fourth tissue the big bubble could not be obtained and a manual cut-down to near Descemet's was completed. Photographic and OCT evaluation revealed a smooth interface with apparent dissection to Descemet's in the three big-bubble technique tissues. The specimen that underwent manual dissection displayed a satisfactorily thin posterior lamella. Histological evaluation, however, revealed a single collagenous lamella of corneal stromal tissue adherent to Descemet's in the big-bubble cases.
The group concludes that the study provides histopathologic evidence that the dissection plane occurs in the deep stroma and leaves a single layer of stroma adherent to Descemet's. Unlike the Descemet's membrane stripping step of DSAEK surgery, the DALK dissection does not occur between the stroma and Descemet's, as is commonly postulated. In cases where the big bubble cannot be achieved, adequate depth of dissection approaching that of the big bubble can be accomplished with manual dissection. Prior cataract surgery incisions may be a risk factor for failure of the big-bubble technique.738
Surgeons in
By light and electron microscopy, they analyzed the excised anterior corneal lamellae of 10 keratokonus patients who underwent DALK using the big-bubble technique. In addition, clinico-pathological correlations and immunohistochemistry were done. Intrastromal air accumulations were quantified morphometrically.
Intrastromal air was detected in all examined excised lamellae (overall 8 percent of stromal volume), but with a large variability (SD 8.8). Intrastromal air bubbles were characterized by round shape, mean size of 1,379 µm² (SD 1,031) and surrounding collagen displacement causing a "pseudo capsule." The air was predominantly located at one periphery of the excised lamella and represented up to 38 percent of stromal volume. The different distribution of intrastromal air in the periphery was statistically significant (p=0.016).To differentiate intrastromal air from histopathological differential diagnoses, they performed a CD68 staining, which was negative. Light and electron microscopy detected no air-injection induced alterations of Bowman's layer and epithelium.
They caution that pathologists should be conscious of this phenomenon and the high topographic variability. Intrastromal air in the recipient rim may be accompanied by a decrease of mechanical stability and may contribute to postoperative suture loosening. In consequence, the surgeon should try to limit the injection of air to the excised central stroma.737
Keratoprosthetics
Researchers at the Massachusetts Eye and Ear Infirmary in
All five patients had count fingers vision or worse in their better eye prior to surgery. Four of the five patients underwent Kpro surgery due to ocular surface failure secondary to Stevens-Johnson syndrome. One patient had severe atopic keratoconjunctivitis with corneal ulceration and multiple failed corneal grafts. All patients were treated with mycophenolate mofetil at least one month prior to undergoing Kpro surgery. All patients achieved improvement in visual acuity, although follow-up times varied. One patient had a wound leak due to corneal melting after starting low-dose mycophenolate mofetil; she underwent Kpro replacement and her mycophenolate mofetil dose was increased. No patients had significant adverse effects from mycophenolate mofetil. Prior retinal disease and glaucoma limited visual recovery in two patients. They conclude that treatment with immunosuppressive therapies prior to implantation can reduce risk of Kpro failure and vision loss in this group of patients.1146
Another group from Mass Eye and Ear, this one from the Retina Service, reports the first description of risk factors significantly associated with retinal detachment. The study reviewed 205 eyes from 170 patients who received a Boston KPro by the same surgeon over 13 years and statistically compared incidence rates of RD.
The mean number of KPros implanted per eye was 1.3 (r: one to four) with an average follow-up period after the first surgery of 3.9 years. Forty-four eyes (21.5 percent) developed a retinal detachment after a mean of 2.6 years (r: one month to 9.5 years) of follow-up. Significant predictive factors for retinal detachment included: the formation of a retro-KPro membrane (p<0.001); the occurrence of sterile vitritis (p<0.001) or endophthalmitis (p=0.002) after KPro; having had a KPro replacement in the same eye (p=0.006); and aqueous humor leak in the postoperative period (p<0.001). Patients who received a KPro because of an autoimmune or systemic disorder affecting their cornea (as opposed to a local pathology) were also found to be at an increased risk of retinal detachment (p<0.001). Lens status at time of surgery, anterior vitrectomy performed at the same time as KPro, tube shunt placement at the same time or after KPro and YAG laser membranectomy or capsulotomy were not found to be predictors for retinal detachment. The calculated incidence of retinal detachment in the entire study population was 8.3 percent at one year. Among all patients who developed a retinal detachment, 14 (32.6 percent) occurred within the first year after surgery, 26 (60.5 percent) occurred within three years and 37 (86 percent) occurred within five years.1140
Surgeons from the
Six of the eight patients (75 percent) have active device retention, superior to that in the reported literature. In six active patients, two patients have BCVA of 20/40 or better whereas four have vision of 20/200 or worse (r: 20/20 to count fingers at one foot). Pre-existing end-stage glaucomatous optic neuropathy is the reason for poor vision in three of the four poorest-seeing eyes. Stromal melting occurred in three patients despite use of Medroxyprogesterone topically. Of these, two were successfully treated with a lamellar onlay keratoplasty. Retroprosthetic membrane formation occurred in four of eight patients. Two of these occurred in patients with Type I surgery and two occurred in patients with Type II surgery. No retroprosthetic membranes occurred with Type III surgery, superior to outcomes in the reported literature. Type III surgery may lead to less retroprosthetic membrane formation. Type II surgery followed by use of a piggyback contact lens fitting system is required for best visual performance in eyes with excellent visual potential.1151
New Technology
Investigators in
They collected data on uncorrected visual acuity, best spectacle corrected VA, corneal astigmatism, corneal pachymetry, endothelial cell density, corneal curvature and contrast sensitivity on 21 femto-ALK eyes, 19 femto-DALK eyes and 21 mDALK eyes.
There was no significant difference between the femto-DALK and the mDALK in UCVA, BSCVA and contrast sensitivity; nor was there any significant difference between the three techniques in cell density count, corneal curvature and corneal pachimetry. The major difference was found in UCVA and BSCVA recovery time, and in contrast sensitivity results between the DALK techniques and the ALK technique, in which the worst results during the first year of follow-up were related to the interface scarring.1130
Besides cutting the donor and host cornea in an interlocking pattern intended to promote precise anterior-posterior tissue alignment and increased wound stability, the femtosecond laser can create radial alignment marks on both donor and host to promote more even tissue distribution, suture length and radiality. A group at the Gavin Herbert Eye Institute,
They retrospectively compared 99 cases of femtosecond laser-enabled keratoplasty (FLEK) with or without 12 radial alignment marks in donor and host cornea. All cases used a zig-zag incision. Postoperative astigmatism based on simulated keratometry and manifest refraction was compared at one, three, six and nine months after surgery; the results appear in Table 1.
There was no significant difference found in postoperative astigmatism comparing surgeries done with versus without radial alignment marks (all p values >0.17). Despite the surgeons' subjective sense during surgery that the radial marks assisted in achieving even tissue distribution, suture length and radiality, the data suggests no difference in outcome.
Radial alignment marks may assist in achieving even tissue distribution, suture length and radiality in FLEK, but this analysis of cases performed with and without radial marks shows no difference in postoperative astigmatism.1119
Keratoconus
Is an irregularly shaped posterior cornea a better indicator of keratoconus than the anterior surface that is often used in keratoconus screening? Researchers at several institutions in
They collected Pentacam data of 18 keratoconus and 22 astigmatic eyes in this study. Within the keratoconus eyes, eight were mild with manifest BCVA of 20/25 or better. The forme fruste keratoconus diagnosis relied on the other eye's condition from the same subject, other keratoconus indications and family history. The remaining keratoconus eyes comprised five moderate cases with a BCVA of 20/30 to 20/40, and five that were worse than 20/40. The 22 astigmatic eyes all had a BCVA of 20/25 or better. Posterior and anterior elevation maps were decomposed into Zernike polynomials to obtain the root mean squared error (RMSE) above the 2nd order that represents high-order complex patterns. The difference between the two RMSE values was used as a third indicator. The extreme RMSE values of the astigmatic eyes were used as the screening criteria (i.e., 100 percent specificity).
The 7-mm diameter cornea decomposition found that the anterior RMSE missed seven of the 18 keratoconus eyes (61 percent sensitivity); five in the forme fruste keratoconus, one in moderate, and one in advanced. Both posterior and the RMSE difference missed four of the 18 (78 percent sensitivity); three forme fruste keratoconus and one moderate keratoconus. The 6-mm result showed that the anterior missed seven of the 18 (61 percent sensitivity); five forme fruste keratoconus, one moderate, and one advanced.
The posterior and the RMSE difference missed six of the 18 (67 percent sensitivity); five forme fruste keratoconus and one moderate keratoconus. The 5-mm result found that the anterior missed eight of the 18 (56 percent sensitivity); five forme fruste keratoconus, two moderate, and one advanced. The posterior missed six of the 18 eyes (67 percent sensitivity) and the RMSE difference missed five of the 18 (72 percent sensitivity).
The posterior cornea surface alone provides more significant indication of keratoconus than the anterior surface. Analysis with a larger cornea area improves detection sensitivity. Either anterior or posterior cornea irregularity is a sufficient indicator of early keratoconus, but sometimes additional information is required to clinically diagnose forme fruste keratoconus.4963
Miscellaneous
Azithromycin 1.5% eye drops are a potent treatment for phlyctenular keratoconjunctivitis complicating childhood ocular rosacea, according to a study in
The retrospective study included 15 children suffering from ocular rosacea who were treated with azithromycin 1.5%. Nineteen eyes of eight boys and seven girls, aged 8 ±4 years were treated. The disease was resistant to lid hygiene in 15 cases, to oral erythromycin in two cases, and to topical steroids in three cases. All patients suffered from phlyctenular keratoconjunctivitis with blepharitis. They received azithromycin 1.5% b.i.d. for three consecutive days every 10 days, associated with lid hygiene. Ocular redness resolved within two months whereas phlyctenular keratoconjunctivitis healed within four to six months in all cases. Palpebral inflammation partially decreased in 13 patients. Treatment was stopped after six months without recurrence (follow-up, three to nine months without treatment).
A team from
While glaucoma prevalence varies by race, in the Ocular Hypertension Treatment Study a thin CCT and optic disc cupping accounted for an increased risk of POAG in blacks.
In the study, 556 eyes (302 consecutive patients) underwent comprehensive ophthalmic evaluation including intraocular pressure measurement by Goldmann applanation, CH and corneal compensated IOP (by Ocular Response Analyzer), CCT by ultrasonic pachymetry, and mean deviation (MD) by 24-2 SITA standard automatic perimetry.
CH and CCT were significantly different among 166 black, 196 Hispanic and 195 white patients (p<0.001). The mean CH was 8.4 mmHg and CCT was 530.5 µm in blacks, 9.6 mmHg and 544.5 µm in Hispanics, and 9.7 mmHg and 551.6 µm in whites. These differences remained significant after controlling for age, sex and MD (p<0.001). CH, but not CCT, was associated with worsening MD (p<0.05). There was evidence of statistically significant effect modification, with the magnitude of change of MD as a function of CH greatest among whites and least among Hispanics (p<0.05; See Figure XX). The predicted change in MD (dB) with a one standard deviation increase of CH (2.64) was 1.78 for whites, 0.83 for blacks and 0.31 for Hispanics.
Hysteresis was significantly different among whites, blacks and Hispanics. Across races, lower corneal hysteresis was associated with a worsening MD. This association appears greatest in whites and lowest among Hispanics.4624
Dr. Afshari is an associate professor of ophthalmology at the





