At the meeting of the Association for Research in Vision and Ophthalmology in May, the enormity of the conference hall and the quantity of research it contained left no doubt as to the volume of important work being conducted. If you couldn't be there in person, though, this article will help catch you up on the latest findings in the areas of allergy and dry eye, focusing on pathophysiology, in vitro work and clinical studies.
Allergy
• Pathophysiology. When allergens cause a mast cell to degranulate, tumor necrosis factor-alpha is among the released contents. Upon its release, TNF-alpha causes the upregulation of intracellular adhesion molecule-1 on endothelial cells. From this position, ICAM-1 attracts inflammatory cells flowing past in the bloodstream. These cells, such as eosinophils, adhere to ICAM-1, infiltrate the tissue and start causing damage. Exposure to allergen and mast-cell degranulation clearly have key roles in instigating this upregulation of ICAM-1 expression, and the subsequent, potentially damaging, effects.
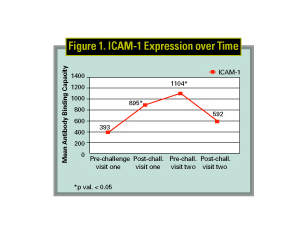
In researching this relationship, one study considered the expression of ICAM-1 in repeated exposure to allergen. In this study, researchers used the conjunctival allergen challenge model to expose subjects to allergen twice within a 24-hour period. Using impression-cytology samples taken before and after each challenge, they found that, after the second challenge, the ICAM-1 expression was significantly less than after the first, suggesting that there may be a negative feedback mechanism in the expression of ICAM-1 (See Figure 1). (Tinios L, ARVO Abstract #3742, 2003)
 |
Several studies also investigated the manifestation of severe forms of allergic disease. The late phase of severe forms of allergic conjunctivitis was investigated in a study of prostaglandin D2 (PGD2), in which study doctors found a direct correlation between the severity of disease and the concentration of PGD2 in tears. (ARVO 2003, #3746) In vernal keratoconjunctivitis, research found that an imbalance of the levels of plasminogen and plasminogen activator inhibitor may contribute to the development of VKC. (Fujishima H, ARVO Abstract #673, 2003)
• Therapies. Research into agents to treat allergic conjunctivitis involved studies of several products, including EPC-K1, a phosphodiester of vitamins C and E. EPC-K1 exhibited potential applicability in the treatment of severe forms of ocular allergy such as VKC and atopic keratoconjunctivitis, as it appeared to be effective in attenuating eosinophilic inflammation. (Okada N, ARVO Abstract #3744, 2003)
Two different environmental-model studies examined the safety and efficacy of epinastine 0.05% HCl. They found that epinastine was superior to placebo and provided numerically better relief of ocular itching than another ocular antihistamine, levocabastine (Livostin, Novartis), and that it was safe and well tolerated in healthy adults and seasonal allergy patients. (Whitcup SM, ARVO Abstract #3729, 2003)
A new product containing olopatadine 0.2%, which is twice the concentration of active drug in Patanol (olopatadine 0.1%, Alcon), was tested for a 16-hour duration using the conjunctival allergen challenge model. Q.d. olopatadine 0.2% was effective for at least 16 hours, implying that less-frequent dosing of the new formulation will have the same potency and enhanced mast-cell stabilizing ability as b.i.d. dosing with a 0.1% formulation. (Abelson M, ARVO Abstract #3736, 2003)
Clinical study of dosing regimens also included evaluation of pemirolast 0.1% (Alamast, Santen) used b.i.d. versus q.i.d. for seasonal allergic conjunctivitis. The two regimens were proven to be equivalent in their efficacy and tolerability. (Gous P, ARVO Abstract #3732, 2003)
Evaluation of ketotifen fumarate (Zaditor, Novartis) found it to be a safe, effective treatment in a pediatric population for at least eight hours as evaluated by the conjunctival allergen challenge model, both after a single dose of medication as well as after a four-week b.i.d. treatment period. (Crampton J, ARVO Abstract #3728, 2003)
Clinical study of existing therapies also included examination of effects on the chemical mediators of allergy. A study of olopatadine looked at mediators released from the mast cell in relation to clinical symptoms. In the past, in vitro models have been used to evaluate the efficacy of mast cell stabilizing ability of anti-allergics. This study of olopatadine, however, revealed a reduction in the release and effect of mediators such as histamine, neutrophils and eosinophils, as well as ICAM-1 expression, and correlated these indices with the clinical effect in ocular allergy subjects. Olopatadine has now demonstrated both in vitro (in past studies) and in vivo mast-cell stabilization (in this study) on human conjunctival mast cells. (Nichols L, ARVO Abstract #3747, 2003)
There were other mediator-focused studies using several current therapies. A study of the effect of ketotifen on eosinophil chemotaxis, oxidative metabolism and mediator release found that the agent inhibited chemotaxis of eosinophils (purified from normal or hypereosinophilic human donors) in a dose-dependent manner. This means ketotifen is able to limit the number of eosinophils at the site of the allergic reaction, which may be applicable in severe forms of allergy such as VKC and AKC. (Lanz R, ARVO Abstract #1294, 2003)
Researchers also explored the use of the new cyclosporine A 0.05% emulsion Restasis (Allergan) in the setting of severe, steroid-resistant atopic keratoconjunctivitis. Twenty-two patients were randomized to treatment with topical cyclosporine A or placebo and were followed for four weeks. The researchers found a greater improvement in signs such as bulbar conjunctival hyperemia and corneal neovascularization, and in symptoms such as itching, tearing and discomfort. They reported no adverse effects from the treatment. (Gottsch JD, ARVO Abstract #672, 2003)
Along the same lines as the ketotifen study mentioned above, an in vitro study of nedocromil (Alocril, Allergan), in a human conjunctival cell line, investigated inhibition of ICAM-1 and the chemokine RANTES; both are expressed by conjunctival epithelial cells during an allergic reaction to help recruit leukocytes, which are involved in the late-phase allergic response and in chronic allergy. Inhibition of ICAM-1 and RANTES with preincubation of cells in nedocromil (incubations of one to six hours) was evident. (Sra KK, ARVO Abstract #3741, 2003)
Researchers also presented new ideas in study design and models of ocular allergy. A model was used for a comparative study of drug interaction with and effects on cell membranes. The model used changes in surface pressure or leakage of mediators such as histamine to measure membrane stability after drug exposure. Drugs tested included desloratadine (Clarinex, Schering-Plough), clemastine (Tavist, Novartis Consumer Health), azelastine (Astelin, MedPointe Pharmaceuticals), ketotifen, olopatadine and epinastine. Olopatadine disrupted cell membranes the least. (Graff G, ARVO Abstract #3723, 2003)
The need to relate clinical evaluation parameters to pollen counts in the study of allergy has long been an issue. A retrospective analysis of pollen-count data and ocular-itching scores in a multicenter environmental study addressed this problem in a new way. In the study, pollen-count data for each site was divided into four quartiles, of which the highest quartile for pollen count was correlated with ocular itching scores. Despite the difference between the absolute pollen levels at the various sites, analysis revealed that, as pollen levels increased by quartile, greater percentages of patients had elevated itching severity. The absolute pollen counts from various geographic locations were poor predictors of itching severity scores. The researchers showed that there's much potential for improvement in our pollen collection and data analysis methods in allergy studies. The study's quartile analysis is an interesting example of new ways to look at pollen-related signs and symptoms. (Rosner S, ARVO Abstract #3766, 2003)
Dry Eye
• Procedures and therapies. Dry eye is a complex disease influenced by many factors, creating the potential for different treatments. Some treatments discussed at ARVO include topical therapies and dietary modifications.
One topical treatment proving to be effective is a new artificial tear solution containing HP-Guar (Systane, Alcon). The mechanism is believed to involve the binding of the HP-Guar molecule to the desiccated regions of ocular surface epithelial cells. Subsequent cross-linking then forms a framework with the existing tear-film components, extending their retention time on the surface. This drop showed significant decreases in the duration of corneal and conjunctival staining compared to placebo. And it showed significantly less morning and evening dryness and less foreign-body sensation compared to the control. (Christensen MT, ARVO Abstract #2483, 2003)
 |
One of the more recent advances in dry eye involves diet modification. As part of the Women's Health Study, researchers selected 39,876 women and studied their intake of omega-3 fatty acids. They found that women consuming higher levels of the acids were less likely to develop dry-eye. (Trivedi KA, ARVO Abstract #811, 2003)
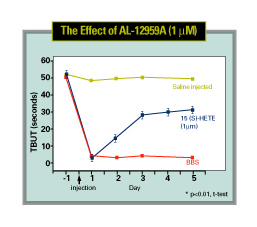
Presenters also discussed the mucin secretagogue 15-HETE at ARVO. In one study, researchers assessed tear-film function, corneal integrity and inflammation in rabbits whose lacrimal glands were injected with the T-cell mitogen Concanavalin A. ConA was used as a model because it increased inflammation in the gland, significantly reduced tear-film breakup time, and increased susceptibility to corneal damage. The application of 15-HETE restored tear-film breakup time and prevented corneal staining, helping to protect the epithelial cells. (Gamache DA, ARVO Abstract #2498, 2003)
• Dry-eye mechanisms. The underlying components of dry eye were also explored at ARVO. One study examined the interactions of tear proteins on the ocular surface. Meibum, albumin, ß-lactoglobulin, lipocalin, lysozyme, lactoferrin and human tears all showed dynamic surface activity, providing evidence that these proteins are major contributors to the surface activity of the tear film. (Tragoulias S, ARVO Abstract #2500, 2003)
A second study focused on the detection of the chemokine receptor CCR5 on conjunctival epithelial cells. CCR5 is a receptor for a chemotactic cytokine that regulates the immune response in tissues by mediating the T-helper-1 type of immune response. The study found that patients with dry eye had more CCR5 on conjunctival epithelial cells than normals, indicating an immunoinflammatory ocular surface response. These data suggest that new therapies involving chemokine-receptor blockades could help decrease the immunoinflammatory response associated with dry eye. (Sood A, ARVO Abstract #671, 2003)
• Corneal sensitivity. Researchers found that patients with low corneal sensitivity tend to take longer to experience symptoms when exposed to an adverse environment, as evidenced in a study using a controlled adverse environment model. (Emory T, ARVO Abstract #2486, 2003) Further, in a significant portion (42 percent) of dry-eye patients, reduced corneal sensitivity leads to a tendency to blink less than those dry-eye patients with normal sensitivity, supporting the neural-loop theory of dry eye.
Meanwhile, dry-eye patients with normal corneal sensitivity tended to blink twice as frequently as normals. (Nally L, ARVO Abstract #2488, 2003) Thus, patients with normal sensitivity are better able to compensate for their decreased tear-film breakup time by increasing blink rate, helping reduce the amount of time the ocular surface is exposed.
In another study examining dry-eye patients and corneal sensitivity, researchers looked at the relationship between the duration and severity of ocular symptoms and sensitivity. Eighty-two patients were classified as having low or normal corneal sensitivity. In the study, the duration of dry-eye symptoms correlated with sensitivity, but both groups reported similar discomfort. The results suggest that patients with dry eye experience low levels of discomfort when not exposed to an adverse environment, creating a symptom "zone." This zone may be due to altered blink rate and reflex tearing. (Ousler GW, ARVO Abstract #2484, 2003)
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. MacDonald and Ms. Humphrey are research associates at Ophthalmic Research Associates in North Andover.



