Recently, a new instrument from Reichert Ophthalmic Instruments—the Ocular Response Analyzer—has made it possible to quantify entirely new information about the biomechanical properties of the cornea. The resulting data are not only making it possible to eliminate confounding factors from IOP measurements, they are broadening our understanding of the cornea and potentially providing new ways to detect and monitor disease progression.
Here, we look at the science behind this new technology, and some of its potential uses.
Measuring Dynamic Resistance
Corneal tissue displays three different kinds of resistance to an outside force: 1) resistance generated by the pressure inside the eye; 2) static resistance generated by the tensile strength and elasticity of the tissue; and 3) dynamic resistance to rapid movement generated by the viscous nature of the tissue. The ORA is unique in that it measures the latter, offering a new parameter referred to as corneal hysteresis.
Dynamic resistance creates a damping effect; this is what you encounter when trying to run in a swimming pool or trying to compress a shock absorber. The faster you attempt to do it, the greater the resistance you encounter. For that reason, unlike the static resistance you encounter when pushing against a spring made of a homogenous material such as plastic or steel, dynamic resistance is rate-dependent.
The fact that corneal static resistance and dynamic resistance are different can be demonstrated by measuring corneal resistance before and after adding a bandage contact lens to the eye. Adding the lens increases the static resistance, or springiness, of the cornea. But it has no significant effect on hysteresis—the resistance to rapid movement. Similarly, changing IOP has no significant effect on hysteresis; elevating pressure artificially doesn't alter the hysteresis reading, though it does impact the level of static resistance, or elasticity.
Since hysteresis is a rate-dependent effect, one way to measure it in the cornea is to move the tissue rapidly, inducing a measurable damping effect. This is exactly what the ORA does. When a rapid air pulse is used to indent the cornea, the dynamic resistance of the tissue causes a slight delay in the movement both inward and back out, which the ORA can detect. In a standard noncontact tonometer measurement this is confounding factor. However, once you understand the existence and nature of this factor, you can isolate and measure it, learn how it correlates to different corneal conditions, and remove it from the pressure measurement to increase the accuracy of the IOP reading.
Measuring Hysteresis
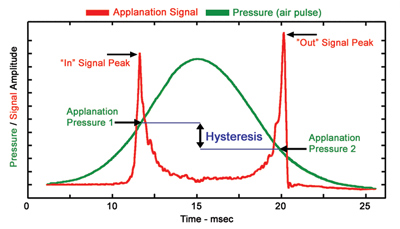
Here's what happens when the ORA takes a measurement. First, the instrument uses a very precise eye-tracking system to locate and lock onto a 0.002-inch target on the apex of the cornea. Then the ORA applies a rapid but variable pressure to the eye using a "fully developed turbulent jet flow"—a column of air that maintains its shape and pressure as it impacts the eye. The air pulse generated by the ORA ramps up and down very precisely over a 20 millisecond period, following a curve like that in Figure 1 (below). At the same time, the electro-optical system takes 400 data samples.
The ORA uses just enough pressure to push the corneal tissue slightly past applanation (flatness). In fact, it customizes the amount of pressure used for every eye, so no eye is subjected to more pressure than is necessary. At the same time, the ORA uses reflected light and sensors to identify the exact moment of applanation on the way in and out, noting the air pressure being exerted at both moments.
Because the damping effect causes a delay in the tissue movement response, the pressure of the air column when the tissue reaches applanation on the way in is slightly greater than it would be if no damping were taking place. For the same reason, as the pressure drops, the tissue resists moving back out; so when the cornea reaches applanation for the second time, as it moves back out, the pressure has dropped a little more than it would have if no damping effect were present. The measured difference between the pressures recorded at the two moments of applanation equals the corneal hysteresis.
According to the company, clinical studies have shown that this measurement corresponds quite directly with material properties of the cornea. In fact, Reichert says this number changes dramatically between normal and compromised corneas, including corneas after LASIK.
Unlocking More Information
Even though the key measurement, hysteresis, is based on the pressure at the two moments of applanation during the rise and fall of the applied air pressure, the instrument monitors the deformation of the cornea throughout the entire process. So, every eye produces a unique waveform that varies with corneal characteristics.
Reichert's ORA measures the delay in tissue movement in and out caused by the cornea's viscoelastic resistance, an indicator of biomechanical condition.
That waveform may contain significant information that has yet to be quantified. Dave Taylor, clinical manager at Reichert Ophthalmic, says that during five years of clinical studies he has seen thousands of these waveforms. As a result, simply by seeing the shape of the waveform, he can tell whether an eye has had LASIK or PRK, or has keratoconus—without even seeing the numbers. "One of our clinical sites sent us 100 measurement signals with all the numbers removed," he says. "Fifty of the eyes had keratoconus, 50 did not. The inventor of the ORA, Dr. David Luce, was able to correctly identify 45 of the 50 keratoconus eyes just by looking at the waveforms."
While the process of extracting information from these waveforms is undoubtedly in the early stages, researchers at Reichert have already combined this data with other numbers in different ways to reveal additional useful information. Measurements currently offered by the instrument include:
• IOPG. This number is the average of the two applanation point readings; it correlates very well with a standard Goldmann tonometer reading.
• Corneal-compensated IOP (IOPcc). This measure appears to eliminate much of the impact of corneal biomechanical characteristics.1 Mr. Taylor explains: "After studying hundreds of thousands of data points, we learned that P1 and P2—the two sequential applanation pressure measurements—actually give us different information about corneal properties," he says. "For example, we found that P1 drops a lot after LASIK, while P2 hardly drops at all. That makes it possible to combine the two numbers mathematically to produce a pressure reading that doesn't change after refractive surgery. [Goldmann readings typically drop 3 or 4 mmHg after LASIK.] We call that number IOPcc. This number, in effect, removes the corneal confounding factors from the measurement."
• Corneal resistance factor (CRF). Unlike IOPcc, which largely eliminates cornea confounding factors, CRF maximizes the impact of those factors, providing a way to measure their impact. "In this case, we found a mathematical way to make the P1 and P2 measurement have maximum correlation to central corneal thickness—the only other corneal parameter we can easily use," Mr. Taylor explains. "Normally hysteresis only correlates weakly to CCT in a healthy eye. CRF maximizes that correlation, thereby reflecting the overall biomechanical strength of the cornea. After refractive surgery, for example, hysteresis drops significantly—but CRF drops even more, reflecting the impact on the cornea's viscoelastic resistance."
Mr. Taylor notes that this measurement can be extremely useful for a surgeon trying to decide whether to perform LASIK on a borderline patient. "These biomechanical metrics can tell us a lot about susceptibility to corneal pathologies," he says. "Keratoconic patients have significantly lower CRF and hysteresis measurements. LASIK tends to lower hysteresis by two or three units. So if a borderline potential LASIK patient has a hysteresis number that falls at the bottom end of the normal population, the surgery will probably push that number down into the range found in keratoconus patients." Mr. Taylor adds that most of the doctors currently buying the ORA are refractive surgeons who are using it for this purpose.
The Glaucoma Connection
One of the possible uses of this new corneal data is in the field of glaucoma management. According to Mr. Taylor, three independent studies (one still unpublished) have shown that low hysteresis is a powerful predictor of glaucoma progression.
"In one study of 229 patients with controlled glaucoma, done by Drs. Condon and Quigley at Wilmer Eye Institute," he says, "the hysteresis measurement was more powerful than IOP or CCT in identifying which patients were still progressing.2 Another study done at the Children's University Hospital in Dublin, Ireland, compared the hysteresis values of normal children to those of children with congenital glaucoma. Their hysteresis readings were totally different; there was hardly any overlap between the two populations. And the readings were independent of IOP.3
"Lower-than-average hysteresis has also been associated with individuals identified as having normal tension glaucoma," he adds. "Our studies found that the ORA's IOPcc measurement was more than 2.25 mmHg higher, on average, than the ORA's Goldmann-correlated IOPG measurement in a population of 24 NTG eyes."
It seems clear that the data being uncovered by the Ocular Response Analyzer has ramifications that are barely beginning to be discovered. "Right now there are a host of studies going on, because most of the people who are buying the ORA are doing research with it," notes Mr. Taylor. "I'm biased, but I think it's very exciting. It's opened up a whole new area of research that didn't exist five years ago."
In addition to the measurements described above, the ORA includes a built-in 20 MHz ultrasound pachymeter and a patient-management database; Reichert says it may soon have a CPT code for the corneal hysteresis measurement, as well. For more information, call 1 (716) 686-4500, or visit ocularresponse-analyzer.com or reichertoi.com.
1. Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma 2006;15:364–370.
2. Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol 2006;141:5:868-75.
3. Kirwan C, O'Keefe M, Lanigan B. Corneal hysteresis and intraocular pressure measurement in children using the Reichert ocular response analyzer. Am J Ophthalmol. In press.



