Presentation
An 80-year-old male presented for evaluation of decreased vision in his left eye. His clinical course began four years prior when he underwent combined phacoemulsification cataract surgery and Descemet’s stripping automated endothelial keratoplasty OS for what was described by an outside provider as a unilateral Fuchs’ dystrophy. His recovery had been complicated by several episodes of recurrent graft rejection over the four years. He subsequently developed significant cystoid macular edema, believed to be a consequence of both recurrent inflammation and pseudophakia. For management of his CME, he received two injections of sub-Tenon’s and 11 injections of intravitreal triamcinolone acetonide over four years. The patient then received an injection of intravitreal ganciclovir four months prior to his Wills Eye visit at an outside provider, with no improvement in his symptoms. He had subsequently developed new, painless, progressive, unilateral decreased vision, prompting referral to Wills Eye Hospital.
Medical History
The patient had an ocular history of unilateral corneal endothelial degeneration that required a combination phacoemulsification/DSAEK; cystoid macular edema; and steroid-induced glaucoma that had required the implantation of a tube shunt and an iStent OS. His medical history was notable for basal cell carcinoma. Family history was notable only for a sibling with diabetes. His ocular medications at presentation were brimonidine 0.2%-timolol 0.5%, sodium chloride 5%, difluprednate 0.05%, bromfenac 0.07% and cyclosporine 0.05% drops. His systemic medications were aspirin, vitamin B, saw palmetto, vitamin D and turmeric. He was retired with no recent travel or substance abuse history.
Examination
 |
 |
Ocular examination revealed visual acuity of 20/20 in the right eye and count fingers in the left. Pupillary examination showed a 1+ relative afferent pupillary defect OS. Intraocular pressure was 11 mmHg OD and 3 mmHg OS. Extraocular movements and confrontation visual fields were full bilaterally.
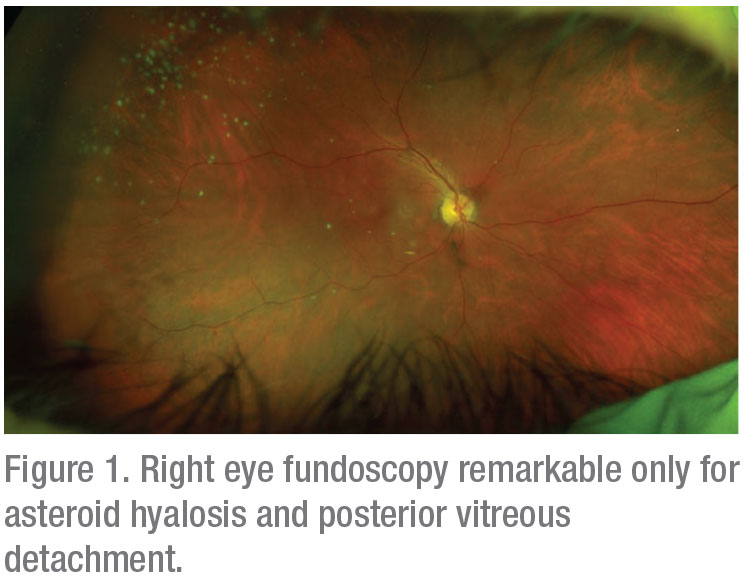
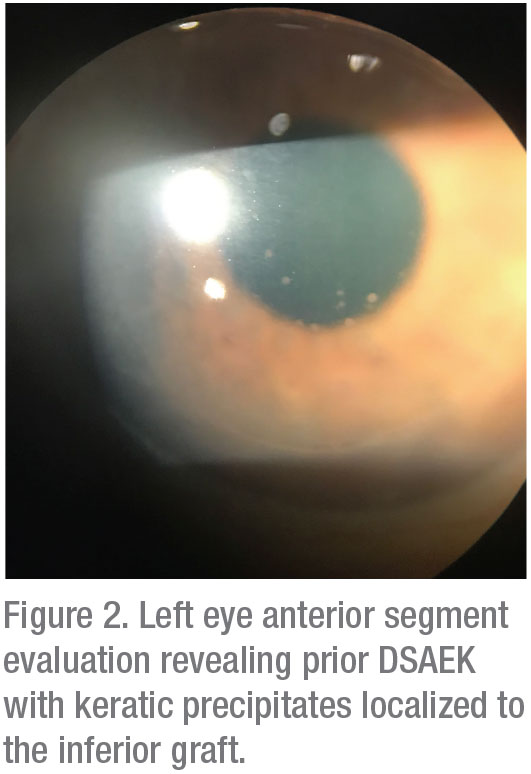
Anterior segment examination of the right eye was notable only for a posterior chamber intraocular lens with 1+ posterior capsule opacification, posterior vitreous detachment and asteroid hyalosis (Figure 1). Examination OS (Figure 2) showed 1+ conjunctival injection. The cornea showed a DSAEK with trace endothelial folds and 1+ keratic precipitates localized to the inferior graft. There was no evidence of a rejection line. The anterior chamber was deep with 1 to 2+ flare, a well-positioned tube shunt at 11 o’clock and a centered PCIOL.
Posterior segment examination showed trace vitreous cell, macular thickening and attenuated blood vessels. Most notable was flat, granular, hemorrhagic retinitis in the temporal periphery and a chorioretinal scar superiorly (Figure 3). The optic disc appeared healthy.
Fluorescein angiography of the right eye was grossly normal. Optical coherence tomography of the right macula showed PVD and scattered drusen. A fluorescein angiogram of the left eye showed granular, hemorrhagic temporal retinitis (Figure 4), and OCT of the macula showed retinal thickening consistent with macular edema as well as regions of necrotic-appearing retina (Figure 5).
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



