Today, refractive surgeons have multiple options to offer their patients, and the good news is that secondary glaucoma in refractive patients is not very common. However, refractive surgery and glaucoma management often interact, in part because the patient population that refractive surgeons deal with largely comprises myopes, and myopia is a risk factor for both glaucoma and steroidinduced ocular hypertension.1,2
Due to an increasing population of both glaucoma and refractive surgery patients, it's important for both refractive surgeons and ophthalmologists treating glaucoma to be aware of the ramifications of refractive surgery. On the one hand, refractive surgeons need to be on the lookout for patients who are at risk for glaucoma, to ensure that adequate preoperative data is collected to aid glaucoma treatment at a later date, if needed. Often, issues relating to glaucoma may not be at the forefront of refractive surgeons' minds; after all, most of these patients are young and relatively healthy. At the same time, those who treat glaucoma in patients who have had refractive surgery need to be aware of the ways in which this surgery impacts our ability to diagnose and monitor the disease.
Pre-Refractive Surgery Screening
One way to avoid glaucomatous problems during or after refractive surgery—and make future glaucoma treatment easier—is to take glaucoma into consideration when screening refractive patients:
• Be on the lookout for glaucoma risk factors. A key element of this is asking every patient about family history of glaucoma. Even if a family history of glaucoma is the only risk factor you find, that's sufficient reason to proceed with caution.
• Pay attention to optic nerve appearance. Before refractive surgery, it's standard to perform a slit-lamp exam and measure intraocular pressure, but it's also important to pay attention to the appearance of the optic nerve. Myopic discs are often difficult to interpret—sometimes even by trained glaucoma specialists—but if the optic nerve looks suspicious, that's a sign that glaucoma may be an issue. It will also be helpful for future monitoring if you document the condition of a suspicious optic nerve with photography or nerve fiber layer imaging. Generally speaking, the more information you gather preoperatively, the more it will help when a patient is treated for glaucoma later. Your data provides a baseline for comparison so we can see how things are changing.
• Take multiple IOP measurements before surgery. A single IOP measurement will not provide a reliable baseline for comparison after surgery. Take multiple measurements, preferably at different times of day.
• Perform gonioscopy. This is a part of the ocular exam that most refractive surgeons omit, but I always recommend it as a way to avoid missing some potential problems. Acute angle-closure glaucoma after hyperopic LASIK has been reported,3 and some cases of pigment dispersion syndrome may only be diagnosed by gonioscopic findings. Pigmentary glaucoma resulting from pigment dispersion syndrome is typically seen in young adult myopes, and is more often seen in men.
This is particularly important if you're considering implanting a phakic IOL behind the Iris. Pigment dispersion syndrome is a contraindication for placement of phakic IOLs.
• Consider using alternate methods to measure IOP. Although Goldmann tonometry is still considered the gold standard, it's well-established that the corneal alterations caused by the most common types of refractive surgery will cause it to produce inaccurate measurements postoperatively. That means that you can't rely on a comparison of preop and postop measurements, and you may have difficulty monitoring postoperative IOP for spikes or steroid-induced glaucoma. Some surgeons may attempt to compensate for the change in corneal thickness by using a formula to adjust the reading, but corneal ablation causes changes in corneal curvature and structure as well. For this reason, you can't just depend on algorithms that focus on changes in corneal thickness to provide an accurate compensation factor.
As mentioned earlier, multiple IOP measurements are helpful, and the difference between average preoperative and postoperative measurements may be used as a correction factor in post-refractive-surgery patients. In addition, tonometric devices other than a Goldmann tonometer may be of value.4 Some studies have shown that the pneumotonometer and Tonopen were less affected after surgery than Goldmann applanation tonometry. These instruments have a very small area of contact and thus are less likely to be altered by changes in the surface properties of the cornea. More sophisticated alternatives include the Dynamic Contour Tonometer, which is a non-applanation tonometer, and the Reichert Ocular Response Analyzer, which uses hysteresis to calculate the IOP. While some refractive surgeons may not own either of the latter two devices, they should consider investing in one as a way to address this key ramification of refractive surgery.
• Consider a glaucoma consultation. Some refractive surgeons may not be comfortable performing tests such as gonioscopy or monitoring with alternate IOP-reading devices. If that's the case and a patient has a suspicious-looking optic nerve or a strong family history of glaucoma, the surgeon can obtain a glaucoma consultation from a colleague. That colleague can give an opinion on whether the patient is a good candidate and whether further information should be gathered before subjecting this patient to a particular type of surgery.
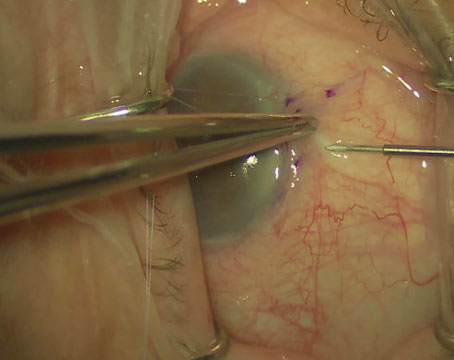
• If glaucoma risk is present, consider choosing a different refractive surgery. It's well known that marked IOP elevation occurs during formation of a corneal flap for LASIK surgery. This transient elevation in IOP may be as high as 90 mmHg, depending on the skill and technique of the refractive surgeon. Unfortunately, there have been reports of optic neuropathy and visual field loss after LASIK when the patient had a compromised optic nerve.5 So if a patient has some family history of glaucoma and a compromised optic nerve, LASIK may not be the best procedure for that patient. PRK or other refractive options might be worth considering, although post- PRK steroid treatment raises other potential concerns. The surgeon must decide what is the safest surgical intervention for each individual patient.
• Advise the patient to be checked for glaucoma periodically. Also, remind the patient that other ophthalmologists who may treat him in the future will need to know about the refractive surgery.
Postoperative Pitfalls
Glaucoma-related problems after refractive surgery center around accurate measurement of IOP and potential problems relating to steroid use. Strategies that may help include:
• Monitor carefully during steroid use. Myopia is a risk factor for steroid-induced ocular hypertension and glaucoma, and steroid-induced ocular hypertension or glaucoma can happen whenever steroids are used for an extended period of time—such as following PRK. Some refractive surgeons may not realize that myopes are more prone to developing steroidinduced ocular hypertension, and so may not be on the lookout for this type of problem. Especially close monitoring should be done if a patient has a family history of glaucoma, a connective tissue disease or diabetes, although the latter two are uncommon in a younger population.
• Watch out for confounding LASIK flap factors. As already mentioned, you can't rely on a Goldmann tonometer to provide accurate measurements of IOP after the cornea has been surgically altered. In addition, other factors may throw your reading off even further. If the flap becomes loose after LASIK, it will be easily distensible, adding to underestimation of IOP. An interface cyst can have the same effect.6 If the patient develops steroid-induced ocular hypertension when these factors are present, you almost certainly will miss it.
• Beware of pressure-induced interlamellar stromal keratitis (PISK). Although PISK is uncommon, it can cause devastating problems if it is undetected following LASIK.7 When present, it's associated with elevated IOP, ocular discomfort, blurred vision and stromal keratitis. The reason it may go undetected is that clinically it resembles diffuse lamellar keratitis, which is far more common after refractive surgery. This is problematic, because the treatment For DLK is steroids, but steroids actually cause PISK; to treat PISK, steroids need to be stopped. So if the surgeon mistakes PISK for DLK, he'll think he's doing the patient a favor by keeping him on steroids, when in fact the steroid response will keep getting worse and worse. In one case report, a patient kept on topical corticosteroid drops for nine weeks in an attempt to treat presumed DLK suffered optic nerve atrophy and associated visual field loss before the error was discovered and corrected.
Probably the easiest way to distinguish PISK from DLK is the timing of presentation. DLK tends to present early on following surgery; PISK usually presents beyond the fourth postoperative week. If you determine that the elevated IOP is the result of PISK, stop steroid treatment immediately.
Managing Glaucoma Postop
If a patient needs treatment for glaucoma or ocular hypertension, previous refractive surgery will have an impact on our ability to diagnose and monitor the disease. In particular, the impact of corneal alteration on IOP measurement can be profound; a Goldmann tonometer may measure as low as 14 mmHg after refractive surgery, when the actual IOP is 30 mmHg. Thus, if you know a patient has had prior refractive surgery, special steps should be taken to ensure that your treatment is based on accurate data.
• Gather as much pre-refractive- surgery data as possible. This will help determine how the eye was altered by the surgery.
• Use alternate instruments to measure IOP. As noted above, other devices may do a much better job of accurately measuring IOP under these conditions. A glaucoma specialist may own a Dynamic Contour Tonometer or Ocular Response Analyzer, but a comprehensive ophthalmologist probably will not. However, as the number of glaucoma patients with previous refractive surgery increases, anyone treating glaucoma should consider investing in one of these instruments. If that's not feasible, it may be worth referring the patient to a glaucoma specialist to ensure that treatment is being based on the most accurate IOP readings.
If you have the capability of measuring the IOP in more than one way, that may also help to give you an idea of how much the IOP reading was altered by the refractive surgery. However, for ongoing measurement, use the same instrument every time.
• Monitor non-IOP parameters extra carefully. This is always important in a glaucoma patient or suspect, but it's especially important when IOP measurements may be suspect because of refractive surgery. If the optic nerve looks suspicious or a disc hemorrhage is present, treatment is probably needed. In addition, we now have multiple options for scanning the optic nerve and nerve fiber layer, and most studies of various imaging modalities have reported no changes in the retinal nerve fiber layer thickness after refractive surgery.8,9 (Caution in interpretation is required when using scanning laser polarimetry without the variable corneal compensation.) Attention should also be paid to earlier detection of functional loss using new technologies such as shortwave automated perimetry (SWAP) or frequency doubling technology (FDT), which can detect visual field loss much sooner than white-on-white automated perimetry by targeting a different population of ganglion cells.
Again, a glaucoma specialist will automatically monitor these factors closely, but a comprehensive ophthalmologist may be less attuned to them. If following these factors in great detail is not practical in your clinic, the best alternative is probably to invest in one of the non-contact tonometers mentioned earlier. That way you can at least be sure your IOP measurements are not being unduly influenced by the prior refractive surgery. And remember to pay close attention to your clinical exam of the optic nerve and nerve fiber layer.
Dr. Salim is assistant professor of ophthalmology at the University of Tennessee Health Science Center at Memphis. She has no financial interest in any of the products mentioned.
1. Mitchell P, Hourihan F, Sandbach J, et al. The relationship between glaucoma and myopia: The Blue Mountains Eye Study. Ophthalmology 1999;106:2010-5.
2. Armaly MF, Becker B. Intraocular pressure response to topical corticosteroids. Fed Proc 1965;6:1274-8.
3. Paciuc M, Velasco CF, Naranjo R. Acute angleclosure glaucoma after hyperopic laser in situ keratomileusis. J Cataract Refract Surg 2000;4:620-3.
4. Garzozi HJ, Chung HS, Lang Y, et al. Intraocular pressure and photorefractive keratectomy: A comparison of three different tonometers. Cornea 2001;20:33-6.
5. Lee AG, Kohnen T, Ebner R, et al. Optic neuropathy associated with laser in situ keratomileusis. J Cataract Refract Surg 2000;26:1581-4.
6. Hamilton DR, Manche EE, Rich LF, et al. Steroidinduced glaucoma after laser in situ keratomileusis associated with interface fluid. Ophthalmology 2002;109:659-665.
7. Davidson RS, Brandt JD, Mannis MJ. Intraocular pressure-induced interlamellar keratitis after LASIK surgery. J Glaucoma 2003;12:1:23-6.
8. Zangwill LM, Abunto T, Bowd C, Angeles R, et al. Scanning laser polarimetry retinal nerve fiber layer thickness measurements after LASIK. Ophthalmology 2005;112: 200-207.
9. Whitson J, McCully JP, et al. Effect of laser in situ keratomileusis on optic nerve head topography and retinal nerve fiber layer thickness. J Cataract Refract Surg;12:2302-05.