AcrySof Toric's Background
To get an idea of the data surgeons will base their treatment decisions on, here's a review of how the AcrySof Toric performed in its FDA clinical trial. In the study, 494 subjects received a lens in their first operative eye. Of these, 250 received an AcrySof SA60AT to act as controls, and 244 received a toric AcrySof.
There are three models currently approved, each with a different level of correction: the T3 (1.5 D cylinder power; 1.03 D cylinder correction at the corneal plane); T4 (2.25 D cylinder power; 1.55 D cylinder correction at the corneal plane); and T5 (3 D cylinder power; 2.06 D cylinder correction at the corneal plane). In the study, 123 patients received a T3, 67 got a T4 and 54 received T5s.
The AcrySof toric IOL could give surgeons more flexibility in dealing with pre-existing astigmatism.

Each of the models was three times more likely than a conventional AcrySof control lens to achieve residual cylinder of 0.5 D or less. In terms of uncorrected acuity, 38 percent of the toric patients saw 20/20 or better, compared to 19 percent of the controls, and 94 percent saw at least 20/40 vs. 77 percent of the control eyes.
With the T3 aimed at correcting less than 1.5 D of astigmatism, there was a 62-percent mean change in cylinder from baseline levels (SD: 38 percent). For an intended cylindrical correction of between 1.51 D and 2 D using the T4, there was a 55-percent average change (SD: 33 percent); and for intended cylindrical corrections over 2 D for which the T5 was used, there was a mean cylinder change of 68 percent (SD: 25 percent).
The other aspect of toric lenses that surgeons are concerned about is rotational stability, since the efficacy of the lens decreases the farther it rotates off of the correct axis. In the study, immediately postop, the mean difference between the intended axis and the achieved was 0.4 ±1.4 degrees. This figure defines how easy or hard it is for the surgeon to get the axis correct. Over the first four to six months postop, 81 percent rotated by 5 degrees or less, and 97 percent rotated by 10 degrees or less.
Astigmatism Protocols
Surgeons say they would probably make a place for the toric lens in their approach to cataract patients, with some caveats.
"If I have a patient in the range of 0.5 D to 2 D of cylinder, and probably 30 to 40 percent of patients fall in this range, in the past I've used limbal relaxing incisions for him," says Minneapolis surgeon David Hardten. "Though, by LRI I mean essentially a 9-mm astigmatic keratotomy, rather than an 11-mm at-the-limbus relaxing incision. I choose this AK because I think it's still pretty safe, you don't have to do as long an arc, and most of the time you get pretty close to the astigmatic effect you want, usually up to 1.5 D or so." He says for patients with 0.5 D or less of cylinder, he doesn't do anything other than make sure he doesn't increase the astigmatism with his cataract incision. "Most of the 2.5- to 3-mm incisions don't do much to induce, worsen or control astigmatism," says Dr. Hardten.
Dr. Hardten thinks the toric lens will be helpful for patients with higher levels of astigmatism. "I think they will be useful for patients with over 1.5 D or 2 D of cylinder in whom LRIs really haven't been as effective," he says. "Patients in that range really want exquisite control of astigmatism and might be the ones who would need secondary laser vision correction to achieve that." He says if a patient has 2.5 D of cylinder, for example, he'd use LRIs to control as much astigmatism as he could at the time of the initial surgery, and, in the relatively rare instance that the patient was still dissatisfied postop, he'd perform a PRK.
Davenport, Iowa, surgeon Lisa Arbisser has worked with the new lens, and, though she feels confident with her corneal incisions, she'd probably prefer to use a lens. Like Dr. Hardten, she also uses a variation of AK rather than strict LRIs.
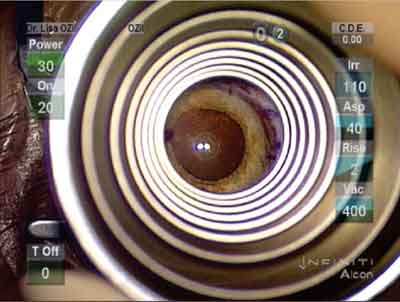
Iowa surgeon Lisa Arbisser uses a Maloney Keratoscope to assess the effect of her relaxing incision.
Lisa Arbisser, MD
"I tell patients who have 2 D of cylinder or less that I can give them a 98-percent chance that, with one surgery, they'll be able to pass the drivers test," says Dr. Arbisser. "I don't promise people crisp, 20/20 vision, because it's really hard to get that with AK." She says though patients can still see very well despite some residual astigmatism, "I'm sure we're making a slightly irregular shape to the cornea [with incisions]. I think the more we can handle using lens-based methods, the healthier it is for these patients."
For patients with higher levels of astigmatism, such as 4 D, since the AcrySof approval doesn't reach that far, Dr. Arbisser says it's possible to combine AK with a toric lens, but possibly not at the same sitting. "I don't think we're accurate enough with these treatments to do that."
Nashville, Tenn., surgeon Jeffrey Horn took part in the Alcon FDA trial of the lens, and says he would probably not use LRIs as often if and when the lens becomes available for wider use. Dr. Horn serves on Alcon's speakers bureau, and receives grants for research from the company.
"If I had a patient that had enough astigmatism to warrant getting the implant, I'd advocate implanting the lens over LRIs, which are potentially unpredictable due to factors such as patient healing," says Dr. Horn. If faced with a patient whose astigmatism is near the upper end of what the most powerful model of the lens, the T5, could correct, he'd use a T5 to get as much as he could, then place corneal incisions later.
A theoretical problem is that, if a toric IOL doesn't correct all of a patient's astigmatism, it could make for a more difficult wavefront-based procedure afterward.
"If a patient's cylinder is over 3 D, that puts me in that range where I'm a little nervous that I'm going to take away some of the things that, postop, let me get good results with astigmatism control, such as laser vision correction," says Dr. Hardten. "For example, if I still have 2.5 D of mixed astigmatism because I've got a toric implant in the eye, that might complicate my wavefront acquisition and it might reduce the optical zone I'm able to capture. Also, the topography will no longer match the refractive astigmatism, because you have a toric lens inside the eye, and you can't look at the topography to help guide your correction."
Dr. Horn says there probably isn't data on such treatments yet, since no "touch-ups" were allowed in the trial, and the lens has only been available since around March of this year. However, he notes that in the trial the residual astigmatism was usually a small amount, and often not enough to warrant a second procedure. He agrees though, that wavefront sensing might not be the best way to proceed in a patient with a toric implant.
"I don't know if I'd necessarily do wavefront-guided laser vision correction on these patients," says Dr. Horn. "Putting implants in these eyes causes the wavefront measurement to be potentially inaccurate."






