Cataract surgery may be the most frequently performed surgery in the world, but it’s still a complex procedure that—like the eyes cataract surgeons are operating on—is a little different every time. Given the vast number of patients presenting for surgery, surgeons are certain to encounter challenges.
Here, in the first of a two-part series, surgeons who’ve performed thousands of cataract surgeries share their advice regarding what to do when facing obstacles—expected or unexpected—during cataract surgery. Challenges discussed this month include uncooperative pupils; poor visualization through the cornea; lack of a red reflex; and weak or missing zonular fibers.
Visualization: Problematic Pupil
One of the first challenges a cataract surgeon may encounter is a small pupil, despite preoperative dilating drops. Options for addressing this include stretching the pupil with viscoelastic; stretching the iris manually with a tool; using iris hooks to hold the iris back during the surgery; and using a ring to keep the pupil enlarged.
Richard Mackool, MD, medical director at The Mackool Eye Institute and Laser Center in Astoria, New York, and senior attending surgeon at the Mt. Sinai New York Eye and Ear Infirmary and New York University Medical Center, says that when dilation becomes an issue, the surgeon should first ask if there’s a chemical way to dilate it. “Don’t be in a hurry to use mechanical stretching without trying other steps first,” he says.
Dr. Mackool notes that in many eyes, especially those with a somewhat floppy iris, you may be able to get the pupil to enlarge just by injecting viscoelastic. “I normally use a dispersive viscoelastic for this because it will retain its position against the sphincter of the iris during the procedure much better than a cohesive viscoelastic,” he says. “In many cases, that’s all that’s needed. However, in some eyes you may also want to inject an adrenergic drug such as epinephrine or phenylephrine. If that’s the case, you need to inject that drug before you inject the OVD. If you inject the OVD first, it will prevent the drug from reaching the iris.
“During the case, avoid aspirating the OVD from the region of the pupillary margin,” he adds. “And, don’t hesitate to re-inject OVD during the case if the pupil starts to come down.”
In terms of mechanical devices for managing the iris, Dr. Mackool notes that some devices aren’t designed to be left in the eye. “My favorite in this category is the two-pronged Beehler pupil dilator [Moria Surgical],” he says. “It stretches the pupil, and in the vast majority of cases, that’s adequate to resolve the problem.”
Elizabeth Yeu, MD, currently in private practice at Virginia Eye Consultants in Norfolk, Virginia, an assistant professor in the department of ophthalmology at Eastern Virginia Medical School, and medical director of the Virginia Surgery Center, notes that to some extent, choosing to work with a pupil between 4 and 6 mm is a matter of the surgeon’s skill set and comfort level. “For me, getting Omidria [keterolac and 1.5% phenylephrine] onboard in that situation has been a huge advantage,” she says. “It allows me to avoid having to do a physical manipulation of the pupil to enlarge it with a Beehler device, iris hooks or a Malyugin Ring.
“However, if the pupil is very small—say under 4 mm—and it’s not responding to the initial dilating drops, it’s not going to dilate because of Omidria or any other drug,” she continues. “In that situation, mechanical manipulation becomes a necessity. Which type of device you should use depends partly on factors such as the presence of posterior synechiae and partly on what the surgeon is comfortable with. If the patient hasn’t been using Flomax [tamsulosin], my go-to is using the Beehler dilator.”
 |
Dr. Mackool says the third way to manage a small pupil is with iris retractors. “These are typically less expensive than the rings, but are a bit more time-consuming to put in,” he notes. “They require a little more dexterity, and you have to adjust the tension on them. If you use four of them, you have to make four tiny punctures in the cornea. They have no effect on the outcome of the procedure, but to save time, many surgeons prefer to simply use a ring.”
Nick Mamalis, MD, ASCRS president, professor of ophthalmology, and director of ocular pathology and co-director of the Intermountain Ocular Research Center, part of the Moran Eye Center at the University of Utah in Salt Lake City, says that if there are no iris abnormalities or zonule issues, he finds pupil rings easier to use than iris hooks. “I have the most experience with the Malyugin Ring,” he says. “You insert its eyelet rings onto the iris and it gives you a nice diamond-shaped dilation that doesn’t disturb the iris sphincter. It usually doesn’t cause problems with bleeding, or any pupil irregularity afterward. However, I may use iris hooks to improve visualization if there are zonular insufficiencies—especially in focal areas. If you want to pull the iris back to improve visualization at one particular point, iris hooks are invaluable.”
Daniel H. Chang, MD, a partner at Empire Eye and Laser Center in Bakersfield, California, prefers using a ring to manually stretching the pupil. “The nice thing about the Malyugin Ring is that it holds the iris at eight points,” he says. “Stretching it manually brings a greater possibility of focal iris sphincter damage and distortion of the pupil shape, as well as the possibility of causing bleeding. The ring also stretches the pupil, of course, but the force is applied more evenly. The only case in which I had a slightly irregular pupil after using a ring was in a patient who had some preexisting scarring of the iris.
“The ring can also function as a good guide to help me center and size my rhexis,” he adds. “Later, I remove it before I take the viscoelastic out.”
Strategies for Pupil Dilation
Surgeons offer this advice when dealing with a small pupil:
• Don’t use manual stretching if the patient has been using Flomax. “Flomax can cause the iris tissue to lose tonicity completely,” notes Dr. Yeu. “In that situation, stretching it manually with iris hooks or the Beehler tool is the worst thing you can do because the iris can cheese-wire right through. Using a Malyugin ring or similar device that circumferentially holds it open is a great way to manage that pupil.”
• If the iris is floppy, use a lower-flow fluidics setting with continuous irrigation. “When the pupil is small and the iris may be floppy, the latter will have a tendency to come out of your wounds because that’s the path of least resistance,” says Dr. Yeu. “In that situation, use a lower-flow setting with continuous irrigation to minimize bouncing of the anterior chamber and lower the risk of extrusion.”
• In Flomax patients, dilating chemicals in the irrigation solution may prevent a mid-surgery pupil constriction. “Sometimes if the patient is on an alpha antagonist such as Flomax, the pupil will stay dilated initially, but during the course of the procedure it will constrict and the iris will become floppy,” Dr. Mamalis explains. “So, you want to plan ahead to avoid dilation problems in these patients. I put Omidria into the irrigating solution to keep the pupil from coming down during the surgery.”
• If a patient isn’t dilating well, try intracameral lidocaine. Dr. Chang says he uses intracameral 1% preservative-free lidocaine when a patient doesn’t dilate well. “If the pupil is 5 mm or smaller, I also place a Malyugin Ring,” he says. “I don’t use intracameral anesthesia on routine cases, but I will on patients with borderline pupils, for two reasons. One, it can help with dilation. Two, if I’m going to manipulate the iris, the supplemental anesthesia inside the eye will help to maintain patient comfort.
“If it’s a 6-mm pupil, or if the patient is on tamsulosin or a similar alpha-blocking medication, I try to assess the iris rigidity while I inject the lidocaine and viscoelastic,” he explains. “Once you open the capsulorhexis, you have to be very careful about placing iris retractors, so I watch the iris as I inject the lidocaine and viscoelastic. If I see it flapping around as I’m injecting either, I’m more likely to insert a Malyugin Ring.”
• Avoid touching the iris. “Once you touch the iris, the pupil will want to come down even further,” Dr. Yeu notes.
• Be on the lookout for high posterior pressure. “This is relevant because when there’s a lot of pressure posteriorly and the bag complex comes forward, the pupil usually comes down as well,” Dr. Yeu explains. “So, if you have a firm eye, a shallow chamber, a small pupil and the iris wants to come out, posterior pressure may be the problem. This can happen in small eyes even without the effusion, because the scleral wall is thicker and the eye has less volume. Often, you’ll notice the signs of this as soon as you enter the eye and put in viscoelastic. For smaller eyes, applying pressure to soften the eye with a Honan balloon or reducing vitreous pressure with IV mannitol can be helpful.
“If that’s the case, there may be a choroidal effusion or an anterior rotation of the ciliary body,” she adds. “In that situation you have to do what you can to mitigate the positive posterior pressure. Deepen very slowly with a heavy viscoelastic device, and stop if iris tissue is moving towards prolapsing out of the wound. If possible, you may need to do a tap of the vitreous cavity to release some of that pressure.”
Visualization: The Cornea
“Whenever you encounter a problem with visualization, the first thing you absolutely have to do is figure out the cause of the problem,” Dr.
Mackool says. “Never, ever proceed until you’ve answered that question.”
Dr. Mackool notes that a number of issues can interfere with your ability to see into the eye clearly. “First, remember that it could be something as simple as the lens at the bottom of your microscope needing to be cleaned,” he says. “Sometimes saline will spray up onto it, maybe from an earlier case; the saline dries, leaving a salt deposit on the lens. Or, the eyepieces could be smudged or have condensation on them. Then, make sure there are no mucoid deposits on the cornea. Irrigate the surface to make sure it’s clear of particulate matter.”
Dr. Mackool points out that a dry, edematous or irregular cornea can interfere with visualization. “The technician may have taped the lids open and the corneal epithelium simply dried out,” he says. “Generally, it’s good to keep the cornea very moist during the procedure. If I know there’s an issue with corneal dryness—whether it was allowed to dry out, or because of a pre-existing issue such as epithelial dystrophy—I coat the surface of the eye with an OVD.
“The best OVD for this purpose is hydroxymethyl cellulose, otherwise known as OcuCoat,” he continues. “It has the perfect molecular weight to coat the surface very well and give you really good visibility. Sometimes it even helps with preexisting corneal irregularities—including some keratoconic eyes that have deformities. I don’t use it intraocularly, but it’s great on the surface of the cornea for these situations.
“If you need to deturgesce an edematous cornea to improve visualization, you should do two things,” he explains. “First, put a dispersive viscoelastic in the anterior chamber to coat the endothelium, so aqueous or BSS can’t pass into the cornea during the case. Second, put topical glycerin on the surface of the cornea. It’s an osmotic dehydrating agent, and within 30 to 60 seconds it will remove the fluid from the epithelium. There will still be fluid in the stroma, but that tends to have less impact on vision.
“If you need to dry out the stroma as well, keep adding glycerin for about 10 minutes,” he adds. “The fluid in the stroma will gradually move toward
the epithelium and be removed by the glycerin. With patience, even very ede-
matous corneas can get pretty clear.”
Dr. Mamalis says that if he has a patient with significant epithelial edema, he may try to deturgesce the cornea using hyperosmolar drops. “High-molecular-weight Dextran will sometimes help,” he notes. “Glycerin does the same thing. But if you can’t get a good view in spite of that, as a last-ditch option you may have to scrape off the epithelium. That’s a drastic step I try to avoid, because then the patient has to wear a bandage contact lens for several days while the epithelium heals.”
Dr. Yeu says that if she’s faced with corneal edema when coupling cataract surgery with a procedure such as an endothelial keratoplasty, she’ll proceed with the surgery until she has to denude the epithelium in order to see clearly enough to continue. “Denuding the epithelium via a superficial keratectomy buys you another 10-to-15 minute window of greater clarity,” she notes.
 |
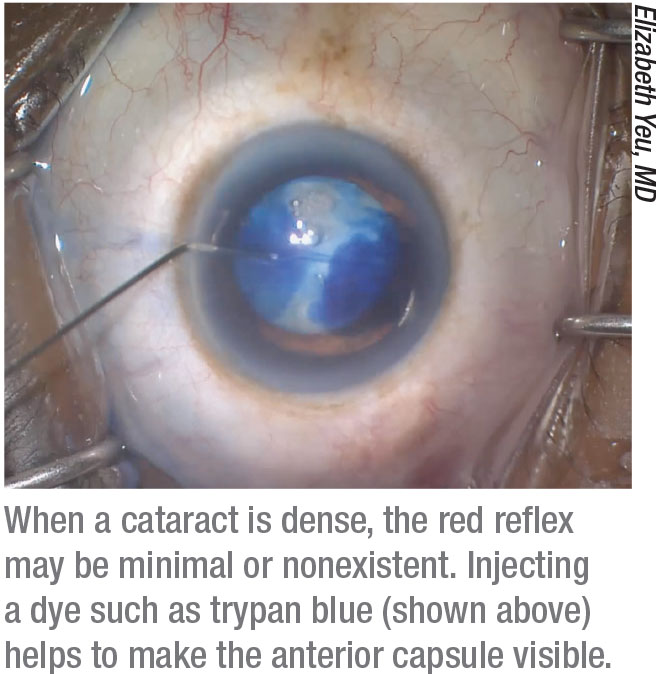
Visualization: No Red Reflex
In some patients, a cloudy cataract will minimize or eliminate the red reflex that ordinarily helps the surgeon see the anterior capsule. Dr. Yeu says if there’s poor visualization through the cornea or a poor red reflex, she uses VisionBlue (trypan blue, DORC) to stain the capsule. “I generally put it into the eye without air, count to 10, and then wash it out,” she says.
She notes that pupil size can be an issue when using a capsule stain. “The trypan blue is only going to stain what’s actually visible on the anterior capsule,” she points out. “So, with a smaller pupil I’ll do what I can to stretch the pupil under cohesive viscoelastic to get as much visualization of the anterior capsule as possible before staining it. You want to be sure you get the stain across all of the anterior capsule that you need to see so you’ll have enough visible surface area to perform your capsulorhexis.”
Dr. Yeu notes that when the red reflex is missing, the surgeon needs to proceed much more cautiously. “Use continuous irrigation with a lower flow rate,” she advises. “Be aware that it may be more difficult to see the posterior capsule, and there could be positive posterior pressure as well.
“In this situation I may use a Koch spatula, held with my nondominant hand, to hold the capsule back while disassembling the nucleus,” she adds. “In fact, I always use a Koch spatula with my last quadrant of lens when performing cataract surgery, but it’s especially important when you lose your red reflex. Meanwhile, fill the bag with dispersive viscoelastic, move slowly, and see if you can find any clues to the contour of the bag—especially when you only have a few pieces of nucleus left to remove.”
Weak or Missing Zonular Fibers
This is a problem that can often—though not always—be detected preoperatively. “Knowing the condition of the zonules beforehand lets you be prepared for what you’ll encounter during surgery,” notes Dr. Yeu. “For example, if your patient has a dislocated lens, you want to know how dislocated it is, in terms of clock hours. If you notice a generalized shimmering of the lens, you might be dealing with a pseudoexfoliation patient.”
Dr. Yeu adds that if the crystalline lens is grossly dislocated, you should lay the patient in a supine position preoperatively. “You want to make sure that the lens doesn’t have a tendency to fall back into the vitreous cavity to a point at which you can’t access it when you’re in the OR,” she says. “This is especially important if the patient has gross zonulopathy, such as four to six clock hours of missing zonules. If you can’t visualize the lens when the patient is lying supine, a combined case with (or a referral to) a retinal surgeon will be the safest option for an anterior segment surgeon.”
Dr. Yeu admits that you can’t always detect zonular problems preoperatively. “If you find, for example, that you’re struggling to create a large enough rhexis, and/or the capsule wrinkles during the capsulorhexis, you may not be getting the usual counter-pressure from the zonules,” she says.
Dr. Chang agrees, noting that a manual capsulorhexis can help to identify locations where the zonules may be focally weak. “Be cautious, because in areas where zonules are weak the lens has a tendency to pull centrally during the capsulorhexis,” he says. “When you release, it moves back and you’ll find that you’re farther toward the periphery of the lens than you thought.”
Tools for Managing Zonules
Several options can help when weak or missing zonular fibers are present:
• A femtosecond laser capsul-otomy. Dr. Yeu points out that if zonular weakness is affecting your ability to make the capsulorhexis, a femtosecond laser capsulotomy could be ideal. “If the patient has decent dilation,” she says, “you can center the laser on the capsule and get exactly what you need without involving the zonules.”
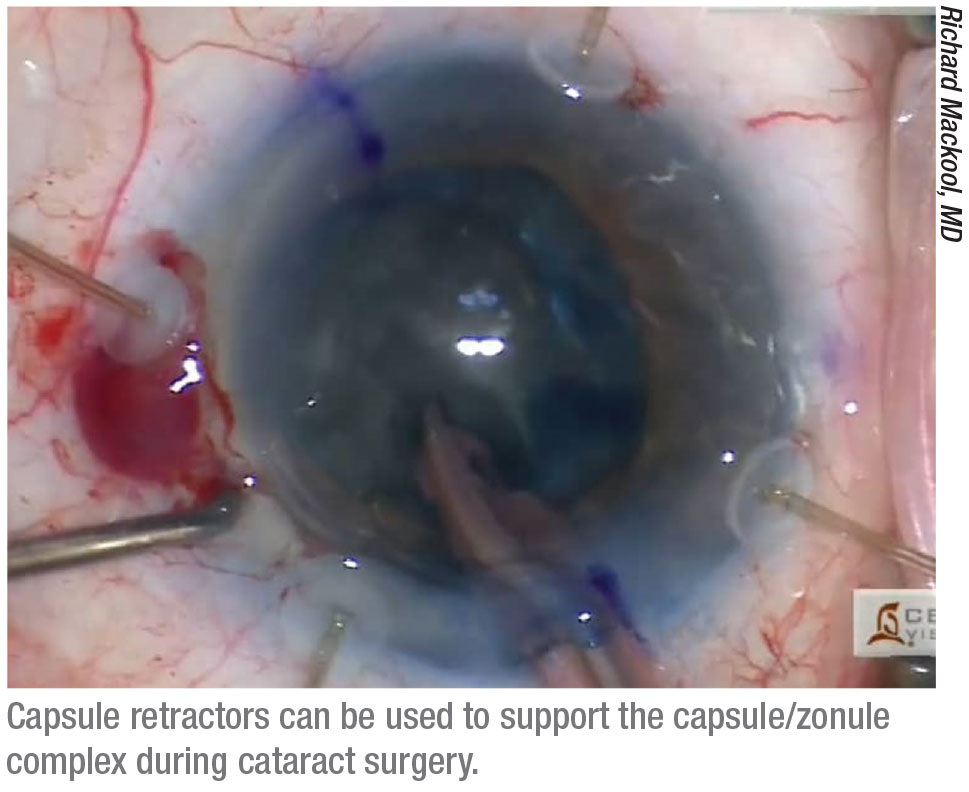
• Capsule retractors. “Capsule retractors hook over the edge of the capsulotomy,” explains Dr. Mackool, who invented the first capsule retractors about 20 years ago. “These are fundamentally different from iris retractors, which are short and not designed to stabilize a lens capsule.”
Dr. Mackool says a common error is holding off using capsule retractors, thinking you might be able to get by without them. “That’s not a good idea, because they can save you from a world of trouble,” he notes. “The first time you think you might need them, stop and put them in. They can dramatically reduce the likelihood of complications. I’ve never regretted putting in capsule retractors, but I have regretted not putting them in.”
Dr. Mackool offers one important tip when using capsule retractors: Don’t pull them tight to retract the capsulorhexis. “That’s not how they help,” he explains. “The terminal part of the retractor going out into the capsular fornix provides support. Just place the retractors so they approximate the edge of the capsulorhexis margin. In areas where there are no zonular fibers, place one about every 45 degrees; in areas where the zonule is lax or weak, put one every 90 degrees.
“If you’re not used to inserting them, it will take you five minutes, but once you’re used to putting them in, it takes two minutes,” he adds. “Be especially careful when using them after a femtosecond laser capsulorhexis, because it might not be as resistant to tearing as a manual capsulorhexis.”
• A capsular tension ring. Surgeons point out that it’s important to know when it makes sense to use a CTR. “A capsular tension ring will keep the capsule expanded, but it doesn’t reduce zonular stress during the procedure,” says Dr. Mackool. “In contrast, capsule retractors act as an artificial zonule. They take the stress off the remaining zonular fibers.”
“If you’re having difficulty because the lens is moving, using a capsular tension device can be helpful,” notes Dr. Yeu. “However, I put it in as late as possible because once the ring is in, it makes it more difficult to do cortical removal. If you can wait until the cortex is completely removed, that will make life easier. But if you have to insert it early on—which sometimes is unavoidable—then be aware that you’ll have to do extra-slow, careful viscodissection to loosen up the remaining cortical fibers.”
Dr. Chang points out that sometimes when the zonules are weak, the lens has been bolstering things in place. “If that’s the situation, you may take out the lens and discover that the bag is collapsing in one area,” he says. “At that point, placing a capsular tension ring can be helpful.”
• An appropriate IOL. “If you have just a little bit of zonulopathy, say one or two clock hours, inserting a three-piece IOL with the haptics aligned in the area of the slightly loose zonules will help to provide some tension at that location,” notes Dr. Yeu. “If the eye has about three clock hours of missing zonules, or a little zonulopathy that’s generalized, as you might find in a pseudoexfoliation patient, a standard capsular tension ring can be a good solution.”
• Segments that can be sewn in place to support the capsule. “Once you have more than three clock hours of missing or weak zonules, or the lens is grossly dislocated, you’ll have to sew in either a segment or a ring, or a combination of multiple segments,” says Dr. Yeu. “How you proceed depends on your skill set and what the ultimate goal of your surgery is.”
 |
Dr. Mamalis says that the tool that makes the most sense depends mostly on whether the zonular disruption is focal or diffuse. “Patients who’ve had a trauma sometimes have disruption of the zonules in just one quadrant,” he points out. “In those patients, you may want to put a capsular hook or two in that area to protect the zonules while you do the phaco. If the area of disruption is three clock hours or less, you can proceed to put a capsular tension ring into the bag, followed by the implant, and you don’t have to do anything further.
“Some patients, such as those with Marfan syndrome or severe exfoliation syndrome, can have zonular weakness all the way around,” he continues. “In that case, I think it’s very helpful to use capsular hooks to support the lens capsule while you’re removing the cataract. After that, a capsular tension ring may not be sufficient to support the capsule with the lens in it, so you may want to consider using a device that can be placed into the capsular bag and sutured to the ciliary sulcus, such as a Cionni ring or an Ahmed segment.”
More Zonule Strategies
Surgeons offer these additional tips:
• If you can see the edge of the capsular bag equator, use viscoelastic to prevent vitreous prolapse. “In this situation you have several missing zonules,” Dr. Yeu points out. “That space is going to allow communication to the vitreous cavity. So it’s extremely important that you tamponade that space with dispersive viscoelastic to prevent vitreous prolapse.”
• Remember that weak zonules can lead to nuclear fragments migrating posteriorly. “When there are areas of zonular compromise, it’s crucial to make sure you get all of the cataract out,” says Dr. Chang. “Be sure you don’t still have a lens fragment behind the posterior capsule. If you’re not sure, dilate early postoperatively or send the patient to retina.”
• Don’t hesitate to refer. Dr. Chang believes there’s no shame in referring a very complex case. “If a patient is missing significant zonules or if the lens is significantly dislocated, I refer those cases either to a colleague who specializes in managing that type of case or to a retina specialist,” he says. “They can take the lens out from the back.”
Dr. Yeu agrees. “For example, you might encounter a patient with zonulopathy and a very dense lens,” she says. “That’s going to be a very tough case, because disassembling that lens will require a lot of manipulation, making it likely that you’ll cause more zonulopathy intraoperatively. You have to decide if this is a case that you want to do yourself. You always have the option of sending the case to someone else.” REVIEW
Dr. Chang is a consultant for Zeiss. Dr. Yeu is a consultant for Omeros. Drs. Mackool and Mamalis have no financial ties to any product discussed.
Next month in Part 2: Managing anterior and posterior capsule tears, problems resulting from the patient coughing, bleeding inside the eye, wound burns and removing a very dense cataract.