Presentation
An 86-year-old Caucasian female with a Type 1 Boston Keratoprosthesis (KPro) in the right eye presented for routine postoperative follow-up with her cornea specialist 16 months after transplantation. During the first six months postoperatively, vision in the right eye remained ‘hand motion’ at worst to ‘count fingers’ at best, limited by glaucomatous optic nerve damage. However, the patient complained of persistent ‘light perception’ vision from postoperative month seven onward despite a laser membranectomy for a dense retroprosthetic membrane (RPM). No pain or increased redness was reported.
Medical History
Past ocular history included two failed traditional penetrating keratoplasties on the right eye in the setting of herpes zoster ophthalmicus, a neurotrophic ulcer and necrotizing herpetic stromal keratitis. Additional ocular history included primary open angle glaucoma, Fuchs’ dystrophy, cataract extraction and lens implantation in both eyes and a Descemet’s stripping endothelial keratoplasty on the left eye. Prior to the KPro implantation, the contralateral left eye had developed both early DSEK graft failure and visually significant scarring secondary to bacterial keratitis.
At the time of KPro implantation, visual acuities were ‘light perception’ in the right eye and ‘count fingers’ in the left eye. There was an initial small increase in visual acuity during the first six postoperative months as noted above. However, visual prognosis was limited by worsening glaucoma. By postoperative month seven, vision was only ‘light perception’ and no improvement was seen after a laser membranectomy. Throughout the postoperative period, the patient wore a soft contact lens and remained on topical ciprofloxacin, vancomycin and a steroid with good reported compliance.
Ocular medications at presentation: vancomycin 2.5% gtt b.i.d. OD; ciprofloxacin 0.3% gtt b.i.d. OD; prednisolone sodium phosphate 1% gtt b.i.d. OU; brimonidine 2%/timolol 0.5% gtt b.i.d. OU; ciprofloxacin 0.3% ointment qHS OS; bacitracin ointment qHS OS; acyclovir 400 mg b.i.d. by mouth.
Other past medical history was notable for breast cancer, hypercholesterolemia and a hiatal hernia. Systemic home meds included omeprazole, simvastatin and mirtazapine. Family and social history were noncontributory.
Examination
 |
Ocular examination demonstrated corrected visual acuities of ‘light perception’ OD and 20/200 OS with pinhole correction to 20/160. Confrontation visual fields were unable to be completed on the right and intact on the left. Intraocular pressure was estimated at 10 mmHg tactile OD and 14 mmHg tactile OS. Motility was grossly full. Pupillary exam demonstrated a known, noted right-sided 2+ rAPD, thought to be due to glaucoma.
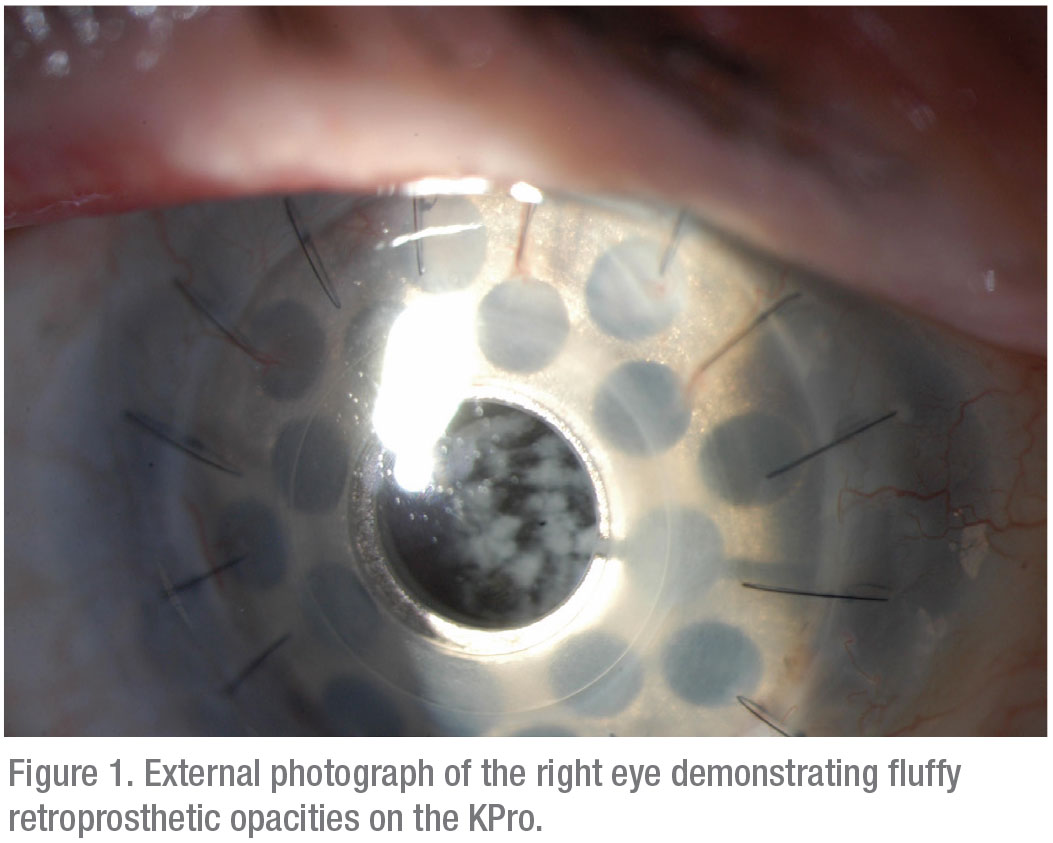
Anterior slit lamp examination of the right eye was most notable for several small white retroprosthetic opacities (Figure 1). The KPro/PK complex was in good position as was a soft contact lens. The rest of the exam on the right demonstrated mild conjunctival injection and two well-covered glaucoma drainage devices. Slit lamp exam also suggested the development of a fluffy vitreous opacity. Posterior exam on the right revealed 3+ optic nerve pallor with severe cupping and a grossly flat retina.
Anterior slit lamp exam on the left was notable for a 3+ superonasal corneal scar encroaching on the visual axis. The rest of the corneal exam revealed a well-positioned DSEK button and trace stromal edema. The conjunctiva was white and quiet, the AC was deep and quiet, iris was normal appearing and the PCIOL was well-centered. Posterior exam on the left revealed a 20/70 view to the posterior segment, mild optic nerve pallor with severe cupping and a grossly flat retina.
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



