A 45-year-old Caucasian male with past medical history significant for chronic sinusitis presented to the Wills Eye emergency room with a two-week history of left-sided facial pain and swelling, presumed to be due to an acute exacerbation of sinusitis. The patient first noted left ear pain as well as left upper and lower eyelid swelling and redness about two weeks earlier. He recalled having a moderate, transient left-sided headache at the time of symptom onset, which had not recurred. There was no history of trauma. A full course of oral azithromycin with a rapid oral steroid taper provided no relief. He was also prescribed tobramycin/dexamethasone (0.3%/0.1%) ophthalmic suspension three times daily to the left eye for one week, with no relief. He reported no blurry vision, eye pain or double vision.
Medical History
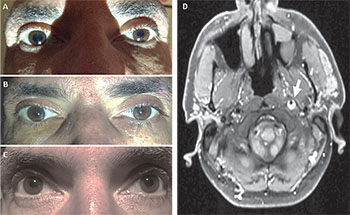 |
| Figure 1. View of the patient’s eyes (A) immediately after ambient light was decreased and (B) after ambient light was increased once again. (C) Is post apraclonidine testing OU. An axial T1 MR image (D) revealed a hyperintense, crescent-shaped thrombus (arrow) in the distal cervical segment of the left internal carotid artery (ICA) consistent with an ICA dissection. |
The patient was healthy except for a history of multiple previous sinus infections spanning several years, which had all been successfully treated with oral antibiotics. There was no history of tobacco use, diabetes, hypertension or malignancy. He had no history of intravenous drug use and drank only socially.
Examination
The patient’s vital signs on arrival were significant for a regular pulse of 72 and a blood pressure of 166/112. He was afebrile. A brief systemic physical exam was unremarkable.
Ophthalmologic examination revealed a visual acuity of 20/40 in the right eye (OD) and 20/25+2 in the left eye (OS). Both pupils were round and reactive, with no relative afferent pupillary defect. In ambient lighting, the patient’s pupils measured 3 mm OD and 2 mm OS; in the dark, the patient’s pupils were 5 mm OD and 2.5 mm OS. Extraocular movements and confrontation visual fields were grossly full in both eyes. External examination revealed an upper eyelid margin to corneal reflex distance of 3.0 mm OD and 1.5 mm OS. The lower eyelid positions were symmetric. There was no evidence of eyelid edema, erythema or tenderness. There was no palpable lymphadenopathy. On slit-lamp exam, the anterior segment exam was unremarkable. Intraocular pressure was 18 mmHg in both eyes. Dilated funduscopic examination was deferred until further testing was completed.
Please click this link for diagnosis, workup, treatment and discussion.



