Workup, Diagnosis and Treatment
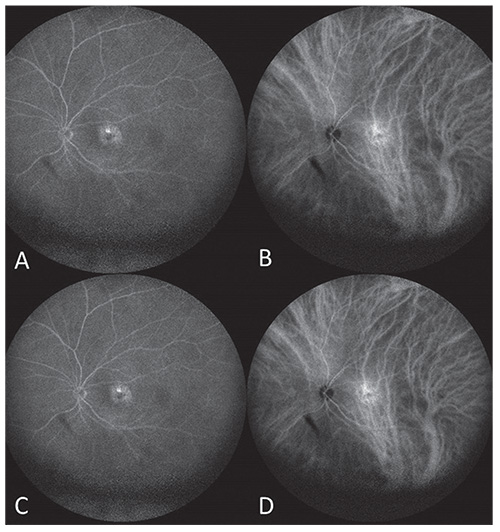 |
| Figure 3. (A) Fluorescein angiography and (B) indocyanine green angiography at 1 minute, 9 seconds after injection showing a slight macular window defect with associated hypercyanescence. (C,D) At 5 minutes, 11 seconds after injection, the hyperfluorescence was stable. There was no evidence of choroidal neovascular membrane. The classic choroidal hemangioma hypercyanescence at one minute with late washout was absent. |
Ultrasonography OS revealed a slightly elevated, echodense, dome-shaped mass (Figure 2). Fluorescein angiography demonstrated normal findings OD and a window defect corresponding to the RPE changes OS (Figure 3A, C). There was no dye leakage or evidence of choroidal neovascular membrane on FA. On indocyanine green angiography, there was slight macular hypercyanescence but not the classic bright hypercyanescence and late washout found with a choroidal hemangioma (Figure 3B, D). Optical coherence tomography showed a normal retina OD and shallow subretinal fluid with RPE hyperplasia OS (Figure 4). In addition, on OCT, there was a dome-shaped elevation of the sclera OS more so than OD.
Based on the above findings, the patient was diagnosed with dome-shaped maculopathy (DSM) related to moderate myopia. Treatment options for the subretinal fluid associated with DSM include anti-VEGF intravitreal injection, photodynamic therapy and laser photocoagulation. This patient elected treatment with intravitreal bevacizumab.
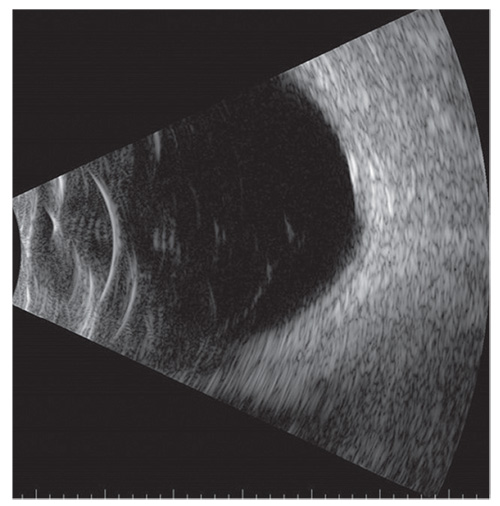 |
| Figure 2. Ultrasonography of the left eye demonstrates a slightly elevated, echodense, solid, dome-shaped mass. |
Discussion
Dome-shaped macula was originally described by Gaucher and colleagues.1 They characterized DSM by the appearance of an inward projection of the macular retina, RPE and choroid, often within a myopia-associated posterior staphyloma.1 Mechanistic explanations of this phenomenon have included geographic variation in vitreoretinal traction and intrinsic scleral wall resistance to the development of the scleral staphyloma.2 Others postulate that an area of underlying thick sclera located between areas of thin sclera leads to a relative difference in radial curvature between the scleral regions of varying thickness.3
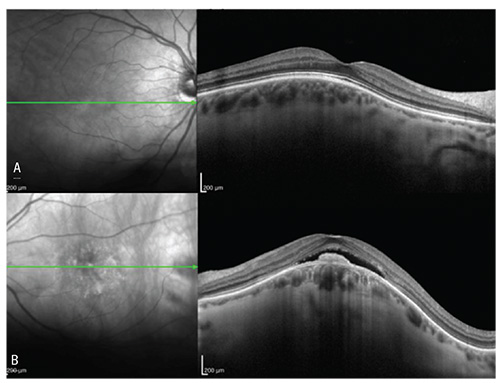 |
| Figure 4. Optical coherence tomography revealed (A) flat retina OD and (B) shallow subretinal fluid OS with a retinal pigment epithelial elevation. Both eyes demonstrated scleral thickening with a dome-shaped contour OS greater than OD. |
In addition to the myopic patients in whom DSM was first observed, more recently, the phenomenon has been demonstrated in hyperopia, inherited retinal dystrophies, and central serous chorioretinopathy.4 Associated complications include serous macular detachment in about half of eyes, extrafoveal retinoschisis in 20 percent of eyes, and choroidal neovascularization in 10 percent. Treatment for DSM is directed toward its complications.
Our patient demonstrates how DSM can masquerade as a choroidal hemangioma, consistent with prior descriptions.4 Choroidal hemangioma is a benign vascular tumor that, in its circumscribed form, can similarly present with decreased visual acuity from subretinal fluid associated with RPE changes.5 On FA, choroidal hemangioma demonstrates early hyperfluorescence in the pre-arterial filling phase with late diffuse hyperfluorescence of the mass and often leakage into the subretinal space.6 By ICGA, choroidal hemangioma characteristically shows rapid early hypercyanescence by one minute after injection of dye and subsequent late-phase “washout” of dye at >10 minutes, reflecting the high flow rate through this tumor.7-9 In contrast, non- or isofluorescence is observed with DSM on FA and ICGA.4 OCT of choroidal hemangioma is much different than DSM. By OCT, a choroidal hemangioma demonstrates a hyperreflective choroidal mass with expansion of choroidal vessels, whereas DSM shows elevation of the retina and choroid from an underlying scleral mass.1-2, 9
In conclusion, this is a case of a 56-year-old woman with a history of myopia, presenting with decreased visual acuity from subretinal fluid and an echodense submacular mass. She was originally diagnosed and treated for choroidal hemangioma elsewhere, but, upon further evaluation, she was discovered to have DSM. Although both choroidal hemangioma and DSM appear as echodense masses on ultrasonography, DSM can be differentiated from choroidal hemangioma by findings on FA, ICGA and, most reliably, OCT. REVIEW
1. Gaucher D, Erginay A, Lecleire-Collet A, et al. Dome-shaped macula in eyes with myopic posterior staphyloma. Am J Ophthalmology 2008;145:909-914.
2. Ng DSC, Cheung CYL, Luk FO, et al. Advances of optical coherence tomography in myopia and pathologic myopia. Eye (Lond) 2016;30:901-916.
3. Wood EH, Powers MA, Sanislo SR, Gaynon MW. Regarding ‘Advances of optical coherence tomography in myopia and pathologic myopia’. Eye (Lond) 2017;31:1114-1115.
4. Iyer PG, Say EM, Shields CL. Dome-shaped macula simulating choroidal hemangioma in a myopic patient. Oman J Ophthalmology 2015;8:188-90.
5. Shields CL, Shields JA. Intraocular Tumors. 3rd Ed. Wolters Kluwer 2016: 248-263.
6. Freund KB, Sarraf D, Mieler WF, Yannuzzi LA. The Retinal Atlas. 2nd Ed. Elsevier 2017: 858-862.
7. Arevalo JF, Shields CL, Shields JA, et al. Circumscribed choroidal hemangioma: Characteristic features with indocyanine green videoangiography. Ophthalmology 2000;107:344-350.
8. Shields CL, Honavar SG, Shields JA, et al. Circumscribed choroidal hemangioma: Clinical manifestations and factors predictive of visual outcome in 200 cases. Ophthalmology 2001;108:2,237-2,248.
9. Rojanaporn D, Kaliki S, Ferenczy SR, Shields CL. Enhanced depth imaging optical coherence tomography of circumscribed choroidal hemangioma in 10 consecutive cases. Middle East Afr J Ophthalmology 2015;22:192-197.



