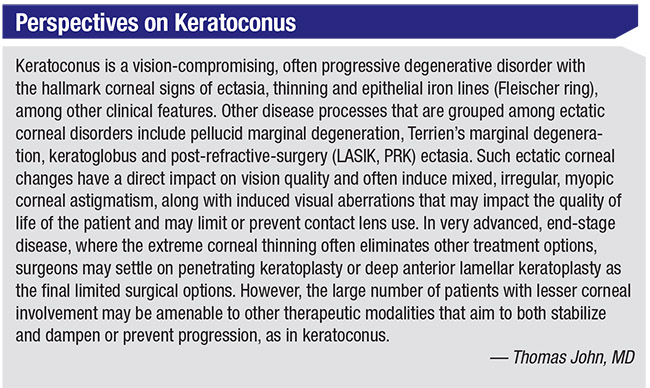
The treatment of corneal ectasias such as keratoconus, pellucid marginal degeneration and post-refractive ectasia has undergone a significant shift in recent years. New treatment options offer not only stabilization of the progressive nature of these conditions, but also corneal flattening and improved visual outcomes, enabling surgeons to intervene earlier in the disease course and avoid penetrating keratoplasty.
Two technologies that have gained recent attention, both independently and used in conjunction with one another, are intracorneal ring segments and corneal collagen cross-linking. In this column, I’ll describe my surgical approach of combining intracorneal ring segments with cross-linking for the management of ectatic corneal disorders, and discuss situations in which one approach might be preferable to the other.
Intacs
Intacs corneal ring segments (Addition Technology; Fremont, California) are the only ICRS available in the United States; they were originally designed for the correction of low degrees of myopia. The intracorneal implants, when placed in the peripheral cornea outside of the optical zone, cause a flattening of the central cornea, thus reducing myopia and mild astigmatism. However, given the advancements and excellent outcomes of excimer laser ablation techniques, intracorneal ring segments like Intacs were largely relegated to treatment of irregular corneas. Intacs were subsequently FDA approved for the correction of myopia and astigmatism associated with keratoconus, in 2004. Candidates for Intacs are patients whose steepest K values are less than 58 D, who have clear visual axes and corneal thicknesses of at least 450 um at the 7 mm optical zone.1 Placement can be performed using either mechanical or femtosecond-created channels. Outside of the United States, Ferrara rings and Kerarings (Mediphacos; Belo Horizonte, Brazil) are the other two commonly used ICRS models.
One of the unique properties of ring segments, which are made of polymethylmethacrylate and come in a range of sizes, is the ability to normalize a highly ectatic cornea by centralizing the cone and reducing maximum corneal curvature. Doing so can often decrease the amount of irregular astigmatism and higher-order aberrations seen in these patients, improve best spectacle-corrected visual acuity, and improve contact lens tolerance.2 There are mixed results in the literature regarding regression of the flattening effect seen after Intacs implantation. Though not indicated for the stabilization of progression in keratoconus, some have reported stabilization associated with ring segment placement: A five-year study in patients treated with Intacs for progressive keratoconus noted that 92.9 percent of eyes showed no significant progression in steepest K value during the course of follow-up,3 while a separate study of patients with previously documented progressive keratoconus and Intacs or Keraring placement demonstrated regression in the mean K value by 3.36 D postoperatively at five years.4
Cross-linking
Corneal collagen cross-linking was approved by the FDA in July 2016 for the treatment of progressive keratoconus and post-refractive ectasia. The procedure, involving the saturation of the cornea stroma with riboflavin (vitamin B2) and subsequent UVA irradiation, increases the biomechanical stability of the tissue by forming chemical bonds between collagen fibrils.5 While only recently approved in the United States, there’s a vast amount of data on the stability and visual acuity results of cross-linking for keratoconus in the literature due to its popularity abroad. Originally described in 2003, cross-linking has been shown to halt progression of the disease with improvement of visual acuity and a variable amount of reduction in steepest K values.5,6 In addition to keratoconus, collagen cross-linking has been used with similar success in other forms of cornea ectasia, including pellucid marginal degeneration7 and post-refractive-surgery ectasia.8
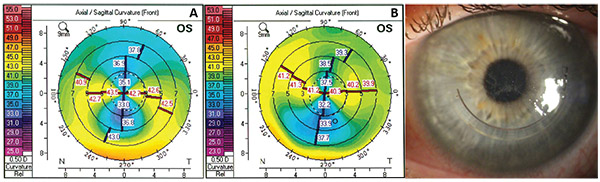 |
| Figure 1. The left eye of a 51-year-old patient with unilateral topographic changes consistent with pellucid marginal degeneration. Anterior curvatures measured by the Pentacam are shown. A) Significant PMD-like ectasia pattern at presentation. B) Improved curvature pattern three months after single Intacs ring segment placement with same-day epithelium-off CXL. C) Slit lamp photograph showing the position of the single ring segment. The patient’s topographic indices decreased after the procedure (steep K value decreased by 2.3 D, anterior corneal cylinder by 2.7 D). |
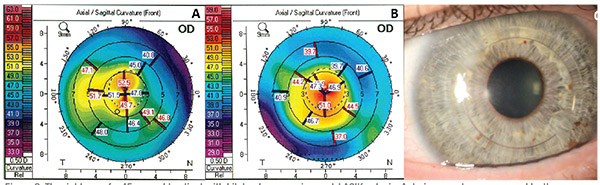 |
| Figure 2. The right eye of a 45-year-old patient with bilateral progressive post-LASIK ectasia. Anterior curvatures measured by the Pentacam are shown. A) Severe steepening with eccentric cone with max K value of 58 D. B) Improved centralization of cone and decreased max K value of 55.2 D after paired Intacs ring segment placement with same-day epithelium-off CXL. C) Slit lamp photograph showing paired ring segments. |
Where Do the Technologies Fit?
In current practice, cornea specialists have both tools at their disposal, and both can play an important role in corneal ectasia management. But in which scenarios does crosslinking make sense? When does one consider ICRS? And does it ever make sense to use both in conjunction with one another?
• The case for cross-linking. In our practice, patients who have classic topographic changes on the anterior and posterior cornea, a clear central cornea and documented progression of myopia or astigmatism are generally offered cross-linking. Nearly all candidates will have a clear central optical axis and a minimum corneal thickness greater than 400 μm. In general, we find patients meeting these criteria to be in the earlier stages of disease progression. Age is a consideration, since the natural history of keratoconus is thought to be one of slowed progression with time. However, there is evidence in the literature that keratoconus can continue to progress beyond age 30, suggesting that the benefit of cross-linking may not be limited to the young patient.9 Thus, progression in keratometric indices over sequential exams at any age should trigger consideration of corneal cross-linking.
Other types of patients who may benefit from cross-linking at an older age are those with suspected topographic progression and concomitant cataract, as the stabilization and flattening may improve the accuracy of the preoperative biometry and reduce the risk of progressive postoperative myopic shift.10 Literature on the subject is sparse, but stabilizing keratometric indices prior to intraocular lens power calculation in a case of progressive ectasia should be considered essential for the patient with corneal ectasia and cataract.
• The case for Intacs. While there has been documentation of slowing keratoconus progression after placement of Intacs, the largest benefit of ring segments seems to be the reduction in the amount of corneal cylinder and centralization of the cone. In our practice, the patients we consider the best candidates for Intacs are those with moderate to severe keratoconus and a clear central optical zone who have developed contact lens intolerance. As in the published literature, we have noted the greatest visual improvement gains in patients with more advanced disease.11 A 2012 study found that in moderate to severe cases of corneal ectasia, Intacs were able to flatten the steepest K by an average 6.7 D, and allowed contact lens tolerance in all cases.12 Ring segments may be placed in single or paired fashion with both methods demonstrating significant effect on refractive parameters and visual acuity.13 (See Figures 1 and 2 for case examples.) In those patients for whom the Intacs don’t completely eliminate intolerance to rigid gas permeable lenses, we have found success with fitting scleral contact lenses over the ring segments, which is supported by the literature.14
• The case for the combination. Given the unique strengths of both individual treatment types—the stabilizing effect of corneal collagen crosslinking and the flattening power of ICRS—one can imagine a potential synergistic effect of using both technologies. While there are mixed results in the literature regarding their additive effect on outcomes, many surgeons believe the mechanical flattening of ICRS can further potentiate the flattening effect of the crosslinking.2
Choosing to perform both procedures, versus one or the other, may depend on a number of factors, not the least of which is insurance coverage and the patient’s ability to afford potentially uncovered services. From a patient-benefit standpoint, any case of progressive keratoconus should be considered a candidate for cross-linking, and ICRS can be considered in moderate to severe cones or patients presenting with contact lens intolerance. These more advanced cases, often with worse presenting BCVA and SE, may stand to gain the most from the combination of both thera pies.15 In our practice, we follow some general guidelines for patient selection, as described in the accompanying description of the patient in the case discussed in Figure 1.
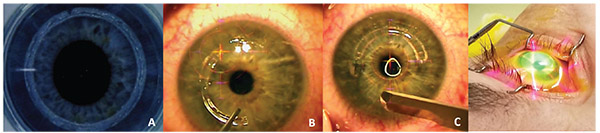 |
| Figure 3. Combining Intacs with same-day corneal cross-linking: A) Femtosecond creation of ring-segment channels; B) placement and securing of Intacs; C) epithelial debridement; and D) standard corneal cross-linking following the Dresden protocol. |
When using both cross-linking and ICRS, simultaneous or sequential therapy can be considered. However, there is debate about which treatment paradigm is more effective. Simultaneous therapy represents the least recovery time, which can be important in these patients, who are often younger, working-age individuals with progressive keratoconus. When directly compared, combining ICRS with same-day CXL has demonstrated greater reduction in cylinder and keratometric indices than ICRS alone.16 While individual protocols of riboflavin administration vary, some studies indicate transepithelial17 and intra-channel18 riboflavin may provide adequate saturation of corneal stroma without epithelial debridement, further decreasing recovery time.
Sequential ICRS and CXL has also been studied in the literature, with many authors theorizing that the flattening effect of CXL may be potentiated by the existing mechanical flattening of the cornea by the ring segments.19 This has been demonstrated in post-LASIK ectasia cases as well.20
 |
My Combined Procedure
We currently perform same-day combined Intacs with CXL when both are indicated. After prepping the eye in a way similar to that of other corneal refractive procedures, we use a femtosecond laser to create the intracorneal ring channels at two-thirds corneal depth. The rings are inserted under the laser microscope and a 10-0 nylon suture is placed at the channel entrance. Next, the epithelium is debrided from the optical zone and peripherally over the implanted ICRS. Riboflavin is then administered as described in the Dresden protocol, and standard CXL is completed (Figure 3). The Dresden protocol consists of applying 0.1% riboflavin-5-phosphate and 20% dextran T-500 to the corneal surface 30 minutes before irradiation and at five-minute intervals during the course of a 30-minute exposure to 370-nm UVA with an irradiance of 3 mWcm2.
Regardless of the treatment pattern chosen, ICRS and CXL represent two major advances in the treatment of progressive corneal ectasia that together have dramatically reduced the need for penetrating keratoplasty. Whether used independently, in sequence or in combined fashion, there is an ever-increasing body of literature demonstrating good outcomes and safety profiles, giving corneal surgeons effective options for management of corneal ectasia. REVIEW
Brandon J. Baartman, MD, is in private practice at Vance Thompson Vision in Omaha, Nebraska. He can be reached at brandon.baartman@ vancethompsonvision.com. Dr. John can be reached at 708-429-2223 or by email at tjcornea@gmail.com. Dr. Baartman has no financial interest in any of the products mentioned in the article.
1. Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treating keratoconus: One-year results. Ophthalmology 2001;108:1409–1414.
2. Avni-Zauberman N, Rootman DS. Cross-linking and intracorneal ring segments – review of the literature. Eye & Contact Lens 2014;40:365-370.
3. Bedi R, Touboul D, Pinsard L, Colin J. Refractive and topographic stability of Intacs in eyes with progressive keratoconus: Five-year follow-up. J Refract Surg 2012;28:6:392–396.
4. Vega-Estrada A, Alio JL, Plaza-Puche AB. Keratoconus progression after intrastromal corneal ring segment implantation in young patients: Five-year follow up. J Cataract Refract Surg 2015;41:1145-1152.
5. Gaster RN, Caiado Canedo AL, Rabinowitz YS. Corneal collagen cross-linking for keratoconus and post-LASIK ectasia. Int Ophthalmol Clin 2013;53:1:79-90.
6. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003;135:620–627.
7. Mamoosa B, Razmjoo H, Peyman A, Ashtari A, Ghafouri I, Moghaddam AG. Short-term result of collagen crosslinking in pellucid marginal degeneration. Adv Biomed Res 2016;5:194.
8. Yildirim A, Cakir H, Kara N, Uslu H, Gurler B, Ozgurhan EB, Colak HB. Corneal collagen crosslinking for ectasia after laser in situ keratomeliusis: Long-term results. J Cataract Refract Surg 2014;40:10:1591-1596.
9. Gokul A, Patel DV, Watters GA, McGhee CN. The natural history of corneal topographic progression of keratoconus after age 30 in non-contact lens wearers. Br J Ophthalmol 2017;101:839-844.
10. Moshirfar M, Walker BD, Birdsong OC. Cataract surgery in eyes with keratoconus: A review of the current literature. Curr Opin Ophthalmol 2018;29:1:75-80.
11.Vega-EstradaA,AlioJL,BrennerLF,JavaloyJ,PlazaPucheAB, Barraquer RI, Teus MA, Murta J, Henriques J, Uceda-Montanes A. Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive and aberrometric impairment. Am J Ophthalmol 2013;155:3:575-584.
12. Khan MI, Injarie A, Muhtaseb M. Intrastromal corneal ring segments for advanced keratoconus and cases with high keratometric asymmetry. J Cataract Refract Surg 2011;38:129136.
13. Yeung SN, Fu JYF, Lichtinger A, Low SAW, Kim P, Rootman DS. Efficacy of single or paired intrastromal corneal ring segment implantation combined with collagen crosslinking in keratoconus. J Cataract Refract Surg 2013;39:1146-1151.
14. Rathi VM, Mandathara PS, Dumpati S, Sangwan VS. Scleral lens after intracorneal ring segments in patients with keratconus. Cont Lens Anterior Eye 2018;41:2:234-237.
15. Vincente L, Boxer-Wachler BS. Factors that correlate with improvement in vision after combined Intacs and trans-epithelial corneal crosslinking. Br J Ophthalmol 2010;94:1597-1601.
16. Chan CCK, Sharma M, Wachler BS. Effect of inferior-segment Intacs with and without C3-R on keratoconus. J Cataract Refract Surg 2007;33:75–80.
17. Ertan Q, Karacal H, Kamburoglu G. Refractive and topographic results of transepithelial cross-linking treatment in eyes with Intacs. Cornea 2009;28:719–723.
18. Kilic A, Kamburoglu G, Akinci A. Riboflavin injection into the corneal channel for combined collagen crosslinking and intrastromal corneal ring segment implantation. J Cataract Refract Surg 2012;38:878–883.
19. Coskunseven E, Jankov MR, Hafezi F, et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg 2009;35:2084–2091.
20. Kamburoglu G, Ertan A. Intacs implantation with sequential collagen cross-linking treatment in postoperative LASIK ectasia. J Refract Surg 2008;24:726–729.




