 |
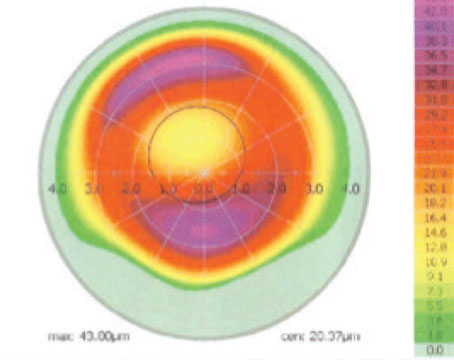
| This ablation plan shows the potential problem with custom enhancements. It calls for 62.6 µm of tissue to be removed from the center of the cornea. Andrew Caster, MD |
Potential Problems
"One of main problems with custom enhancements, particularly if the patient has a lot of spherical aberration, is that the patient tends to end up hyperopic," says Los Angeles surgeon Andrew Caster, who primarily uses the Alcon LadarVision CustomCornea system. He is wary of custom enhancements. "It's common that the custom enhancement will not be the final treatment; you'll need to do a non-custom hyperopic correction afterward.
"The other problem with custom enhancements is that they use up a lot of central corneal tissue. Many of the patients I've evaluated for custom enhancements would need up to 50 or 60 µm of central corneal tissue removed when they only have less than a diopter to correct. Obviously, we're all concerned about ectasia, and we want to preserve central corneal tissue. So, the trade-off of possibly lowering the patient's higher-order aberrations but using up so much central corneal tissue may not be worthwhile." He also notes that removing so much central tissue may limit the patient's future refractive surgery options.
Ronald Krueger, MD, director of refractive surgery at the Cleveland Clinic, recalls a patient he consulted on who had a nightmarish custom enhancement experience.
"A surgeon from out-of-state called me about a patient who had 2 D of myopia left after his primary surgery, so the surgeon decided to just go back and do a custom retreatment," Dr. Krueger says. "The results were bad. When I asked him to check the ablation printout for how deep the ablation was, it read 100 µm. The surgeon happened to do a surface ablation, thinking he might conserve some tissue, but the 100-µm ablation made the patient +5—a huge overcorrection."
Dr. Krueger says the custom treatment takes so much tissue because it's trying to treat all the aberrations it finds, in addition to the spherocylindrical error. "To treat all those aberrations, you have to take the tissue down to a lower level to make it planar," he says. "And that's just so deep you're going to get biomechanical shifts that lead to overcorrection."
Because of the potential for such cases, Dr. Caster says he's been shying away from performing custom enhancements in favor of conventional ones, unless a patient is extremely symptomatic.
"When a patient comes back after the initial surgery, we put a pair of glasses on him to show what his vision would be like with a conventional enhancement. If he says, "The quality of my vision with these glasses is really terrible,' then that's the type of situation where you'd consider doing a custom enhancement. If, however, he tries on the glasses and says, 'Wow! That's terrific!' then I'd highly recommend that you do a conventional enhancement on him instead of a custom one."
Fortunately, the LadarVision system provides a surgical planning map that shows where the greatest amount of tissue will be removed during the treatment. "With this, the surgeon can see how much tissue will be removed, and, if it's too much, can fall back to a conventional enhancement," says Dr. Caster.
Some surgeons, though, have been more pleased with custom enhancements, and say they yield good results. Care is still required, however, to avoid too much hyperopia postop.
 |
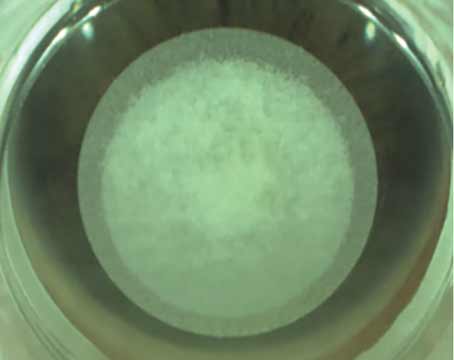
| A post-LASIK patient with complaints of poor visual quality and significant glare, halos and night vision problems in his right eye. Spectacles and soft contact lenses do nothing for the symptoms. Edward Manche, MD |
"I basically do all my patients, both primary and enhancements, using custom," says Stanford University's Edward Manche, MD. He uses the Visx system for most of the enhancements. "You can shrink the treatment zone size down a bit to conserve more tissue. For example, say a patient is -1 with 1 D of cylinder, and the laser parameters call for the removal of 23 µm of tissue, but you don't want to remove that much, you could shrink the optical zone of the retreatment a bit to conserve some tissue." The other laser system he uses, the Bausch & Lomb Zyoptix, allows users to shrink the optical zone size, but he says it uses a bigger blend zone than the Visx, which causes it to remove about 10 to 20 percent more tissue than the Visx per unit treated.
He says the risk involved with doing an enhancement increases if the enhancement patient is a referral. "If the patient's primary procedure wasn't yours, you have to be very careful in measuring the residual stromal bed before doing the enhancement in that case," he says. "But if it was your primary, and you know the flap thickness and how much residual tissue there was remaining, then you can go ahead and treat pretty safely."
However, Dr. Manche adds, a custom enhancement isn't right for all cases. "I rarely run across a case where I wouldn't use custom, but there can be cases where I wouldn't do an enhancement with either custom or conventional," he says. "This type of case would be someone with a best-corrected acuity of only 20/30 or 20/40, which may be due to irregular astigmatism if there's any problem with the flap or striae. You really want to consider that patient carefully. There also may be a patient with a significantly decentered ablation that's off by 2 mm and his original correction was -7 D or above. A custom retreatment on such a case wouldn't work well at all."
Successful Strategies
Here are the steps surgeons recommend taking to get the best results from custom enhancements while minimizing the risks.
"I feel pretty strongly that, for the most part, using custom for enhancement makes the most sense," says Minneapolis surgeon David Hardten. "There are some things that are important, though. If you're going to lift the flap for the enhancement, make sure the flap is big enough for the size of the treatment. I prefer at least 8 mm of treatable area. Also, patients are at a little bit higher risk for epithelial ingrowth if they're further out postop."
 |
| The custom ablation plan for the post-LASIK patient with irregular astigmatism from page 49. The surgeon decided on a flap-lift retreatment. Edward Manche, MD |
Dr. Hardten also looks at the patient's 3-, 4-, 5- and 6-mm wavefront maps on his Visx system, even though he says patients will usually do well if their manifest refraction matches the 4-mm wavefront. "It's another way of looking at spherical aberration and what effect it's having on the refraction," he explains. "The wavefronts at the different diameters don't vary much in normal eyes, but in patients who have had previous standard LASIK you'll see spherical aberration; so the 3-mm might be more or less myopic and the 6-mm one might be more myopic because you're collecting some light rays from around the edges, where the transition zone is. In the patients with the real high spherical aberration that suggests a real high myopic value, you may have to be more careful about doing the full treatment with the wavefront. You have to be careful, in a sense, that you don't overtreat those patients."
 |
| The six-month wavefront of the custom LASIK retreatment described above. The uncorrected vision went from 20/50 to 20/16, and the higher-order RMS value of the aberrations decreased from 0.48 to 0.18. Edward Manche, MD |
Dr. Manche recommends a liberal use of the surgeon offset that your system offers to avoid this overtreatment. "You can offset the treatment up to 0.75 D," he says. "You can also do a percentage reduction of the treatment on the Visx by 10 to 20 percent, in addition to the offset. This is helpful because even if the wavefront and manifest refractions match up, say they're about -2 D in each, if you program -2 D into the wavefront treatment, you will generally end up overcorrecting by 0.5 or 0.75 D. So you really want to back off. Even if the wavefront, manifest and cycloplegic refractions were in agreement, I'd still back off no less than 0.5 D, maybe even 0.75 D, to only treat -1.25 D. This is especially true in the more aberrated eyes where you tend to get more overcorrection."
Dr. Krueger also swears by the use of the offset. "Right now, if it's an enhancement on a patient who had a custom primary procedure, I'll use a small offset, maybe 0.25 D or none, depending on factors such as the ablation depth," he explains. "I do this because since it was previously custom, there weren't a lot of aberrations generated, so now when I do a custom again I should be able to pretty much get the correction I plug into the system. But when I do a custom retreatment of a previous conventional treatment, especially if the patient was a high myope, I'll almost always go to a higher offset, like 0.75 D, or maybe 0.5 D."
In the near future, however, Dr. Krueger says surgeons may have more flexibility in their custom enhancements. "Probably in the next two months or so, the FDA will announce that we will be able to go up to +2.5 D and around - 1 D with our offsets," he says. "That should give us the flexibility we need to do custom enhancements and back off quite a bit on the spherical part of treatments. We'll be able to better control things, but, of course, we'll need to know what the relationship is between the offset and the aberrations; in other words, how much of a target offset compensates for how much preop spherical aberration? Though we don't have the numbers completely together yet, after an analysis of the previous custom retreatments we've done, we do know the preop spherical aberration is correlated to the postop spherical equivalent overcorrection."
Using these strategies, most of the surgeons to whom we spoke say their results have been acceptable in custom enhancements.
Dr. Hardten used custom enhancements on 83 eyes of 69 patients with an average pre-enhancement error of -1 D, with 0.48 D of cylinder. The average spherical aberration RMS error was 0.18. The average follow-up was six months. He analyzed the case series retrospectively.
Post-enhancement, 70 percent of the patients see 20/20 or better uncorrected, and all see 20/40 or better. The average refraction is a little hyperopic, +0.14 D. None of the eyes lost more than a line of best-corrected visual acuity. He says these patients achieved significantly better Snellen acuity than a similar group of 164 eyes that he and his colleagues analyzed in a different study of conventional retreatments. In the conventional study, 46 percent of the eyes could see 20/20 or better uncorrected post-enhancement, and 95 percent saw 20/40 or better.1
Dr. Manche performed a similar retrospective analysis of 120 eyes of 102 patients; one of the eyes had previous PRK, while the rest were LASIK patients. At three months, the mean refractive error was -0.20 (down from -0.91 D preop), and all the eyes were within ±0.75 D of emmetropia. All of the eyes showed equal or improved UCVA (range 20/15 to 20/30) with 20/20 or better in 74 of the 84 eyes (88 percent) available for follow-up at three months.2
Overall, when armed with the right target offset and reliable data, Dr. Krueger says he feels comfortable doing custom enhancements.
"If overcorrections occurred in a large percentage of them, I'd stop doing them," he says. "I'm at a comfort level where I can keep doing them."
1. Davis EA, Hardten DR, Lindstrom M, Samuelson TW, Lindstrom RL. LASIK enhancements: A comparison of lifting to recutting the flap. Ophthalmol 2002;109:2308-14.
2. Montague AA, Manche EE. CustomVue laser in situ keratomileusis treatment after previous keratorefractive surgery. J Cataract Refract Surg 2006;32:5:795-8.
Some surgeons, when faced with certain suspect custom enhancement cases, will turn away from LASIK and instead perform PRK over the LASIK flap.
When to Come to the Surface