|
Mark B. Abelson, MD, and ORA Clinical |
The 2006 Association for Research in Vision and Ophthalmology annual meeting in Ft. Lauderdale, Fla., upheld its reputation, yet again, as the ultimate forum for ophthalmic research. A record-breaking 10,200 participants were present this year. The amazing quantity of fields covered and research results presented made the week a busy one for all who attended. As it is virtually impossible to canvass the vast expanses of research presented each day, we hope this summation of some interesting highlights will prove useful both for those who could not attend as well as those who did visit this year's ARVO meeting.
Anti-Infectives and Anti-Inflammatories
The anti-infective arena saw Phase III results presented from an active-controlled azithromycin clinical trial. In this study, InSite's 1% azithromycin ophthalmic solution (AzaSite) dosed b.i.d. for the first two days and q.d. for days three to five was equivalent to tobramycin 0.3% q.i.d. ophthalmic solution in the treatment of bacterial conjunctivitis, using clinical cure and bacterial eradication as the clinical endpoints (Abelson MB, et al. IOVS 2006; 47:ARVO E-Abstract 3589). The azithromycin ophthalmic solution represents an advance in the treatment of bacterial conjunctivitis, with its lower-frequency dosing schedule than currently available options such as tobramycin.
Quickly and accurately identifying pathogens in corneal ulcers is often challenging. An advance that could help solve these problems was presented by researchers who showed that more rapid and accurate identification of pathogens from corneal ulcers can be achieved using a polymerase chain reaction (PCR) test (Qi et al. IOVS 2006; 47:ARVO E-Abstract 3582). In the study, a PCR test identified pathologic bacteria in two specimens that were negative in both smears and cultures.
Similar results were obtained in a separate study of endophthalmitis specimens, which also identified positive specimens through PCR that were negative when cultured (Therese KL, et al. IOVS 2006; 47: ARVO E-Abstract 1890).
In the field of anti-inflammatory research, one study examined hydrocortisone 1% supplemented with anionic polar phospholipid (APP) cream compared with hydrocortisone 1% cream (Hytone) for the treatment of inflammatory eyelid disease. The hydrocortisone-supplemented APP cream showed 75 times greater penetration at four hours and 20 times greater penetration at eight hours. The APP vehicle may allow for a lower concentration of topical steroid to be dosed while still maintaining efficacy (Greiner, et al. IOVS 2006;47:ARVO E-Abstract 600). This formulation might become particularly useful in the long-term treatment of eyelid dermatoses where corticosteroids may be the appropriate treatment, but could be applied in lower dosages.
Another advance in the arena of anti-inflammatory therapies was research presented on TNF-alpha inhibitors as potential treatments for posterior segment inflammatory disease. Results presented from the Remicade European Study for Chronic Uveitis (RESCU) showed that infliximab (Remicade, Centocor) was generally well-tolerated and effective when used to treat uveitis (De Smet MD. IOVS 2006; 47:ARVO E-Abstract 1525). Two other studies revealed similar findings, indicating that other TNF-alpha inhibitors, such as adalimumab, may also be effective in the treatment of posterior segment inflammatory disease (Rozenbaum I, et al. IOVS 2006;47:ARVO E-Abstract 2437; Zierhut M, et al. IOVS 2006; 47:ARVO E-Abstract 1526).
Dry Eye
Dry eye research presented at this year's ARVO included advances in diagnosing and categorizing, etiological aspects, and treating and managing dry eye.
Many researchers acknowledge that tear-film breakup time (TFBUT), though widely used, remains a limited tool for diagnosis of dry-eye syndrome because it offers clues, but often an incomplete picture of the condition. The computer-driven Tear Stability Analysis System (TSAS) may help create a more holistic determination of tear-film stability. This system superimposes a color-coded topographical image over video of the ocular epithelium to determine the areas in which the tear film has parted. It repeats this imaging process each second over a 10-second interval and calculates a breakup index (BUI), the value of which reflects the rapidity of breakup and the unprotected ocular surface area at each time point. While it is a more complete method of measuring tear-film stability, and may prove useful in research, TSAS uses highly advanced technology that could limit its potential as a basic diagnostic tool for everyday clinical use (Hara, S et al. IOVS 2006;47:ARVO E-Abstract 235).
Tear-film breakup patterns (TFBUP), though not a replacement for breakup time measurements, also appear to have potential as a novel diagnostic tool. Five TFBUPs have been identified: linear; fractured; wispy; spotting; and amorphous blob. Each pattern may indicate a specific type or severity level of dry eye, and certain patterns are strongly correlated with longer or shorter TFBUTs. A wispy pattern is thought to be representative of very severe dry eye, because it was seen in eyes with exceptionally short breakup times. The amorphous blob pattern appeared most indicative of a healthy tear film. Further study of patterns using a population of Ashkenazi Jewish subjects—a group having uniform dry-eye etiology—demonstrated that both reflex tearing and meibomian gland expression are capable of altering TFBUP. With additional study, tear-film breakup patterns hold promise for use as a clinical diagnostic tool in the near future (Schindelar MR, et al. IOVS 2006;47:ARVO E-Abstract 5610; Casavant JS, et al. IOVS 2006;47:ARVO E-Abstract 282; Wilcox KA, et al. IOVS 2006; 47: ARVO E-Abstract 283).
The goblet cells that generate the mucin layer have also been a point of interest. One study showed that LASIK surgery can affect goblet cell populations. Post-LASIK patients displayed decreased goblet cell populations, most likely due to the pressure put on the ocular epithelium by the suction ring in such procedures. This suggests that any sustained pressure applied to the ocular surface could influence goblet cell density, mucin layer generation, and consequently, tear-film stability (Rodriguez E, et al. IOVS 2006;47:ARVO E-Abstract 273).
Dry-eye therapies were also a focal point of research. Alcon recently introduced its new liquid gel tear substitute, Systane Free. This product, featuring a novel preservative-free ionic buffer system, demonstrated significantly greater patient acceptability (p<0.0008) and lesser blur profile (p<0.0001) than Refresh Liquigel (Allergan), a liquid gel containing 0.1% CMC (Christensen MT, et al. IOVS 2006;47:ARVO E-Abstract 274). In the same study, Alcon researchers say the Systane Free eye drop shows significant (p=0.05) reduction in corneal staining relative to Refresh Tears (Allergan) at six weeks.
In the process of investigating omega-3 fatty acids in macular degeneration therapy, a potential application for dry eye was found. Study results indicated that food supplements containing n-3 FA, ALC and CoQ10 may improve dry-eye symptoms of elderly patients, while further improvement may be reached by concomitant treatment with vitamin A (Feher J, et al. IOVS 2006;47:ARVO E-Abstract 246).
Allergy
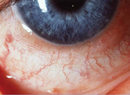
Though allergic rhinitis and allergic conjunctivitis are known to be prevalent throughout the industrialized world, these conditions remain largely underdiagnosed and undertreated. This topic was the subject of a symposium focusing on the allergic condition (Bielory L, Barney NP, Abelson MB, Keane-Myers AM, ARVO 2006, Session 427). Speakers discussed the importance of understanding the connection between rhinitis and conjunctivitis and of incorporating ocular examinations into allergy assessments and vice versa. Speakers addressed different mechanisms involved in ocular allergies, and the manners in which they differ according to disease profile, such as the differing ocular mast cell response to secretagogues according to their location in the eye. The mast cells in allergic conjunctivitis are located primarily in the substantia propria ,while mast cells involved in chronic allergic conditions are also found in conjunctival epithelial tissue. Such differences accordingly give rise to distinguishing signs and symptoms.
A number of studies involving novel or marketed anti-allergy therapies were presented this year, including work stemming from prior evidence of the potential efficacy of a probiotic in managing allergic inflammation by modulating the Th1/Th2 balance. After two weeks of treatment with a probiotic eye drop (Lactobacillus acidophilus in saline solution), four out of six vernal keratoconjunctivitis subjects showed significant (p=0.028) improvement of symptoms, and five showed an improvement of symptoms and signs at four weeks. The authors concluded that further extended studies are warranted to determine the potential use of Lactobacillus acidophilus in treating the signs and symptoms of VKC (Iovieno A, et al. IOVS 2006; 47: ARVO E-Abstract 4998).
Two separate anti-allergy therapies were evaluated for their ability to prevent signs and symptoms of ocular allergy using the conjunctival allergen challenge (CAC) model, a standardized, well-controlled, reproducible means of measuring drug efficacy. In a double-masked crossover study, researchers compared the efficacy of desloratadine 5 mg (Clarinex, Schering-Plough) to placebo for prevention of signs and symptoms of ocular allergy. Following a week of once-daily dosing, desloratadine was significantly more effective than placebo in the prevention of ocular itching at three, five and seven minutes post-CAC (p<0.001), with similarly significant results achieved in preventing redness, chemosis, lid swelling and tearing (Goodhue K, et al. IOVS 2006;47:ARVO E-Abstract 4977). Another study assessed the efficacy of prednisolone acetate 1% ophthalmic suspension (Pred Forte, Allergan) versus placebo. Results indicated that prednisolone acetate 1% is a potent preventative of the signs and symptoms of ocular allergy, and that a modified CAC model appears useful for the evaluation of new steroids and for bioequivalence studies (Gomes PJ, et al. IOVS 2006;47:ARVO E-Abstract 4978).
Basic Science
The pathology of glaucoma, optic nerve injury, neuroprotection, regeneration and viability were hot topics in basic research this year. Of particular interest were studies evaluating responses to optic nerve crush. One such study analyzed markers for functional changes including cell division, chemokine receptor changes, differentiation, cytotoxicity and activation of astrocytes over six days following injury. The researchers also tracked markers for phagocytosis, activation, p38 MAPK, cytotoxicity and paracrine cell signaling in microglia from day two to day 10. Researchers found that the microglia, once activated following the nerve injury, expressed these chemical signals with different functions in differing temporal patterns as the 10-day observation period progressed (Wang AL et al. IOVS 2006;47:ARVO E-Abstract 1240).
Another study assessed potential genetic markers for degeneration in response to optic nerve crush. The study evaluated retrograde degeneration of retinal ganglion cells in WldS mutant mice and normals and determined that degeneration did not differ. This result suggests that the WldS protein doesn't prevent degeneration of ganglion cells after optic nerve crush (Yuan M, et al. IOVS 2006;47:ARVO E-Abstract 1262).
The wealth of research being conducted on neuroprotective agents and glaucoma optic neuropathy provides a promising basis for clinical development of neuroprotective agents to complement existing IOP-lowering drugs. From the perspective of the clinician, such advances could represent a coming shift in the paradigm of treatment strategy for the glaucoma patient.
Investigation of the immunologic underpinnings of allergy also presented an interesting avenue of basic research. As our knowledge of the complex relationships between inflammation and allergy grows, researchers in immunology continue to examine the specific interactions where these two areas come together. One study in mice evaluated the implications of active allergic conjunctivitis during corneal transplant. The study revealed that mice sensitized and challenged with short ragweed pollen to induce allergic conjunctivitis experienced accelerated rejection of corneal allografts compared to naïve mice and sensitized but un-challenged mice (Flynn TH, et al. IOVS 2006;47:ARVO E-Abstract 1300). This type of research may provide insight into the conditions that will facilitate a higher probability of graft survival, perhaps better enabling clinicians to use appropriate treatments in a way that maximizes the chances for success.
Age-Related Macular Degeneration
The treatment landscape for age-related macular degeneration therapies continued to shift this year. Discussions of combination therapy and the efficacy of various drug regimens dominated. Ranibizumab (Lucentis) and bevacizumab (Avastin), in particular, received a considerable amount of attention.
Highlights included a report presented by Philip Rosenfeld, MD, PhD, and colleagues from the Prospective OCT Imaging of Patients with Neovascular AMD Treated with Intra-Ocular Lucentis (PrONTO) study, conducted at Bascom Palmer Eye Institute in Miami (Rosenfeld PJ, et al. IOVS 2006;47:ARVO E-Abstract 2948). The study enrolled 40 neovascular AMD patients with central macular thickness of > 300 µm, as measured by OCT and visual acuity from 20/40 to 20/400. Patients were administered three consecutive monthly injections of ranibizumab, which was followed by retreatment only if one of the following conditions was present:
• a loss of five letters of visual acuity with recurrent fluid (confirmed by OCT);
• increase in central OCT thickness of > 100 µm;
• new classic neovascularization or new macular hemorrhage.
Though the results are limited—only seven months of follow-up were reported—patients did show a marked decrease in the number of retreatments required. Approximately half of the eyes required no retreatment at the seven-month time point; however some patients with aggressive lesions, considered retinal angiomatous proliferation, qualified for retreatment at every visit.
This study will continue for two years and will provide insight into the clinical need for retreatment. Data from this and other studies could provide evidence for reducing the number or frequency of injections in some patients. Also, longer-duration treatments such as anecortave acetate (Retaane), which is administered every six months via a posterior juxtascleral depot, may find a niche in providing baseline prevention of progression of neovascular lesions.
The clinical safety results from the ranibizumab MARINA study were presented by Harvard's Joan Miller, MD, and colleagues (Miller JW, et al. IOVS 2006;47:ARVO E-Abstract 3539). Not surprisingly, the two-year safety data presented were similar to the one-year data presented previously, but the study questioned the effect of continued exposure to potent anti-VEGF molecules such as ranibizumab and bevacizumab. No one has yet established when a clinician should stop injections of an anti-VEGF agent. Common practice leads many physicians to reduce treatments when neovascularization has been controlled. However, reducing the number of treatments is not always possible, especially with very aggressive lesions. Additional research is needed and this topic is likely to generate much discussion at subsequent meetings, especially given that anti-VEGF combinations are now possible.
The scope of research presented at ARVO seems to expand each year. This year was no exception, and it appears the trend will continue. As long as it does, the conference will continue to be the place where—more than anywhere else in ophthalmology—ideas, interaction and inspiration thrive.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals.
Dr. Abelson would like to thank the following staff at ORA for their contribution to this article: Anti-infective/Anti-inflammatory—Aron Shapiro, director; Dry Eye—George Ousler, director, and Russ Anderson, research associate; Allergy—Paul Gomes, director, and Ingrid Lapsa, research associate; Basic Science—Keith Lane, danager, and Akimitsu Makino, research associate; AMD— Mark Thomson, danager; Medical Writing—Annie Plumer and Lisa Lines.