AMO Catalys
Users of the Catalys were recently given a new option for planning their intrastromal incisions in the form of a website, femtoemulsification.com, developed by London surgeon Julian Stevens and based on his personal nomogram.
“With these intrastromal incisions—which I like to call cylinders—there’s no risk of infection and there’s a very fast visual recovery and healing compared to manual incisions,” Dr. Stevens says. “Stabilization of the vision is much quicker, and by a month it’s actually not bad.
|
One of the general limitations of these intrastromal incisions is that they don’t achieve the same magnitude of effect as a similar-sized incision that breaches the surface. “A new nomogram needed to be built,” says Dr. Stevens. “For this nomogram, I lifted my original nomogram for intrastromal femtosecond incisions with the IntraLase and fed it into the system, creating version 1 nomogram for the Catalys. I then used my results to build version 2, then the current version 3.”
To use the website, you enter in data in the fields provided, such as the amount and axis of the preop astigmatism the location and length of your usual entry wound and how much astigmatism it induces, and the nomogram will generate the length of two symmetric arcs and the meridian on which they should be made. On the laser, the cylindrical incisions are placed in a space between 20 and 80 percent of the corneal depth, at an 8-mm zone, based on optical coherence tomography of the Catalys. You also have to adjust the laser’s setting beforehand for optimal results. “You deliberately increase the power of the laser during the intrastromal application,” explains Dr. Stevens. “That creates extra gas in the cornea that separates the cylinder’s edges. This is quite important because if there are any extra bridges of tissue the cylinder won’t open fully and achieve its effect. Some patients’ eyes are quite kinetic and of course there are always micro-movements that can result in some tissue bridges.” Dr. Stevens says the current intrastromal nomogram generates a mean vector magnitude of correction of 83 percent of the intended amount, up to a maximum of 2.5 D. He says the incisions achieve greater effect in the elderly and less in younger patients. In fact, the website will display a warning when the data is entered for a younger patient, informing the surgeon that the procedure may not achieve the entire amount of correction.
Since the initial version of the software is based on his work with the IntraLase, Dr. Stevens says the nomogram can also be transferred to that device. “With the IntraLase, you use an OCT ahead of time and then program the laser from a percentage depth approach,” he says. “The difference is you have to manually enter the planning into the IntraLase screens. It’s quite a bit of typing. Also, it’s important to scrutinize the screen marked ‘Review’ on the IntraLase to make sure you didn’t put in any incorrect values.”
Alcon LenSx
Users of the LenSx are also creating intrastromal astigmatic incisions, and are refining their nomograms.
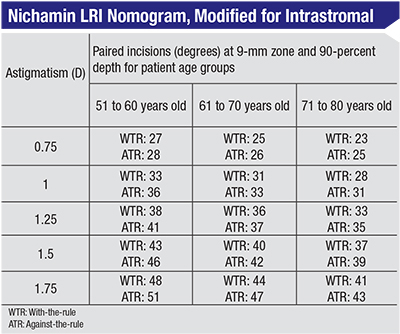
Jeffrey Wipfli, MD, of St. Luke’s Eye Center in Tampa, Fla., has hit upon an approach that’s been working well for him. “We use the AMO LRI calculator and I’ve been using the Nichamin nomogram,” he explains. “I used to initially open all of my LRIs right off the bat in the OR. I didn’t find that it made a huge difference so I stopped doing that. So, in some ways, you could call it intrastromal in that we’re not breaking through the epithelium. I aim for 80 percent of what the nomogram recommends based on the work of Eric Donnenfeld and the fact that the incisions are more central than the LRIs we would do before. I use a 9-mm optical zone. The length and depth are a lot more accurate, so to prevent overcorrections we were shooting for about 80 percent of what was predicted by the nomogram. I’ve adjusted the nomogram slightly, based on the posterior corneal astigmatism issue that has come up with toric lens implants, because I found I was not quite getting as much treatment effect as I would have liked. What I’m doing now is shooting for about 90 percent when the astigmatism is against-the-rule, but I’m still doing 80 percent in patients who have oblique or with-the-rule astigmatism.” He says he programs the laser’s OCT to start creating the incisions at 90 percent of the corneal depth.
Dr. Wipfli says one of the benefits of the intrastromal incision approach is that if there’s an undercorrection postoperatively, he’s still got a few options. “I wait a week postop to see what the effect is,” he says. “If it appears that the patient is undercorrected, then I’ll take a small Slade spatula and open the incisions at the slit lamp. This can get between a 0.25- and
0.5-D boost. It’s rare that I need to do that, however.”
Dr. Wipfli says a challenge with intrastromal incisions in general is avoiding intersecting the cataract entry wound or the paracentesis. “I try to create paired incisions, if possible, without having to adjust my main incision or my paracentesis,” he says. “If it looks like I will bisect one of my other incisions, I’ll do a single LRI, up to a 45 degree arc length. I did a longer incision once, 60 degrees, that caused some irregular astigmatism and overcorrection, so 45 degrees is as long as I will go. If the patient needs any more correction later, I can either open it at the slit lamp or add a second one manually and pair it with the other.”
In terms of the maximum amount of correction, Dr. Wipfli says he thinks surgeons could get up to 2 D with paired limbal relaxing incisions, but that he typically doesn’t do that. “For between 1 and 1.5 D of preop astigmatism, I’ll usually choose between a toric lens or a LenSx LRI depending on the axis of the astigmatism,” he says. “However, I feel comfortable with up to about 1 D with against-the-rule and a little bit more—1.25 D—with with-the-rule with the LenSx. So over 1.5 D I’ll usually use a toric lens. I think that is more accurate and reproducible.”
B + L Victus
London surgeon Sheraz Daya says the Victus femtosecond laser can also create intrastromal cuts, as long as you know how to set it up.
|
Overall, Dr. Daya says that, though there are some purported advantages to intrastromal astigmatism treatment, he currently leans more toward creating more conventional incisions that break the surface. “With intrastromal, you’re not breaking through Bowman’s, you have no incisions that can cause patients discomfort and, theoretically, there is no risk for corneal infiltrates or epithelial breakdown,” he says. “I haven’t seen any infiltrates or breakdown with other femtosecond incisions that open on the surface, though. I have had some open astigmatic keratotomy incisions that went on to be overcorrected and which I’ve had to suture, which is a situation you’d avoid with intrastromal cuts.
“However, I’ve done intrastromal incisions at a 7-mm optical zone in corneal graft patients,” Dr. Daya continues. “And I’ve experienced a lot of instability with them. Initially they wouldn’t get any effect, and then the patient would come back six months later not being able to see well. It would turn out they had
4 D of correction. For me, I find non-intrastromal LRIs more stable.”
LensAR
Manila, Philippines, surgeon Harvey Uy says the femtosecond LRI nomograms for non-intrastromal incisions developed by Louis Nichamin, MD, have served LensAR users well thus far when they attempt intrastromal cuts.
Even though conventional wisdom holds that you get less of an effect with an intrastromal cut if you use a nomogram meant for a normal, surface incision, Dr. Uy says it actually fits his approach to treating astigmatism. “I follow the same nomogram because, in general, I’d rather be undercorrected than overcorrected,” he says. “The nomogram is based on 90-percent depth and a 9-mm optical zone. The LensAR system will measure the corneal thickness and then the software will automatically set it to begin the incision at 90-percent depth. You can change the setting to other depths, as well as alter the optical zone, however. We like the 9-mm zone because it’s farther from the visual axis.”
Though the depth, optical zone and cutting are automated, Dr. Uy says the surgeon has to use his manual skills to get the axis correct. “Now, we basically put a reference mark on the eye,” he says. “You also have a reference mark on the patient interface. You align the two marks, then do the imaging and pre-program the incision locations. Though it works, it is subject to some errors when marking the reference points. You’ll probably be off by a few degrees, which can lead to suboptimal astigmatic correction in some cases. However, LensAR is currently developing new iris registration software so that a diagnostic machine will capture an image of the patient’s eye preoperatively. The image of the eye will be sent to the femtosecond laser to let it determine the correct treatment axis.”
In terms of correction, Dr. Uy says he can treat up to 3 D of preoperative cylinder with these intrastromal incisions. “However, if someone has over 1.5 D, we encourage him to get a toric intraocular lens,” he says. “Even so, there will be some patients who get the toric lens but whose astigmatism still exceeds the power of the IOL. In those cases, we’ll use the arcuate incision to supplement the toric IOL and correct larger amounts of astigmatism.”
Dr. Uy says one aspect of intrastromal femtosecond incisions he likes is the titratability in cases of undercorrection. “The disadvantage of an incision that opens is you may overcorrect the astigmatism and you can’t really undo it,” he says. “Whereas if you do intrastromal and you’re undercorrected, you can still open it up after the surgery and titrate the correction. The percentage of patients in my practice who need to have the incisions opened later on is about 10 to 15 percent. I’ve found that patients are generally happy after the procedure. It’s the patients who get multifocal lenses who are a bit more particular about correcting their astigmatism.”
Dr. Uy says that, though intrastromal ablations take a bit more customization to perform, they have their uses. “I think it’s a very safe procedure,” he says. “We haven’t had any complications from it, and haven’t seen any perforations. If a surgeon has a femtosecond laser, I’d encourage him or her to use this particular feature.” REVIEW