THE MAJORITY OF WHAT RETINA SPECIALISTS DO FOR PATIENTS is directed at improving the quality of life, not the quantity of life. Certainly, ophthalmologists "save lives" by diagnosing malignancies, detecting neurologic and vascular emergencies, and noting ocular manifestations of life-threatening systemic disease. Yet the treatment of macular degeneration, retinovascular disease, retinal detachment and other common retinal conditions has a much greater impact on how, rather than how long, patients live their lives.
So why do we need to measure quality of life? Certainly, for any disease or treatment to be evaluated properly, its impact should be studied. The field of ophthalmology enjoys many biometric measures, such as visual acuity, intraocular pressure, retinal thickness, etc. But while a measurement such as best-corrected visual acuity may be both objective and accurate in assessing macular function, it does not adequately describe the impact retinal disease has on a patient's quality of life, or on a patient's ability to undertake activities of daily living.1
A significant volume of recent ophthalmic literature has been devoted to the measurement of health-related quality of life (HRQOL), particularly in anterior segment disease and glaucoma.2-9 Outcomes research in patient-assessed quality of life for posterior segment disease, however, has lagged behind. In fact, as noted in a recent publication of the Submacular Surgery Trials Group, "None of the randomized clinical trials in age-related macular degeneration reported to date has included an assessment of patient perceptions of the influence of their vision on health-related quality of life."10
HRQOL: What It Is, Why It's Important
Health-related quality of life is how a person's own health affects his satisfaction with and enjoyment of life, including physical, psychological, and social functioning. HRQOL offers information that is complementary to other biophysical measures in evaluating the impact of disease on a patient.
HRQOL is important at many different levels in the health-care system. For a patient and his or her family, being informed about the effect that a disease may have on one's life is crucial for coping with the disease in the present and knowing what to expect in the future. HRQOL information can have a big impact on a physician's clinical decision-making process in weighing and communicating the risks and benefits of various treatments and placing a patient's eye disease in perspective to the background of their overall health. Hospitals and health-care organizations are increasingly turning to HRQOL data to determine where to focus their efforts. Quantitating a disease-associated HRQOL is a prerequisite for cost-effectiveness analysis. At the governmental and societal levels, HRQOL and cost-effectiveness data have a tremendous impact in deciding reimbursement levels, appropriating research dollars, and otherwise allocating resources.
Studies commonly measure HRQOL by means of a utility value. Utility values in ophthalmology are usually highly correlated with the acuity of the better-seeing eye.
Utility Value Defined
Utility theory addresses making rational decisions based on uncertainty in data. Utility theory in health-care sprang from economic theories introduced by John von Neumann and Oskar Morganstern in 1944. The application of utility theory to health care began in the 1980s to quantify the uncertainty concerning screening of populations for various diseases, prognostic factors and interventions.11
A utility value is a numerical measure of an individual's health state. By convention, perfect health is assigned a value of 1.0 and death is assigned a value of 0.0. By various methods that will be described shortly, patients may assign their current health state a value from 0 to 1. Utility values can also be used to calculate a single weighted measure of health status combined with life expectancy, or the quality-adjusted-life-year. The QALY may be divided into health-care costs in determining costs per QALY, the basis of cost-effectiveness analysis.
How We Measure Utility
There are several methods to measure health state preferences. Four of the methods more commonly used are the standard gamble, time trade-off, willingness-to-pay, and rating scale methods.12
The standard gamble method asks a patient if he or she would prefer a specific health state, or take a certain risk of a worse health state in hopes of achieving an improved health state. For example, suppose a new surgical device can be implanted to cure Parkinson's disease, but the surgery is associated with a 10-percent mortality rate. Would patients with Parkinson's disease accept a 10-percent risk of death (undesirable health state) in order to return to health (desirable health state)? By posing such a question to numerous patients with Parkinson's disease, and adjusting the risk percentage appropriately, one could arrive at a statistically valid utility value for living with Parkinson's disease, or a HRQOL measure in patients with Parkinson's disease.
The time trade-off method asks a patient how much of his life expectancy would he give up for a better health state? For instance, if a patient with end-stage renal disease on chronic hemodialysis therapy had a life expectancy of 10 years, how many of those years would he give up to live with perfect health?
The willingness-to-pay technique asks subjects to evaluate their health state in monetary terms. For instance, a question posed could be, "What percentage of your household income would you be willing to pay per year for a complete cure of your arthritis?" By asking for a portion of total income rather than a specific dollar value, differences in socioeconomic status among patients are minimized.
Rating scale methods present patients with a graphical or numeric scale on which to rate their health state. For instance, patients with HIV/AIDS might be asked to place a mark on a line from 0 (death) to 100 (perfect health) describing how they feel about the quality of their lives as related to health.
Several vision-specific HRQOL have been introduced over the years. The Activities of Daily Living Scale (ADLS), 20-item metric,13 and the Visual Activities Questionnaire, both introduced in 1992, were early attempts to quantify HRQOL in ophthalmic studies. However, several subsequent questionnaires have largely supplanted these metrics.
The Visual Functioning Index (VF-14) is a functional assessment consisting of 14 questions designed to elicit how a person functions with his current vision. This metric was initially developed for patients with cataract in 1994,14 but has been applied in other settings. An example of one question is, "Do you have any difficulty, even with glasses: Reading small print such as labels on medicine bottles, a telephone book, food labels? Taking part in sports like bowling, handball, tennis, golf?" Respondents who answer affirmatively must then rate the difficulty as either: "a little," "a moderate amount," "a great deal," or "unable to do the activity." The VF-14 was first validated for patients with retinal disease in 1999.15 The VF-14 does address functional limitations, including driving and other activities of daily living. However, it does not specifically elicit how the visual decline affects a patient's overall sense of well being.
The National Eye Institute Visual Function Questionnaire (NEI-VFQ) investigates visual functional limitations as well as how they impacts a patient's overall social and emotional functioning. This 51-item metric was validated in 1998 on patients with cataract, macular degeneration, diabetic retinopathy, glaucoma, cytomegalovirus retinitis, and low vision. The areas tested (number of questions) were: general health (2); general vision (2); ocular pain (2); near vision (7); distance vision (7); vision-specific social functioning (4); vision-specific mental health (8); expectations for visual function (3); vision-specific role functioning (5); dependency due to vision (5); driving (4); peripheral vision (1); and color vision (1).16 This comprehensive metric is commonly employed in large ophthalmic trials. One drawback is that questionnaires with numerous items can be unwieldy, time-consuming, and expensive to administer in studies.
With an intent to streamline the 51-item NEI-VFQ, a shorter version, the 25-Item National Eye Institute Visual Function Questionnaire (NEI-VFQ-25), was validated in 2001. This shorter version can be administered in five minutes. The areas tested (number of questions) are: general health (1); general vision (1); near vision (3); distance vision (3); driving (1); peripheral vision (1); color vision (1); ocular pain (2); and vision-specific questions, which included mental health and social functioning (11).17
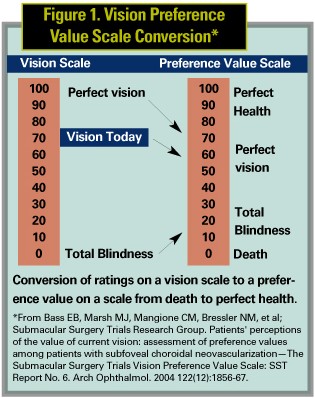
The Vision Preference Value Scale (VPVS) was introduced in 2004 in the Submacular Surgery Trials. The rating-scale technique was chosen for the VPVS owing to high test-retest reliability and good internal consistency, even in the absence of visual aids or an in-person interview. This metric consists of three questions and can be administered over the telephone. Patients are asked to rate their overall quality of life supposing they have their current health and perfect vision on a scale from 0 (death) to 100 (perfect health with perfect vision). Using the same scale, patients are asked to rate quality of life supposing they have their current health but complete blindness. Lastly, on a different scale, patients are asked to rate their current vision on a scale from 0 (blindness) to 100 (perfect vision). A simple calculation from the answers to these three questions yields a "preference value" or utility measure of the patient's overall quality of life.18
The results of numerous studies of patients with retinal disease that include vision-specific HRQOL measures indicate that visual impairment has a profound effect on quality of life. For instance, in one study patients with diabetic retinopathy and those with age-related macular degeneration were willing to give up three years of every remaining decade of life for perfect vision. Those with legal blindness would give up four years off every decade, and patients with "complete blindness" would give up three-quarters of their remaining lives for perfect vision.19 The Submacular Surgery Trials, which introduced the VPVS, revealed that patients with vision loss from choroidal neovascularization exhibited a mean preference value of 0.64. This indicates how profound an effect vision loss from CNV has on quality of life when compared with preference values for congestive heart failure (0.77), AIDS (0.65), chronic renal failure requiring dialysis (0.54), and major stroke (0.30).20
In deciding how to interpret future studies with HRQOL measures included, Sanjay Sharma and colleagues propose a framework. The reader of a study should ask if the HRQOL measurement is necessary, if the results are valid, what the results are, and how they can be applied.21
| Figure 2. Critical Appraisal Framework for a HRQOL Paper* |
| I. Is a HRQOL measurement necessary? II. Are the results valid? |
| a. Are all items important to patients? |
| b. Are all relevant aspects being measured? |
| c. Does the instrument appear to measure what is intended? |
| d. Are there logical relationships between questionnaire scores and other measures? |
| e. What kinds of inferences can be made about the HRQOL measurements? |
| III. What are the results? |
| a. Is the observed effect significant? |
| b. Is the observed effect important? |
| IV. How can these results be applied? |
| a. Can these results be generalized to clinical practice? |
| b. Can these results help the patient make a decision? |
| * From Sharma S, Oliver-Fernandez A. Age-related macular degeneration and quality of life: how to interpret a research paper in health-related quality of life. Curr Opin Ophthalmol 2004;15(3):227-31. |
Health-related quality of life is increasingly recognized as an important outcome that provides information complementary to physical measures, such as visual acuity. Patients and their physicians will be better educated about disease and make more informed treatment decisions with consideration of HRQOL data.
This manuscript was supported by the Heed Foundation (HFF) and the Macula Foundation Inc. Dr. Fine has no financial interest in the topics discussed. He is a fellow in vitreoretinal surgery at Columbia University College of Physicians and Surgeons; 460 Park Avenue, Fifth Floor, New York, NY 10022. Contact him at (212) 861-9797, fax (561) 828-0784, or e-mail h_f_fine@yahoo.com. Dr. Chang is a resident at Wilmer Eye Institute, Johns Hopkins Medical Institute, Baltimore.
1. Sharma S, Brown GC, Brown MM, et al. Converting visual acuity to utilities. Can J Ophthalmol 2000 Aug;35(5):267-72.
2. McDonnell PJ, Mangione C, Lee P, Lindblad AS, et al. Responsiveness of the National Eye Institute Refractive Error Quality of Life instrument to surgical correction of refractive error. Ophthalmology 2003 110(12):2302-9.
3. Hays RD, Mangione CM, Ellwein L, Lindblad AS, et al. Psychometric properties of the National Eye Institute-Refractive Error Quality of Life instrument. Ophthalmology 2003 110(12):2292-301.
4. Chia EM, Wang JJ, Rochtchina E, Smith W, et al. Impact of bilateral visual impairment on health-related quality of life: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci 2004 45(1):71-6.
5. Busbee BG, Brown MM, Brown GC, Sharma S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology 2003 110(12):2310-7.
6. Feiner L, Piltz-Seymour JR; Collaborative Initial Glaucoma Treatment Study. Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol 2003 14(2):106-11.
7. Donovan JL, Brookes ST, Laidlaw DA, Hopper CD, et al. The development and validation of a questionnaire to assess visual symptoms/dysfunction and impact on quality of life in cataract patients: The Visual Symptoms and Quality of Llife (VSQ) Questionnaire. Ophthalmic Epidemiol 2003 10(1):49-65.
8. Prager TC, Chuang AZ, Slater CH, Glasser JH, Ruiz RS. The Houston Vision Assessment Test (HVAT): an assessment of validity. The Cataract Outcome Study Group. Ophthalmic Epidemiol 2000 7(2):87-102.
9. Boisjoly H, Gresset J, Fontaine N, Charest M, et al. The VF-14 index of functional visual impairment in candidates for a corneal graft. Am J Ophthalmol 1999 128(1):38-44.
10. Submacular surgery trials randomized pilot trial of laser photocoagulation versus surgery for recurrent choroidal neovascularization secondary to age-related macular degeneration: II. Quality of life outcomes submacular surgery trials pilot study report number 2. Am J Ophthalmol 2000 130(4):408-18.
11. Sharma S, Brown GC, Brown MM, Shah GK, et al. Converting visual acuity to utilities. Can J Ophthalmol 2000 35(5):267-72.
12. Froberg DG, Kane RL. Methodology for measuring health-state preferences--II: Scaling methods. J Clin Epidemiol 1989;42(5):459-71.
13. Mangione CM, Phillips RS, Seddon JM, Lawrence MG. Development of the 'Activities of Daily Vision Scale'. A measure of visual functional status. Med Care 1992 30(12):1111-26
14. Steinberg EP, Tielsch JM, Schein OD, Javitt JC, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol 1994 112(5):630-8.
15. Linder M, Chang TS, Scott IU, Hay D. Validity of the visual function index (VF-14) in patients with retinal disease. Arch Ophthalmol 1999 117(12):1611-6.
16. Mangione CM, Lee PP, Pitts J, Gutierrez P, et al. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol 1998 116(11):1496-504.
17. Mangione CM, Lee PP, Gutierrez PR, Spritzer K, et al. National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 2001 119(7):1050-8.
18. Bass EB, Marsh MJ, Mangione CM, Bressler NM, et al; Submacular Surgery Trials Research Group. Patients' perceptions of the value of current vision: assessment of preference values among patients with subfoveal choroidal neovascularization—The Submacular Surgery Trials Vision Preference Value Scale: SST Report No. 6. Arch Ophthalmol 2004 122(12):1856-67.
19. Sharma S, Brown GC, Brown MM, Shah GK, et al. Converting visual acuity to utilities. Can J Ophthalmol 2000 35(5):267-72.
20. Bass EB, Marsh MJ, Mangione CM, Bressler NM, et al; Submacular Surgery Trials Research Group. Patients' perceptions of the value of current vision: assessment of preference values among patients with subfoveal choroidal neovascularization—The Submacular Surgery Trials Vision Preference Value Scale: SST Report No. 6. Arch Ophthalmol 2004 122(12):1856-67.
21. Sharma S, Oliver-Fernandez A. Age-related macular degeneration and quality of life: how to interpret a research paper in health-related quality of life. Curr Opin Ophthalmol 2004 15(3):227-31.



