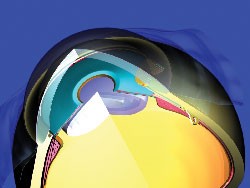
One that appears to hold much promise is the DeepLight Glaucoma Treatment System, developed by Solx in Boston. This is the first treatment system to include both a laser (titanium-sapphire) and a photo-titratable gold micro-shunt. The two components are designed to be used separately or together, thus providing three complimentary treatment options: repeatable trabeculoplasty using the laser, implantation of the shunt to expedite aqueous outflow, and laser titration of the shunt at any time after implantation to open extra drainage channels (initially held in reserve).
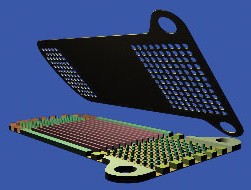  |
| Solx's DeepLight Gold Micro-Shunt implant contains multiple micro-channels that increase outflow without a bleb. Some channels are initially held in reserve; they can be opened later using the DeepLight laser. |
Each option has unique aspects that set it apart from currently available treatments.
The DeepLight titanium-sapphire laser is a flashlamp-excited, solid-state laser that emits near-infrared light (790 nm) in pulses lasting five to 10 microseconds. It's been in development for the past four years at the Boston University Photonics Center; it's currently available in Europe, Canada and the Middle East.
 |
| The DeepLight titanium-sapphire laser can be used to perform trabeculoplasty without causing coagulative tissue damage. |
In one ongoing pilot study, 68 eyes of 57 patients were treated. Data for the 38 eyes that have been followed for 18 months show:
• IOP was reduced from 21 to 29 percent compared to medication alone.
• Use of medication decreased by two-thirds or more.
• Patients in the pilot study who were on a single medication before laser treatment were using no medications after 18 months; of all patients in the study, 50 percent became medication-free.
• Retreated patients' IOPs decreased 26 percent from medicated levels.
• Patients who had had prior ALT dropped 28 percent from medicated IOP levels and reduced medication use 75 percent.
• No patient was worse following treatment.
Another randomized, controlled study at the Goldschleger Eye Institute in Tel-Hashomer, Israel, compared trabeculoplasty done using the DeepLight laser with traditional ALT. The DeepLight laser induced significantly less tissue damage than argon trabeculoplasty.
Shlomo Melamed, MD, who practices in Tel Aviv and has conducted several studies using the laser and micro-shunt, is conducting a randomized, masked study comparing the titanium-sapphire laser procedure to ALT; his first 40 cases have more than six months of follow-up.
"In the titanium-sapphire laser group," he says, "the pressure in many eyes goes down within one hour, dropping below the ALT eyes' pressure. We believe this is because this laser affects deeper layers of tissue. However, at one month, the pressure in the two groups is very similar. Then, at three and six months the titanium laser patients are better.
"After treatment," he says, "there's no peripheral anterior synechiae formation, necrotic signs or scar formation, and we've seen no serious complications. Only a few patients had a pressure spike after the treatment, which subsided within 24 hours. Patients don't complain of pain or discomfort, which is amazing considering the high level of energy being used." According to Solx, a study starting this summer will compare this procedure to SLT.
Solx describes the biocompatible, 24-karat gold micro-shunt as a departure from standard shunts and valves. Instead of a tube, the shunt is a flat plate 5.2-mm long, 2-mm wide and 60-µm thick, containing multiple microchannels. Initially, about half are open; the remainder can be opened after implantation, using the laser.
The micro-shunt is designed for subscleral implantation through a single incision made at the limbus; once inserted in the eye (using a special preloaded insertion device) it can't be felt by the patient, and is only visible if the eyelid is raised. It's placed to form a bridge between the anterior chamber and supraciliary space, so no filtering bleb is created.
|
|
| The DeepLight gold micro-shunt creates a bridge between the supraciliary space and the anterior chamber. Insertion is a 2.5-mm single-incision procedure. |
|
|
| The DeepLight gold micro-shunt creates a bridge between the supraciliary space and the anterior chamber. Insertion is a 2.5-mm single-incision procedure. |
Several pilot studies have been conducted using the gold micro-shunt to reduce IOP. In one study conducted in Barcelona and Madrid, Spain, the micro-shunt was implanted in 47 eyes of 47 patients, who were followed from baseline to 18 months. Mean IOP decreased from 27.5 to 17.4 mmHg, and the average number of required medications decreased from 3.3 to 1.2.
According to Solx, a second pilot study, conducted in Spain and Israel, is following 57 eyes; seven have now been followed for two years. "The patients in the study were all on failed maximal medical therapy, plus one failed surgical trabeculectomy," explains Douglas Adams, president and CEO of Solx. "The data showed a mean IOP of about 29 mmHg before implantation. Eighteen months after implantation, the mean IOP was 18.38, about a 37-percent change, and this was accompanied by a reduction in mean medication use as well. We saw no significant deviation in mean IOP from one to 24 months, something that would not be expected with trabeculectomy." Solx is conducting a study comparing the gold micro-shunt to other shunts, including the Express and the Ahmed valve. Results may be published later this summer.
The company hopes that the gold micro-shunt will eventually replace trabeculectomy.
Titrating the Shunt
As a third option, the titanium-sapphire laser can be used to photo-titrate the gold micro-shunt, selectively opening pre-existing microtubular channels to increase the amount of outflow. "This is a new concept," observes Dr. Melamed. "The gold has a maximum absorption curve at 790 nm, which is the wavelength of the titanium-sapphire laser. If some channels are clogged after one or two years, you can open extra channels that are still closed by a thin film of gold and reactivate the shunt."
Mr. Adams says that the company is beginning a study of the titration capability now. "We've opened up four or five extra channels in the gold micro-shunt in five eyes that reached 12-month follow-up," he says. "The eyes averaged an additional drop of 5 mm from the new baseline. However, this is short-term data."
Dr. Melamed has only tried this once, in a difficult case, and notes that eventually the extra channels also closed. "We still don't know a lot about the capacity of the healing processes that take place in the supraciliary space," he admits. "We're learning as we go."
Off and Running
Solx has two major clinical studies of the system getting under way; the company plans to enroll up to 500 eyes in each study. Currently the DeepLight Gold Micro-Shunt is pending CE clearance.
More information can be found online at Solx.com.