Because ocular surface conditions such as dry eye can affect patients’ outcomes after cataract or refractive surgery, it’s important to establish a healthy ocular surface preoperatively. Notably, the recent PHACO study found that the incidence of dry eye in patients scheduled to undergo cataract surgery was higher than anticipated.1
This prospective, multicenter, observational study included 136 patients who were at least 55 years old and were scheduled to undergo cataract surgery. Patients’ mean age was 70.7 years. Most were Caucasian (73.5 percent), and half were women. Almost 60 percent had never complained of foreign body sensation. Most patients (62.9 percent) had a tear breakup time of five seconds or less, and 77 percent had positive corneal staining. Half of the eyes had positive central corneal staining, and 18 percent had a Schirmer’s score with anesthesia of 5 mm or less. These findings were definitely not what was anticipated in the standard cataract patient population that presents routinely to the office.
According to Robert Latkany, MD, who is in practice in New York City, preparing the ocular surface for cataract or refractive surgery requires a customized approach for each patient. “If you neglect the ocular surface in patients undergoing cataract or refractive surgery, outcomes will be compromised, and you will have fewer happy patients,” he says. “However, the drying effects of cataract surgery are not nearly as devastating or detrimental to the ocular surface as refractive surgery. So, I’d probably be a lot more aggressive in the refractive surgery patient than in the cataract patient. Unfortunately, there is no cookbook answer. I look at the eye and the anatomy and listen to patients’ complaints, and then I determine what I can do to ensure the best possible outcome.”
According to John Sheppard, MD, who is in practice in Norfolk, Virginia, the main difference between
Edward Manche, MD, who is in practice at Stanford University, agrees. “Cataract patients are often significantly older than refractive patients, often by several decades,” he says. “From that standpoint, treatment may be a bit different, but you still approach them with the same philosophy. However, older patients often have issues that a younger person might not have.”
Preoperative Management
According to Karl Stonecipher, MD, who is in practice in Greensboro, North Carolina, the ocular surface disease index is still a great screening tool for dry eye. “We put it out in our waiting area, and it’s part of our intake form,” he says. “If a patient scores in the normal range, we move on. If he or she scores mild, moderate or severe, it behooves us, whether it’s a cataract or refractive patient, to move to the next level. I’ve empowered my staff to do two simple things: tear breakup time and corneal staining. They’re trained to read and put into my EMR a staining pattern with fluorescein, a tear breakup time or a lissamine green stain.”
Dr. Stonecipher says that diagnosis is
According to Dr. Stonecipher, if a refractive surgery patient is severely dry, you may want to consider only operating on him or her during the summer, when there are higher humidity levels. Alternatively, patients can try cyclosporine or
For younger refractive surgery patients, Dr. Stonecipher also is investigating the use of Epic Treatment (Espansione, Italy), which is a combination of intense pulsed light and low-level light therapy. It simultaneously treats the lower and upper eyelids with direct and indirect applications. The company claims it improves dry-eye symptoms after a few hours, as a result of the synergy of the two technologies helping meibomian glands resume production of the necessary lipids. “Although the mechanism of action is still debated, IPL primarily opens, heats and stretches the glands,” says Dr. Stonecipher. “The nice thing about the Epic System is that it’s a
Dr. Stonecipher also expresses patients’ meibomian glands. “I have also just started to use TempSure (Hologic), which uses radiofrequency to heat the glands, [which is a treatment] for the more resistant patients who are not responding to the Epic system,” he explains.
Patients who continue to be resistant then undergo LipiFlow (TearScience) treatments. “We have a tier system because it’s all out-of-pocket. The cost is a little less for Epic versus TempSure versus LipiFlow. I think all of these systems have their pluses and minuses, but insurance doesn’t pay for any of this, which is an issue. LipiFlow costs, on average, $1,000 to $1,500 per treatment of both eyes, while the others are between $350 and $550 per bilateral treatment,” he notes.
IPL combined with meibomian gland expression has been found to safely and effectively treat meibomian gland dysfunction, according to a study that was published this summer.2 The prospective, randomized,
According to Dr. Sheppard, surgeons need to consider the ocular surface unit as a whole and look for more than
Dr. Sheppard also assesses the patient for blepharitis and allergy. “Those tend to be either confused with dry eye or ignored in the presence of dry eye as a contributory condition,” he adds.
He notes that 75 percent of his patients presenting for cataract surgery have dry eye or a combination of ocular surface conditions that manifest as dry eye. “We create an intervention, and then we look to see that the critical central corneal epithelium is optically acceptable, clear and regular. We do that by confirming topographies,
Postoperative Management
Some patients continue to experience or develop dry-eye symptoms after surgery. Dr. Stonecipher says that he sees five or six patients a month who have undiagnosed dry-eye disease post premium IOL or refractive surgery and who are extremely unhappy with their surgical outcome. “Most of the patients who come to see me for refractive surgery are young patients who have meibomian gland disease because they’re staring at their computers and phones all day,” he says. “I’m seeing increasing numbers of patients with severe evaporative dry eye, which is leading to their contact lens wear being compromised. Of my LASIK volume each month, approximately 20 to 30 percent of my patients fall into that category. That’s a significant number, and if I operate on those patients and make their problem worse, even if it’s temporary, it’s my problem and not their problem anymore. However, if you tune them up before surgery, you will have fewer unhappy patients.”
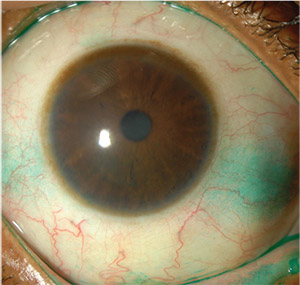 |
| Training staff to read staining patterns can help the surgeon quickly identify ocular surface problems preop, experts say. Photo by Christopher Rapuano, MD |
Dr. Sheppard adds that it’s important to remember that any surgical procedure worsens existing ocular surface disease or can create new ocular surface disease. “When patients have no idea that there were abnormalities present prior to cataract surgery and then suddenly they arise, a very difficult discussion ensues,” he says. “Therefore, warn patients about their pre-existing ocular surface conditions. Postoperatively, we definitely trigger more ocular surface disease and dry eyes because of the incisions, the lights and the microscope, the speculum holding the eye wide open, and all the medicines that patients are using.”
According to Dr. Manche, many cases of dry eye resolve on their own after refractive surgery. “Dry eye generally tends to get better on its own over time following
These surgeons agree that managing patient expectations is the key to a successful surgical outcome. According to Dr. Latkany, patients need to be
The Future
Dr. Sheppard notes that we live in an interesting time for treating dry eye. “It’s a truly exciting field that we’re experiencing,” he says. “Twenty years ago, dry eye was neglected and, if considered at all, treated only with tear supplements. Now, we understand that a variety of factors contribute to ocular surface disease and dryness, and we can treat our patients with genuinely targeted intent,” he says.
Drs. Latkany, Sheppard
1. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The prospective health assessment of cataract patients’ ocular surface (PHACO): The effect of dry eye. Clin Ophthalmol 2017;11:1423-1430.
2. Rong B, Tang Y, Tu P, et al. Intense pulsed light applied directly on eyelids combined with meibomian gland expression to treat meibomian gland dysfunction. Photomed Laser Surg 2018;36:6:326-332.



