Howard F. Fine, MD,
Wei Wei Nabil Simaan, PhD,
Ophthalmic surgery, and in particular vitreoretinal surgery, is a technology-driven field. A majority of recent advances in retina surgery are owed in large part to engineers, such as small-gauge instrumentation, high-speed cutters, panoramic visualization systems and wide-field illumination probes, to name a few.1 Could robot-assisted surgery represent an upcoming revolution in our field?
Advantages of Surgical Robots
The introduction of robots into the operating room has been a paradigm shift for many of our surgical colleagues in other fields, such as laparoscopic surgery, urology, gynecologic surgery, orthopedics, neurosurgery and others. Adoption is growing at a rapid pace. For example, estimates suggest that 80 percent of radical prostatectomies in the
Robots may offer a number of specific advantages over unaided human hands. Scaling of motion allows robots to make extremely precise movements. Tremor filtration can correct an inherent human limitation. Dexterity in confined anatomic spaces can be enhanced, as can maneuverability without direct visualization.3 Robots can shield surgeons from harmful exposures, and tele-operation of robotic systems could afford patients access to specialized procedures without necessitating travel.4
In fact, all of these goals have already been achieved in humans. The most commonly employed surgical robot to date is the da Vinci Surgical System (Intuitive Surgical, See Figure 1). The surgeon is seated at a console ("master") viewing stereoscopic images from an endoscopic camera and controlling the robotic arms ("slave"), which can accommodate a variety of instruments.5 Other examples include the Sansei X Robotic Catheter System (Hansen Medical) which allows cardiac electrophysiologists to guide a catheter-based robot with great dexterity and without exposure to fluoroscopy,6 and the Robotic Arm Interactive Orthopedic System (Mako Surgical), capable of high-precision joint replacement and resurfacing based on preoperative CT scans.7
Disadvantages of Surgical Robots
Robots in the operating room also have a number of downsides. Currently, expense is a major limiting factor. The da Vinci Surgical System, for instance, costs well in excess of $1 million with annual maintenance/disposables costs that can reach hundreds of thousands of dollars. Setup time can be significantly longer with da Vinci-assisted cases (more than 20 minutes in some studies).8 This could represent a major impediment for applications in vitreoretinal surgery, which has taken great strides in efficiency over recent years. Lastly, there exists a learning curve associated with using new surgical tools, and surgical robots often present a challenge both for physicians and operating room support staff alike. Certainly retina surgeons need not worry about losing a job to robotic outsourcing any time in the foreseeable future.
Retinal Robots
Ophthalmic surgery and retina surgery in particular pose a number of unique challenges for robot development. First, the precision required is great: Membrane peeling and other techniques require tolerances on the order of microns, not millimeters. Second, the most commonly employed visualization techniques involve specialized lens systems particular to our field in conjunction with an operating microscope, although endoscopic visualization is used occasionally. Third, the pivot point (remote center of motion) differs in vitreoretinal surgery from typical laparoscopic surgery.
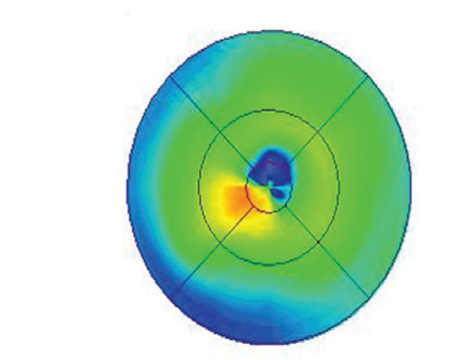
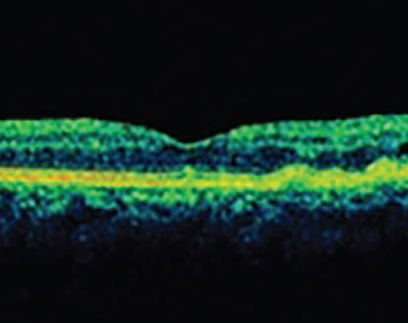
Several retina specialists have worked to introduce robotic systems for ophthalmic and/or retinal surgery. Eugene de Juan, MD, and colleagues developed a "steady-hand" robot capable of tremor filtration.9 Steve Charles, MD, and colleagues developed a telerobotic system for eye surgery.10 Dr. Charles founded and chairs MicroDexterity Systems, which is currently focused on orthopedics and neurosurgery.11 Angelo Tsirbas, MD, and colleagues utilized the da Vinci system to suture corneal lacerations in an animal model (See Figure 2).12 Takashi Ueta, MD, and colleagues have demonstrated vascular cannulation in an animal model (See Figure 3).13 Jean Pierre Hubschman, MD, and colleagues described a hexapod system that works in conjunction with the da Vinci robot.14 Our group designed a novel dual-arm ophthalmic surgical robot (See Figure 4) capable of high precision (<5 µm) and presented both vascular cannulation and stent deployment in animal models (See Figure 5).15
Adoption of Surgical Technology
What drives a surgical tool to be adopted? Merely reproducing what surgeons can already do well is unlikely to promote use of a robot for ophthalmic surgery. A "killer application" is required. For instance, the technology could enable surgeons to treat a condition that is currently untreatable. Significantly improving outcomes or lowering complication rates would also make a compelling argument.
Many lessons can be learned from the da Vinci experience. Before its introduction, many surgeons reacted with skepticism about the value of such a device: They were already able to perform all of the procedures for which they were trained, and their complications rates were acceptably low. Yet once the robot for laparoscopic surgery was approved by the Food and Drug Administration, the floodgates opened. Surgeons innovated, the list of indications treatable with robotic surgery rapidly expanded, and the number of cases performed with robotic assistance has increased exponentially.
Robot-assisted surgery has revolutionized many other surgical fields. While a number of obstacles exist for ophthalmic surgical robots, interest appears to be growing, as highlighted by a number of recent presentations and publications on the topic. Robotics for vitreoretinal surgery has the potential to expand our treatment armamentarium and reduce complication rates, and it holds the promise in the future to treat conditions that remain incurable today.
Dr. Fine is an assistant professor at
1. Bhatnagar P, Fine HF,
2. Orvieto MA, Patel VR. Evolution of robot-assisted radical prostatectomy. Scand J Surg. 2009;98(2):76-88.
3. Palep JH. Robotic assisted minimally invasive surgery. J Minim Access Surg. 2009 Jan;5(1):1-7.
4. Marescaux J, Leroy J, Rubino F, et al. Transcontinental robot-assisted remote telesurgery: Feasibility and potential applications. Ann Surg 2002;235:487–92.
5. http://www.davincisurgery.com
6. Saliba W, Reddy VY, Wazni O, et al. Atrial fibrillation ablation using a robotic catheter remote control system: Initial human experience and long-term follow-up results. J Am Coll Cardiol. 2008;24;51(25):2407-11.
7. Pearle AD, Kendoff D, Stueber V, et al. Perioperative management of unicompartmental knee arthroplasty using the MAKO robotic arm system (MAKOplasty). Am J Orthop (Belle
8. Iranmanesh P, Morel P, Wagner OJ, et al. Set-up and docking of the da Vinci((R)) surgical system: Prospective analysis of initial experience. Int J Med Robot. 2010 Jan 4. [Epub ahead of print]
9. Taylor R, Jensen P, Whitcomb L, et al. Steady-hand robotic system for microsurgical augmentation. International journal of robotics research. 1999 (18):1201.
10. Charles S, Das H, Ohm T, Boswell C, Rodriguez, Steele R, Istrade D. Dexterity-enhanced telerobotic microsurgery. ICAR 1997,
11. http://www.charles-retina.com
12. Tsirbas A, Mango C, Dutson E. Robotic ocular surgery. Br J Ophthalmol. 2007 Jan;91(1):18-21.
13. Ueta T, Yamaguchi Y, Shirakawa Y, et al. Robot-assisted vitreoretinal surgery: Development of a prototype and feasibility studies in an animal model. Ophthalmology. 2009 Aug;116(8):1538-43
14. Hubschman JP,
15. Fine HF, Simaan N, Wei W, et al. A novel dual-arm dexterous ophthalmic microsurgical robot: Applications for retinal vascular cannulation and stent deployment. Retina Congress, NY, October 2009.
16. Reprinted with permission from Tsirbas A, Mango C, Dutson E. Robotic ocular surgery. Br J Ophthalmol. 2007 Jan;91(1):18-21.
17. Reprinted with permission from Ueta T, Yamaguchi Y, Shirakawa Y, et al. Robot-assisted vitreoretinal surgery: Development of a prototype and feasibility studies in an animal model. Ophthalmology. 2009;116:1538-43.