Three factors have a profound impact on how successful a given patient will be at taking his medicine. The first factor is acceptance: If the patient doesn't accept that he has a problem that requires treatment, he won't take the medicine. The second factor is persistence: The patient has to continue to take the medicine—as directed—for the duration of the disease without losing interest, becoming distracted or letting the medicine run out. (Unfortunately, persistence tends to wane over time.) The third, less obvious issue is: Can the patient execute the administration of the drop—i.e., is the patient getting the correct dose into his eye?
Ironically, the last factor has received very little attention, despite the fact that eyedrops have been in use for more than 200 years. In recent years researchers have done elegant studies on everything from how many drops are contained in a bottle at various temperatures to what happens if you tilt the bottle at different angles. The U.S. Food and Drug Administration has worried about the plastic from the bottle leaching into the drops. These are all important issues, but hardly anyone has devoted much effort to one of the most important questions of all: Does this delivery method work in the patient's hands?
The Best of Intentions
To address this question, in one of our recent studies we enrolled 139 patients diagnosed with hypertension or glaucoma who had self-administered eyedrops for at least six months; we videotaped them instilling drops and had them answer questions about their use of the medications.1 The results were revealing: Among other findings, 20 percent of "compliant" patients didn't get even a single drop onto their eye. To make matters worse, most of them didn't even realize they'd failed to get the medication in.
Others instilled too many drops. Most patients wasted drops, and many touched the bottle to their eyes. Meanwhile, most of these subjects thought they were doing a great job of administering the medication and had no idea there was a problem.
Not getting the drops onto the eye becomes even more of a concern when the patient has poorer vision. There's an obvious irony here: The people who most need the medication—and are most likely to feel the urgency of being compliant—are most likely not to end up instilling the medication as prescribed. (And many of them still don't realize anything is wrong.) Many doctors in this situation, noting that the patient's vision is still deteriorating, suspect that the patient is being noncompliant or that the target IOP isn't low enough. That's certainly possible, but it's equally likely that the patient is simply not successfully administering the drops.
One of the reasons this problem escapes many doctors' notice is that it's easy to think of using eyedrops as being analogous to taking pills. If your general practitioner prescribes a 90-day supply of an anti-hypertensive pill, the pharmacist gives you 90 pills. Unless you drop one behind the counter or the dog eats some of them, those 90 pills will get you through 90 days. With glaucoma medication eyedrops, there are a specific number of drops in the bottle, but whether those drops will last 90 days is highly questionable.
How Many Drops Does It Take?
In the study mentioned earlier, we found that among experienced hypertensive and glaucoma patients, the average number of drops put in the eye per successful instillation was 1.8—almost twice the correct amount. Even more amazing, the patients used an average of seven drops in each attempt. So if you assume that a bottle that contains 45 drops will last 45 days, you may be off by a wide margin. In fact, most of us have heard patients complain that their drops don't last as long as they're supposed to.
Given this reality, the average glaucoma patient who is struggling to pay his bills may run out of his three-month supply well before the three-month period is up. At that point he can either pay a substantial amount out of pocket or simply stop and wait for the end of the three-month period and then get more drops. More than likely, he'll take the latter option. In addition, he may take the drops less frequently from then on to make sure they last three months.
We've attempted to contact insurers about making an allowance for this. Unfortunately, insurers seem to be moving in the opposite direction—putting stricter limitations on what constitutes a three-month supply of medication. We've also discussed this with people at the
In hindsight, it seems obvious that the average patient wouldn't think to complain to CMS about running out of drops too soon. If they complained to anyone other than their doctor, it would probably be the medication manufacturer or the pharmacy. On the other hand, it makes sense that CMS needs evidence to support making a change. So, in hopes of remedying this situation, we now encourage our patients to register a complaint with CMS if they run into this problem. To make this easier, we provide our patients with a written, detailed description of how to call CMS, navigate the automated system and speak to a representative.
Instillation: What Goes Wrong
We're currently analyzing approximately 800 videos of individuals attempting to self-administer eyedrops. We hope to find out exactly what approaches do and don't work so that specific problems can be addressed. Our criteria for successful self-administration is that the patient 1) gets the drop in the eye; 2) only puts in a single drop; and 3) does not touch the bottle to the eye. In our experience so far, less than a third of the patients met all three criteria.
Here are a few of the specific mistakes the patients we monitored made when trying to instill eyedrops:
• Not being able to open the bottle. Even doctors sometimes struggle to open an eyedrop bottle in front of a patient, so it shouldn't be hard to understand why some patients with limited fine motor capability find the tamper-proof seal quite troublesome. Outside of your office, some of these patients will simply give up out of frustration.
• Not keeping the eye open. Keeping the eye open may seem obvious, but many of our videos show people trying to put drops in with their eyes closed. The patient may not understand the need for the eye to be open, or may simply find it hard to keep it open.
(It's a natural defense mechanism to close the eye when a foreign object is approaching.)
In the latter situation, an easy technique for surmounting the problem is to use one's fingers to hold the eye open. Some patients understand this; however, in response to one of our questionnaires in a recent study, 20.5 percent said they didn't hold their eyes open, and of those who said they did, 80 percent only held one lid open (mostly the lower lid).2
• Not using gravity to their advantage. If you stand up and hold the bottle perpendicular to your eye, the drop is going to go straight down onto the floor or onto your cheek. Again, we have many videos of patients doing this. The patient needs to learn to position the bottle directly over the eye, pointing towards the eye.
• Not bracing the bottle. If the bottle isn't braced against the other hand or braced against your nose, a small tremor in the bottle-holding hand may be sufficient to cause the drop to miss the eye.
• Not looking at the bottle. Some patients are reluctant to watch the drop coming toward them, so they look away. This deprives them of visual feedback, so that even if they're doing everything else right, the drop may end up on the nose.
• Letting the bottle touch the eye. To avoid contamination, the patient needs to keep the bottle from touching the eye or skin. In our recent study, 21.9 percent of the subjects touched their eye when using a 15-ml bottle and 30.8 percent touched their eye when using a 2.5-ml bottle. Notably, many patients are aware that they're doing so; in response to our questionnaire, about half admitted that they let the bottle touch their eyes. (Apparently, they fail to realize the danger.)
Previous studies have found contamination in 19 percent of drops tested before eight weeks of use and in 40 percent of drops tested after eight weeks of use; 91 percent of the bacteria found were gram positive.3 Based on these statistics, it's clear that the human body is highly resilient; if it weren't, far more people would be suffering from ocular infections.
• Putting in too many drops. This may be a function of fine motor skill limitations—not being up to the task of squeezing gently enough to produce only a single drop at a time. However, it could also indicate a lack of corneal sensitivity. For example, one young doctor we taped was unable to feel the drops landing on his cornea, and as a result had no idea how many drops he had put in; after seven or eight drops he still thought he had missed his eye.
One possible way to avoid this problem is to cool the drops in the refrigerator. However, lowering the temperature of some drops might be contraindicated because of their chemistry. (The package insert should help clarify whether this approach is safe, should a patient have this particular problem.)
Helping the Patient Get It Right
So what can a clinician do to address this issue?
• Let your patients know that this is a common problem. People can easily overlook a problem if they have no idea that it may exist. Discussing it focuses their attention on their technique and the importance of not being too casual about instilling drops. It also allows them to air their difficulties with the doctor without fear of ridicule.
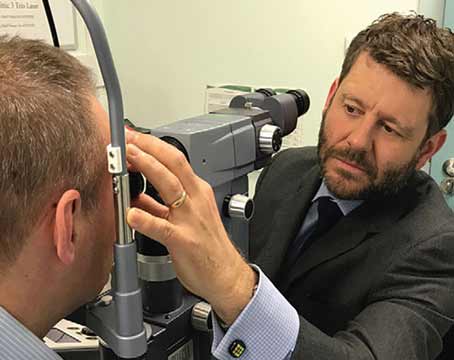
• Ask your patients to show you how they put in their eyedrops. Few ophthalmologists do this, but it's an easy way to find out if a patient is likely to have trouble getting the prescribed dose into the eye.
• Have a staff member teach the patient ways to address specific delivery problems. Although this strategy will help in many cases, it's not foolproof. If a lack of fine motor skills is contributing to the problem, all the training in the world may not solve it. (On the other hand, the patient will at least be aware of the issue.)
If a lack of fine motor skills is contributing to the problem, the doctor might ask that someone else be responsible for eyedrop administration. If this is not a viable solution, the next option may be switching to another form of therapy such as laser or surgery.
• Suggest that patients follow basic strategies for successful drop administration. These include: Wash your hands (in response to our questionnaire, one-third admitted they rarely do so); use your fingers to hold both lids open; look at the bottle; brace the hand holding the bottle against either your nose or the hand holding the lids open; minimize the distance from the bottle to the eye (without touching the eye); make sure the bottle is positioned above the eye so that gravity will put the drop onto the eye; and if feasible, chill the drop so you can tell when it has landed on the eye.
• Suggest that patients having trouble get assistance from a friend or family member. The drawback here is that this requires imposing on others, which some patients may be reluctant to do, either because of inconvenience or because of the desire to remain autonomous.
• If patients run out of drops early, have them contact CMS or the pharmacy benefit manager. Make them aware that this may help remedy the problem in the future. Provide them with information about how to register their comments.
• If you know a patient has a problem administering drops and the drops don't seem to be working, don't prescribe additional drops. Instead, consider switching to a laser or surgical approach. If it seems likely that the drops aren't making it into the patient's eye, it makes no sense to prescribe additional drops.
• Become an advocate for your patients with pharmacy benefit managers. If your patients don't end up taking their drops correctly, both you and they will pay a price. Fighting for a more realistic number of drops in the bottle will help.
Building a Better Bottle
Another way to minimize self-administration concerns might be through better bottle design. To date, most of the research on bottle design has focused on concerns such as evaporation, compatible materials, percentage of fill, preservative reactions with the bottle itself, and so forth. There have been some creative attempts to address the issue of making sure the medication reaches the eye, such as a bottle that mists the liquid into the eye, but no one has provided any data so far proving that these alternatives work.
Ironically, there may be some difference between existing bottle designs. In one of our recent studies,1 we asked patients to simulate their normal drop instillation technique.
We had them use familiar bottles containing sterile saline solution (to avoid overdosing on medication). Subjects who normally used Alcon's Systane used Systane bottles; subjects who used Travatan or Xalatan used a Travatan bottle. The point was not to compare the efficacy of the bottles, but to ensure that subjects were simulating their normal routine.
To our surprise, the bottles appeared to make a difference in the results: Subjects using the Travatan bottle did better in all three criteria (getting the drop in the eye, instilling only one drop and not touching the bottle to the eye). We were surprised to find this correlation, and so far we're unable to explain the reason for the difference.
Heading Toward a Solution
The seriousness of this problem can hardly be overstated. Compliance is always an issue, but if patients who are trying to be compliant are failing to instill their medicine correctly, that might account for a significant percentage of poor outcomes among our hypertensive and glaucoma patients.
Hopefully, our research will help to elucidate the specific problems that individuals have administering their eyedrops and lead to more productive ways to address these concerns. For example, we're working on developing an educational video for patients; the primary concern here will be finding the most convenient way to expose the patient to it.
In the meantime, we hope that better ways to deliver medications to the eye will be developed. If we can find better ways to help patients get the right number of drops into the eye, both our patients and our practices will benefit.
Dr. Robin is clinical professor of ophthalmology at the
1. Stone JL, Robin
2. Tsai T, Robin
3. Geyer O, Bottone EJ, Podos SM, Schumer RA, Asbell PA. Microbial contamination of medications used to treat glaucoma. Br J Ophthalmol 199579:4:376-9.