Workup, Diagnosis and Treatment
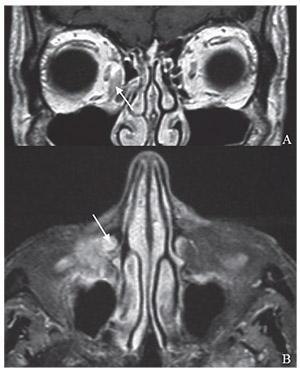 |
| Figure 2. MRI of the orbits showing an enhancing increase in soft tissue in the right medial orbit (A, arrow) with extension inferiorly into the nasolacrimal duct (B, arrow). |
Prior to referral to the Wills Eye Hospital, a surveillance MRI of the orbits had demonstrated an enhancing amorphous increase in soft tissue inseparable from the right medial canthal tendon and anterior margin of the medial rectus (Figure 2A); the lesion demonstrated deep adnexal involvement with extension inferiorly into the nasolacrimal duct (Figure 2B). An orbitotomy for biopsy of the orbital mass, ethmoid mucosa and lacrimal sac was performed, and histopathology from all sites was consistent with BCC. After discussing the treatment options, the patient decided to proceed with exenteration of the right orbit and ethmoidectomy in a combined case with the otolaryngology service. Frozen sections were obtained during the case, and the resection margins were negative for tumor. Permanent sections of the right exenterated orbital tissue, including the medial rectus, the inferior rectus and conjunctiva, as well as the posterior ethmoid bone, were positive for tumor. Based on this finding, the patient opted for further surgery to resect the posterior ethmoid bone. Of note, during this case, the oculocardiac reflex was elicited when traction was placed near the optic nerve stump; the surgery was otherwise uneventful.
Approximately one year after exenteration, the patient underwent additional skull base surgery for recurrence, with placement of a skin flap over the empty orbit (Figure 3). Two years after exenteration, surveillance PET-CT revealed increased uptake in the right posterior maxilla with a 3-mm area of uptake in the left apical lung. Endoscopic biopsies revealed recurrent BCC of the orbit and bilateral frontal sinuses, for which the patient underwent adjuvant radiation therapy.
Discussion
Basal cell carcinoma is the most common malignancy in the world and is responsible for 90 percent of malignant eyelid tumors. More than 20 percent of basal cell carcinomas of the head and neck are periocular, with the lower lid being the most common site, followed by the medial canthus, upper lid and lateral canthus. BCC of the medial canthus is most likely to invade the orbit or present with aggressive histology, followed by the lower eyelid, the upper eyelid and the lateral canthus. Nevertheless, orbital invasion is rare, with reported incidence rates ranging from 1.6 to 2.5 percent.1
 |
| Figure 3. External photo showing the postoperative appearance after placement of a skin flap over the exenterated orbit. |
Basal cell carcinoma is the most common malignancy in the world and is responsible for 90 percent of malignant eyelid tumors. More than 20 percent of basal cell carcinomas of the head and neck are periocular, with the lower lid being the most common site, followed by the medial canthus, upper lid and lateral canthus. BCC of the medial canthus is most likely to invade the orbit or present with aggressive histology, followed by the lower eyelid, the upper eyelid and the lateral canthus. Nevertheless, orbital invasion is rare, with reported incidence rates ranging from 1.6 to 2.5 percent.1
Our patient presented to us for evaluation of a right medial canthal lesion with a history of multiple recurrences of basal cell carcinoma in that region. Imaging revealed invasion of the orbit with extension into the nasolacrimal duct. Suspicion was high for recurrent BCC, which was confirmed by biopsy. Treatment options for periocular BCC consist of surgical excision (Mohs micrographic surgery or wide surgical excision with frozen sections), exenteration, radiotherapy, vismodegib (hedgehog pathway inhibitor), or imiquimod (topical immunotherapy), although vismodegib and imiquimod are newer therapies and were not yet available at the time of this patient’s presentation. Topical, medical or radiation therapy may be used as adjuvant therapy or in patients who are poor surgical candidates, but surgical excision remains the treatment of choice in patients suitable for surgery. However, when there is bulbar extension or extensive orbital invasion, exenteration should be considered.1,2 In fact, intraorbital spread of eyelid, globe or conjunctival malignancies is the most frequent indication for orbital exenteration.2
In an ambispective cohort study of 31 consecutive patients who underwent orbital exenteration for a malignant neoplasm invading the orbit, investigators found that the median (50 percent) survival period for all patients studied was 78.4 months. Median length of survival in patients with BCC was 60 months, although there was no significant difference in time to death when stratified by tumor histologic subtype (basal cell carcinoma, squamous cell carcinoma and other). The decision to perform orbital exenteration can be difficult since the operation results in substantial disfigurement and dysfunction for patients. However, the authors conclude that exenteration provides sufficiently good survival outcomes to justify its use.2 Management options considered for our patient were radiation, surgical excision and orbital exenteration. Given the extent of this patient’s orbital disease and his history of multiple recurrences, we thought that surgical excision or radiation would be unlikely to control his disease and exenteration would therefore offer him a better prognosis. In addition, given his visual acuity of count fingers in the right eye secondary to advanced glaucoma, exenteration would minimally impact his visual function. For these reasons, it was felt that the benefits of exenteration far outweighed the risks, and in fact, we questioned whether or not he would have benefited from exenteration earlier in his clinical course.
In addition to lending itself to a discussion of the management options of periorbital basal cell carcinoma, this case is also noteworthy for elicitation of the oculocardiac reflex from an empty orbit. This reflex was first reported in 1908 and has since become a well-documented clinical phenomenon.3 It has been reported to occur in a wide variety of ophthalmic procedures involving traction on the extraocular muscles,4-8 for which it is probably most familiar to ophthalmologists. In contrast, elicitation of the OCR from an empty orbit is rare, and only a handful of cases have been reported in the anesthesia literature.8-12
In conclusion, this is a case of an 88-year-old male with a history of multiple primary malignances, including recurrent BCC of the right cheek and right medial canthus, who presented with recurrent right medial canthal basal cell carcinoma with orbital invasion and extension into the nasolacrimal duct. Given the extent of his orbital disease, the decision was made to proceed with exenteration. Despite an aggressive surgical approach, he developed skull base, orbital and frontal sinus recurrences, requiring multiple additional surgeries and radiation. REVIEW
1.ShiY,JiaR,FanX.Ocularbasalcellcarcinoma:Abrieflitera-Fax (206)676-5005 ture review of clinical diagnosis and treatment. Onco Targets
Ther 2017;10:2483-2489.
2. Hoffman GR, Jefferson ND, Reid CB et al. Orbital exenteration to manage infiltrative sinonasal, orbital adnexal, and cutaneous malignancies provides acceptable survival outcomes: An institutional review, literature review, and meta-Analysis. J Oral Maxillofac Surg 2016;74:3:631-43.
3. Blanc VF, Hardy JF, Milot J et al. The oculocardiac reflex: A graphic and statistical analysis in infants and children. Can Anaesth Soc J 1983;30:4:360-9. 4.AptL,IsenbergS,GaffneyWL.Theoculocardiacreflexin strabismus surgery. Am J Ophthalmol 1973;76:4:533-6.
5. Anderson RL. The blepharocardiac reflex. Arch Ophthalmol 1978;96:8:1418-20.
6. Munden PM, Carter KD, Nerad JA. The oculocardiac reflex duringenucleation.AmJOphthalmol1991;111:3:378-9.
7. Bailey JH. The oculocardiac reflex. Am J Ophthalmol 1935;18:1:22-25.
8. Kerr WJ, Vance JP. Oculocardiac reflex from the empty orbit. Anesthesia 1983;38:883-5.
9. Nicholson D, Kossler A, Topping K et al. Exaggerated oculocardiac reflex elicited by local anesthetic injection of an empty orbit: A case report. A A Case Rep 2017;9:12:337–8.
10. Tsai JC, Heitz JW. Oculocardiac reflex elicited during debridement of an empty orbit. J Clin Anesth 2012;24:5:426-7.
11. Ward B, Bass S. The oculocardiac reflex in a congenitally anophthalmic child. Paediatr Anaesth 2001;11:3:372-3.
12. Shanks AB, O’Carroll TM. Oculocardiac reflex from the empty orbit. Anaesthesia 1984;39:3:291-2.



