 |
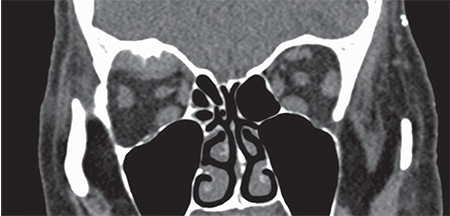
| Figure 2. Coronal section of a CT scan of the orbits showing homogenous enlargement in the area of the superior rectus and levator superioris with adjacent bony reaction of the orbital roof. |
Workup, Diagnosis and Treatment
Ancillary imaging studies included CT scan of the orbits without contrast, which showed a 2.3 x 2.2 x 0.7 cm soft tissue subperiosteal mass within the superior posterior aspect of the right orbit, with associated periosteal reaction and cortical thinning (Figure 2). MRI of the brain and orbits with and without contrast showed the same size heterogenous mass in the right orbit, involving the orbital roof and superior rectus muscle. Orbitotomy of the affected right orbit was performed, and the tumor was removed piecemeal with long rongeurs. The tumor was found to extend to the orbital apex, and the periosteal reaction was extensive.
Grossly, the mass consisted of fragments of firm, gray and dark brown tissue measuring 12 x 11 x 5 mm in aggregate. Microscopic evaluation demonstrated fragments of lamellar bone with reactive changes, surrounded by nests, islands and bands of infiltrating malignant cells with frequent mitotic figures, apoptotic bodies and geographic necrosis (Figure 3). Immunohistochemical stains showed that the neoplastic cells expressed NKX3.1 and androgen receptors.
The combined clinical, morphologic and immunohistochemical findings were compatible with metastasis of the patient’s known prostate adenocarcinoma to the orbit, prompting referral to an oncologist for systemic management.
Discussion
Metastatic orbital lesions account for approximately 1 to 13 percent of all orbital tumors reported in the literature.1 In a review of 1,264 patients with orbital tumors from the Wills Eye Hospital Oncology Service, metastatic tumors to the orbit were the seventh most common type of orbital lesion, comprising 7 percent of all orbital tumors. In adults over the age of 60, metastases comprised 10 percent of the total number of tumors.2 The reported incidence of metastatic tumors to the orbit has increased in recent years; this may be due to an increase in the median survival of patients with cancer, as well as improvement in our ability to detect metastasis with refinement of ancillary studies and fine-needle aspiration biopsy techniques.3 The most common types of cancer to metastasize to the orbit include breast, lung and prostate carcinomas.1-3
Prostate carcinoma is the most common malignancy in males in the United States, with an estimated 220,800 new cases in 2015. In the past decade, there have been several advances in our ability to treat metastatic prostate carcinoma. Despite such advances, metastatic prostate carcinoma remains an often-lethal disease accounting for approximately 27,000 cancer-related deaths in the United States annually.4
Prostate carcinoma has a well-recognized pattern of metastatic disease, most frequently involving the axial skeleton and local lymph nodes. Skeletal metastases are predominantly osteoblastic (95 percent of cases) and preferentially involve the spine, pelvis and femur. These lesions are found in up to 84 percent of patients with advanced disease. Metastasis to the orbit is rare, occurring in less than 1 percent of patients with prostate carcinoma.5
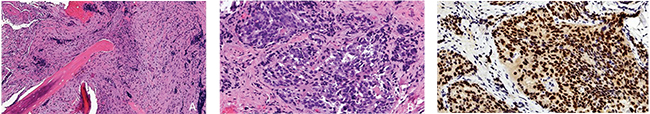 |
| Figure 3. A: Spicules of bone associated with dense fibrosis (hematoxylin-eosin; original magnification x 50). B. Higher magnification demonstrates nests of atypical cells with a vaguely cribriform arrangement in a densely fibrotic stroma (hematoxylin-eosin; original magnification x 100). C: The neoplastic nuclei express prostate adenocarcinoma marker NKX 3.1 (original magnification x 100). |
In general, the presenting symptoms of orbital metastasis include proptosis, pain, diplopia, decreased vision and ptosis.3,6 Pain is more common in prostate carcinoma because it tends to spread to the orbital bone and periosteum where there are sensory nerves rather than orbital soft tissue. Bony lesions are usually osteoblastic and may simulate a meningioma, especially if the sphenoid bone is affected. The rapid development of osteoblastic orbital lesions in an elderly male is highly suggestive of metastatic prostate carcinoma.3
Nearly all prostate cancers are carcinoma, specifically adenocarcinoma, and can range from well-differentiated to very poorly differentiated. Recognition of metastatic prostate carcinoma is important, since it can be managed safely and effectively with hormonal therapy. Prostate carcinoma is a radiosensitive malignancy, so treatment for orbital disease usually consists of radiotherapy combined with hormonal therapies.3
In summary, we describe a patient with metastatic prostate adenocarcinoma to the orbit, who presented with painful blepharoptosis and limitation of extraocular motility. This case highlights the importance of medical history in guiding diagnostic workup and management. REVIEW
1. Shields JA, Shields CL, Scartozzi R. Survey of 1,264 patients with orbital tumors and simulating lesions. Ophthalmology 2004;111:997-1008.
2. Demirci H, Shields CL, Shields JA, et al. Orbital tumors in the older adult population. Ophthalmology 2002;109:243-248.
3. Ahmed SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Current Opinion in Ophthalmol 2007;18:405-13.
4. Park JC, Eisenberger MA. Advances in the treatment of metastatic prostate cancer. Mayo Clin Proc 2015;90:1719-33.
5. Long MA, Husband JES. Features of unusual metastases from prostate cancer. Br J Radiol 1999;72:933-41.
6. Shields JA, Shields CL, Brotman HK, et al. Cancer metastatic to the orbit. Ophthalmic Plast Reconstr Surg 2001;17:346-354.



