Advanced Medical Optics and IntraLase last month entered into a definitive agreement for AMO to acquire IntraLase for approximately $808 million in cash.
AMO expects the transaction to be completed early in the second quarter of 2007. The transaction is subject to IntraLase stockholder approval as well as regulatory approvals and other customary closing conditions. "This acquisition offers significant strategic value by further establishing AMO as the global refractive technology leader, positioning us with a broad range of technologies and expertise to serve the needs of comprehensive refractive practices," said AMO Chairman, President and CEO Jim Mazzo.
IntraLase President and CEO Robert J. Palmisano added, "There will now be the ability to advance our femtosecond laser technology in a coordinated way, both developmentally and commercially, with the world's leading excimer laser technology. Also, this combination provides the opportunity for further innovation and beneficial refinement of LASIK procedures that can and should grow the overall LASIK market."
Carl Zeiss Meditec received Food & Drug Administration clearance to market the laser keratome applications of its Visumax femtosecond laser system. The company had previously projected that this clearance would be granted in the second half of 2007. For a further description of the technology, see this month"s article on femtosecond lasers.
The addition of the IntraLase femtosecond laser technology into AMO's portfolio of refractive technologies complements AMO's fundamental growth strategy.
AMO also announced the acquisition of WaveFront Sciences Inc., which designs and manufactures the industry's highest resolution Shack-Hartmann-based aberrometer. The acquisition expands AMO's portfolio of industry-leading laser technologies and strengthens its pipeline of new wavefront-guided diagnostic innovations.
Said Mr. Mazzo, "This acquisition represents another step forward in AMO's strategy to provide a full range of products and services that meets the needs of comprehensive refractive practices." AMO acquired WaveFront Sciences for approximately $20 million, including a $14 million cash payment at closing and an agreement to make a total of $6 million in future cash payments contingent on achievement of certain milestones over the next three years. Based in Albuquerque, New Mexico, WaveFront Sciences is a privately held company.
New Lucentis Data On Several Fronts
New two-year data from the second pivotal Phase III study that led to the Food and Drug Administration approval of Lucentis (ranibizumab) was presented last month. Data from the ANCHOR study showed that the improvement in visual acuity endpoints in the Lucentis groups at year one was maintained at year two. Overall, these data are consistent with the one-year ANCHOR and two-year MARINA data recently published in the New England Journal of Medicine. The ANCHOR study is a head-to-head study of Lucentis and verteporfin (Visudyne) photodynamic therapy in patients with wet age-related macular degeneration.
Key two-year ANCHOR findings include:
• Approximately 90 percent of patients treated with 0.3 mg and 0.5 mg of Lucentis maintained or improved vision (defined as a loss of less than 15 letters in visual acuity) compared to approximately 66 percent of those treated with PDT.
• Up to 41 percent of patients treated with Lucentis improved vision (defined as a gain of 15 letters or more) compared to approximately 6 percent of patients treated with PDT.
• Two-year safety and efficacy data are consistent with findings from one-year ANCHOR data and two-year MARINA data.
In a separate study reported in December's American Journal of Ophthalmology, intraocular injections of ranibizumab significantly reduced foveal thickness and improved visual acuity in 10 patients with diabetic macular edema, which demonstrated that VEGF is an important therapeutic target for DME, the authors conclude. They call for a randomized, controlled, double-masked trial to test whether intraocular injections of ranibizumab provide long-term benefit to patients with DME.
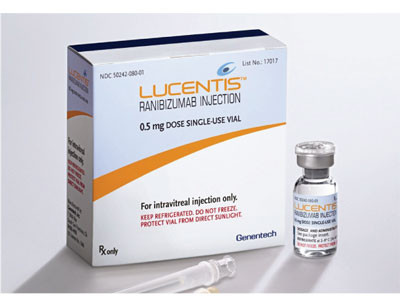
The researchers, at the Wilmer Eye Institute at Baltimore's Johns Hopkins University School of Medicine, performed intraocular injections of 0.5 mg of ranibizumab at baseline and at one, two, four and six months in 10 patients with chronic DME. The primary outcome was change in foveal thickness between baseline and seven months, and the secondary outcome measures were changes from baseline in visual acuity and macular volume.
Mean values at baseline were 503 µm for foveal thickness, 9.22 mm3 for macular volume, and 28.1 letters (20/80) read on the ETDRS visual acuity chart. At seven months (one month after the fifth injection), the mean foveal thickness was 257 µm, which was a reduction of 246 µm (85 percent of the excess foveal thickness present at baseline; p=.005 by Wilcoxon signed-rank test for likelihood that this change is due to ranibizumab rather than chance). The macular volume was 7.47 mm3, which was a reduction of 1.75 mm3 (77 percent of the excess macular volume at baseline; p=.009). Mean visual acuity was 40.4 letters (20/40), which was an improvement of 12.3 letters (p=.005). The injections were well-tolerated with no ocular or systemic adverse events.
Reuters also reported in late January that Genentech had sent a letter alerting eye doctors to the risk of stroke from Lucentis. The letter was a "proactive effort" to advise doctors that an interim analysis of a 5,000-patient trial shows that 1.2 percent of patients given a 0.5-mg dose of the drug suffered a stroke, compared with 0.3 percent of patients given a lower 0.3-mg dose, spokeswoman Dawn Kalmar told the news service.
She said the findings are consistent with data from previous trials as well as the label for Lucentis, which was approved by the FDA last June.
"We've shared this information with the FDA and there is no indication, based on our discussions with the agency, that this will change the label," Kalmar said.
TVT Study Reveals One-Year Results
Non-valved tube shunt surgery was more likely to maintain IOP control and avoid persistent hypotony or reoperation for glaucoma than trabeculectomy with mitomycin-C during the first year of follow-up, according to the one-year results of the Tube Versus Trabeculectomy (TVT) Study, published in January's American Journal of Ophthalmology. Both surgical procedures produced similar intraocular-pressure reduction at one year, but there was less need for supplemental medical therapy following trabeculectomy with MMC, the report said.
The multicenter, randomized trial at 17 clinical centers enrolled patients 18 to 85 years of age who had previous trabeculectomy and/or cataract extraction with intraocular lens implantation and uncontrolled glaucoma with intraocular pressure ≥18 mmHg and ≤40 mmHg on maximum tolerated medical therapy. Patients received Baerveldt glaucoma implant or trabeculectomy with mitomycin-C. Main outcome measures were IOP, visual acuity and reoperation for glaucoma.
A total of 212 eyes of 212 patients were enrolled, including 107 in the tube group and 105 in the trabeculectomy group. At one year, IOP (mean ±SD) was 12.4 ±3.9 mmHg in the tube group and 12.7 ±5.8 mmHg in the trabeculectomy group (p=.73). The number of glaucoma medications (mean ±SD) was 1.3 ±1.3 in the tube group and 0.5 ±0.9 in the trabeculectomy group (p<.001). The cumulative probability of failure during the first year of follow-up was 3.9 percent in the tube group and 13.5 percent in the trabeculectomy group (p=.017).
B&L Aligns with Acufocus Presbyopia Technology
Bausch & Lomb announced that it made an equity investment in and secured an exclusive option to purchase AcuFocus Inc., a privately held company located in Irvine, Calif., that is developing corneal inlay technology for the treatment of presbyopia.
The AcuFocus ACI 7000 is designed to treat presbyopia. The AcuFocus corneal inlay is designed to treat presbyopia in all patients, including those who have had cataract surgery, and reduce their dependence on reading glasses.
The ACI 7000 corneal inlay is implanted in the cornea under a LASIK flap in a simple outpatient procedure. The device incorporates technology that increases the patient's depth of field, thereby improving near vision. The ACI 7000 has been designed to maintain normal corneal physiology and corneal health. The procedure does not involve tissue removal nor does it permanently alter the cornea, so pre-implant vision can be restored if the inlay is removed.
Recent studies have demonstrated that the ACI 7000 improves near vision in patients who previously didn't require vision correction (emmetropes) as well as those who have had LASIK surgery. Trials are being conducted to study the ACI 7000 in patients with intraocular lenses.
'Patient-Shared Billing' Expands to Toric IOLs?
Alcon announced that CMS also issued a ruling that allows Medicare beneficiaries undergoing cataract surgery to choose an astigmatism-correcting intraocular lens, such as Alcon's AcrySof Toric. Similar to the CMS decision allowing cataract patients access to presbyopia-correcting IOLs, this new ruling allows patients to pay the additional charges for the correction of pre-existing astigmatism while Medicare provides customary reimbursement for cataract surgery. In addition to this ruling, CMS also noted that it will issue guidance to Medicare contractors, including the specific IOLs impacted by this ruling.
CMS Releases New Code for Retisert Implant
The Centers for Medicare & Medicaid Services has established a product specific J-Code for Bausch & Lomb's Retisert fluocinolone acetonide intravitreal implant 0.59 mg. The Retisert implant was approved as a single-indication orphan drug by the FDA for the treatment of chronic noninfectious posterior segment uveitis in patients 20 to 50 years of age.
The new J-Code, J7311 Fluocinolone acetonide intravitreal implant, replaces the Medicare hospital outpatient code, C9225, which had been available to hospitals for billing Medicare when the Retisert implant is implanted in a hospital outpatient setting. The J7311 code should be recognized by all health-care insurers as they add this code to their respective billing systems. CMS also has published a payment rate for J7311 of $19,345, or 106 percent of the average sales price for the product.
"This is an important milestone, which recognizes the national utilization of the Retisert implant and the critical and unique role it may play in preventing cumulative damage to the visual system caused by recurrent episodes of inflammation," said Michael O'Rourke, general manager of the U.S. Pharmaceutical business for Bausch & Lomb.
The J-Code and Medicare payment rate are effective as of January 1, 2007. Private insurers may pay at different rates than Medicare.



