Some scientists jokingly say the abbreviation of the Janus kinase family, JAK, stands for "just another kinase." Actually, JAKs are a crucial part of the direct signal transduction pathway known as JAK-STAT. In fact, JAKs are so important, they were named after the Roman god of gates, Janus, who is commonly depicted with two faces, one looking forward, and one looking backward. Like Janus, JAKs have two molecular "faces": a pseudokinase domain (JH1) and a catalytic kinase domain (JH2).1 Like Janus, the god of gates, the Janus kinase-STAT pathway controls a "gate" connecting cytokine signals with transcription.
Recent research in respiratory allergy underlines the importance of the JAK-STAT pathway in asthma, a condition that's very close to ocular allergy. This article will describe inhibitory mechanisms of JAK-STAT signaling which are relevant to the treatment of atopic ocular allergic conditions.
Histamine and the Th1/Th2 Balance
Breakthroughs in ocular allergy often come from research into atopic conditions such as asthma, eczema and rhinitis.2 In both the lungs and the eye, allergies begin with sensitized mast cells covered with FceRI receptors bound to immunoglobulin E (IgE) antibodies. Regardless of their location, mast cells react to antigen in the same way.2 When activated, mast cells degranulate, releasing mast cell mediators including histamine, various cytokines and leukotrienes. In atopic syndromes, the healthy balance of T helper cells is disrupted. Histamine released from mast cells increases the number of T helper type 2 (Th2) lymphocytes and reduces the number of T helper type 1 (Th1) lymphocytes.3 Th2 cytokines such as the crucial interleukins (IL)-4 and IL-13 are upregulated, and Th1 cytokines like IL-2 and IFN are downregulated.
The Th imbalance created by histamine perpetuates the allergic response through a positive feedback loop. Mast cells secrete histamine, leading to a "baby boom" of Th2 cell differentiation. Th2 cells, in turn, maintain an environment which favors persistent IgE synthesis through cytokine signaling.4 IgE synthesis helps sensitize mast cells, continuing the allergic cycle. Th2 cell differentiation is mediated by JAK-STAT signaling, and consequently JAK-STAT is central to this positive feedback loop. The JAK-STAT pathway describes the journey of cytokine signals through the cell membrane, the cytoplasm and the nuclear membrane to their destination: DNA.
The JAK-STAT Pathway
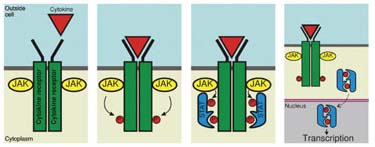
Receptors on the surface of cells act like biological "keyholes." When a cytokine binds to its receptor, the "lock" begins to "turn," activating JAKs. JAKs phosphorylate tyrosine residues in the cytoplasmic region of the receptor.1 In essence, the part of the "lock" inside the cell is changed to allow molecules called signal transducer and activator of transcription (STAT) proteins to join the team of molecules congregating near the cellular membrane.
STAT monomers link with the phosphorylated tyrosine sites the JAKs have made, and become tyrosine phosphorylated. Once the right molecular "package" of activated STATs is complete, it is released from the receptor. The STATs are able to translocate to the nucleus, passing through the nuclear envelope to reach DNA where genes are transcribed.
The JAK-STAT pathway is a complicated process. It can be thought of as a kind of nanobiological relay race. The cytokine passes the "baton" to the JAK, which passes it the STAT, which reaches the DNA. Seven STATs have been identified. Recent JAK-STAT research into asthma has focused on one of the STAT molecules, STAT6.
High levels of STAT6 have been found in the airways of asthmatic patients.5 Interestingly, atopic asthma patients have a higher density of STAT6 cells than patients with nonatopic asthma. Although no ophthalmic study of STAT6 has been done, to our knowledge, given the predominance of STAT6 in respiratory atopic allergy, however, it is conceivable that STAT6 is upregulated in atopic ocular allergy.
Japanese genetic studies have validated the connection between STAT6 and allergies.6 Genetic polymorphisms in the first exon of STAT6 have been correlated with atopic diseases such as asthma, food allergies and atopic dermatitis. In other words, variations in the DNA encoding STAT6 can be linked to the allergies.
Regulation of STAT Signaling
Once the cytokine "key" has bound to the receptor "lock," the JAK-STAT cascade is controlled by a series of negative regulators. These regulators include suppressors of cytokine signaling (SOCS), protein inhibitors of activated STAT (PIAS), STAT serine phosphorylation and arginine methylation.1 The primary motivation behind research into STAT regulatory pathways is clear: STAT regulation pathways could be potentially manipulated in therapeutic interventions for immunological disorders.
|
This alteration of the Th1 and Th2 balance hasn't been shown in a model of allergic disease, but it's easy to imagine the therapeutic potential of a drug with a mechanism similar to SOCS5. As previously described, histamine tilts the Th1/Th2 balance during the immunological allergic response. A molecule that could correct the Th balance, tilting the Th1/Th2 balance to its pre-histamine level, might be developed into a useful drug.
In 2003, a group of Japanese researchers investigated SOCS3 in allergic responses.8 In one of their more striking experiments, the researchers measured SOCS3 expression in adult patients with atopic asthma. They found asthmatics had significantly higher SOCS3 expression compared to healthy controls. They also found SOCS3 expression increased in proportion to disease severity. However, SOCS3 expression was not affected by steroid therapy. These data suggest that an agent with the ability to inhibit SOCS3 expression would affect an immunological pathway not currently managed by local steroid treatment.
Novel Signaling Therapies
For ocular allergy, cytokine signaling drugs exploiting JAK-STAT regulatory pathways are purely speculative. In the 2006 World Transplant Congress, a series of abstracts described research that justified some of the speculation in recent literature.
Janus Kinase 3 (JAK3) inhibitors have exciting immunosuppressive properties many authors reported in last summer's Transplant Congress. Stanford University's Stephen Hendry, MD, and co-workers reported that JAK3 inhibitors may be able to duplicate the efficacy of current immunosuppressants, with fewer unwanted toxicities.
Pfizer presented data on a Phase I trial of its JAK3 inhibitor, CP-690,550, demonstrating the agent was safe and that it improved psoriasis lesions within 14 days in patients treated with high doses.
Promising preclinical studies were also updated at the meeting: Dr. Hendry reported that the JAK3 inhibitor R935 extended the survival of heart grafts in rats; and the University of Texas' Hermangshu Podder, MD, reported that the inhibitor NC1153 extended the survival of kidney grafts in rats.
Of course, the novel immunosuppressive agents used to aid transplant tolerance would not be appropriate for the treatment of allergies. Successful targeting of cytokine signaling pathways does demonstrate the wealth of therapeutic potential in JAK-STAT regulation.
Hope for the Future
In the early 1990's, it was unclear how cytokines affected transcription. It was evident that cytokines would bind to cell-surface receptors and then disappear into the cell. Later, evidence of gene transcription appeared. In their 1994 paper, James Darnell, MD, Ian Kerr, PhD, and George Stark, PhD, described the JAK-STAT direct signal transduction pathway for the first time.9 Their research, which started as an investigation of two interferons (a and g), ended with the discovery of a fundamental biologic process. The JAK-STAT pathway connected the cytokines outside the cell to transcription inside.
The JAK-STAT pathway and the regulatory pathways that intersect it are complex. Drugs targeting the JAK-STAT pathway are in development for a variety of conditions unrelated to ocular allergy. Research into asthma, measuring molecules including STAT6 and SOCS3, has shown the JAK-STAT pathway is relevant in atopic allergy. For now, the hope for a novel ocular allergy therapy is simply that—a hope. But it is a hope that could very well become reality.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Mr. McLaughlin is a medical writer at ORA Clinical Research & Development in North Andover.
1. Chen, W., Daines MO, et al. Turning off signal transducer and activator of transcription (STAT): The negative regulation of STAT signaling. J Allergy Clin Immunol 2004;114:3:476-89.
2. Abelson MB. Allergic Diseases of the Eye. Philadelphia: W.B. Saunders Co., 2001.
3. Packard KA, Khan MM. Effects of histamine on Th1/Th2 cytokine balance. Int Immunopharmacol 2003;3:7:909-20.
4. McIlroy A, Caron G. Histamine and prostaglandin E up-regulate the production of Th2-attracting chemokines (CCL17 and CCL22) and down-regulate IFN-gamma-induced CXCL10 production by immature human dendritic cells. Immunology 2006;117:4:507-16.
5. Pernis AB, Rothman PB. JAK-STAT signaling in asthma. J Clin Invest 2002;109:10:1279-83.
6. Tamura K, Suzuki M, et al. Linkage and association studies of STAT6 gene polymorphisms and allergic diseases. Int Arch Allergy Immunol 2003;131:1:33-8.
7. Seki, Y, Hayashi K, et al. Expression of the suppressor of cytokine signaling-5 (SOCS5) negatively regulates IL-4-dependent STAT6 activation and Th2 differentiation. Proc Natl Acad Sci U S A 2002;99:20:13003-8.
8. Seki, Y, Inoue H, et al. SOCS-3 regulates onset and maintenance of T(H)2-mediated allergic responses. Nat Med 2003;9:8:1047-54.
9. Darnell JE, Kerr IM, et al. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science 1994;264:5164:1415-21.