Refractive IOL implantation still poses many challenges today. Meeting patient goals and expectations, achieving consistent and accurate results with theoretical formulas and counseling patients about their options are just some of the hurdles refractive surgeons face.1
Adjustable IOL technology, however, may be able to offer some solutions. RxSight’s (formerly Calhoun Vision) Light Adjustable Lens (RxLAL), which received Food and Drug Administration approval in the fall of 2017, and the developing Perfect Lens femtosecond laser technology are two promising advances in this field. Both of these technologies are able to alter the refractive characteristics of an implanted IOL after surgery in order to achieve a customized, patient-specific refraction. Adjustable IOL technology may also enable the delegation of pre and postop counseling to ODs and increase bilateral same-day sequential cataract surgery volume.1 Two-part modular IOLs offer another possible option. Here, we’ll take a closer look at these adjustable IOL technologies and how they work.
Outlook
Surgeons say that adjustable IOLs’ potential for customization after they’re implanted will bring peace of mind and represent a significant step forward. “Being able to adjust refractive error, treat astigmatism and add or ‘erase’ multifocality in an accurate manner is exciting,” says Y. Ralph Chu, MD, founder of Chu Vision Institute in Minnesota and a member of the Perfect Lens scientific advisory board.
Adjustable IOL technology has the potential to improve many cataract outcomes, but one population that’s particularly well-suited to postop adjustments is those who have had previous refractive surgery. “It’s very hard to do lens power calculations on previous refractive surgery patients, particularly radial keratotomy,” says Sydney Tyson, MD, MPH, of Wills Eye Hospital in Philadelphia. “The greatest patient benefit is probably knowing that you’ll have the best result you can possibly have with a minimum amount of effort on both the surgeon’s part and the patient’s part,” he says. “Right now, if patients pay a certain amount of money to get a certain result, it doesn’t necessarily guarantee that outcome.
“Everyone is anatomically different, and there’s a lot of variability in proper lens placement,” Dr. Tyson continues. “If we can efficiently fine-tune a patient’s vision postoperatively, then we’re not as dependent on theoretical formulas for lens power calculations. We don’t really know where the lens is going to sit inside the capsular bag when we implant it—it could be a little anterior or a little posterior or even be tilted—and that’ll change the patient’s prescription, particularly with premium lenses, which magnify misses more than monofocal lenses.
“Classically, we would do adjustments by laser vision correction after the fact, or sometimes in extreme cases, a lens exchange,” Dr. Tyson explains. “But those are costly, and in the case of LASIK, you’re working on the cornea to make adjustments. For lens exchanges, you have to go back into surgery, and it’s another procedure with the risk of infection and the associated complications.”
Experts say there’s still a significant percentage of patients with missed target refractions.2 A 2018 multicenter data study of 282,811 cases reported to the European Registry of Quality Outcomes for Cataract and Refractive Surgery between January 2014 and December 2015 found that the biometry prediction error within 0.5 D was achieved in only 72.7 percent of the cases. A biometry prediction error within 1 D was achieved for 263,015 eyes (93 percent).3 The authors reported that risk factors such as poor preoperative CDVA, ocular comorbidity and previous eye surgery were related to poor refractive outcomes.
Similarly, a 2014 retrospective study of 1,275 cataract surgeries performed in 2010 at Massachusetts Eye and Ear Infirmary reported that 94 percent of cases (1,196 surgeries) achieved outcomes within 1 D of the target refraction.4 The authors note that the refractive outcomes at the academic teaching institution were higher than average international benchmarks.
From a market opportunity standpoint, adjustable IOL technology like Perfect Lens, which can adjust almost any IOL, may become one of the biggest growth areas in ophthalmology, predicts Kevin M. Miller, MD, professor and Kolokotrones chair of ophthalmology at the David Geffen School of Medicine at UCLA, and member of the Stein Eye Institute. “I think there’s a bigger potential for this technology than we saw with LASIK and PRK, because there are so many more people it would apply to. There are already millions of people in the United States with lens implants, and not all of them see perfectly. They can get glasses to correct their residual refractive errors, or they could have a noninvasive procedure to adjust their implants so they wouldn’t have to wear glasses. If the cost wasn’t too high—maybe the difference between a $300 pair of glasses and a $1,000 procedure—then many patients might opt for the procedure.”
IOLs Today
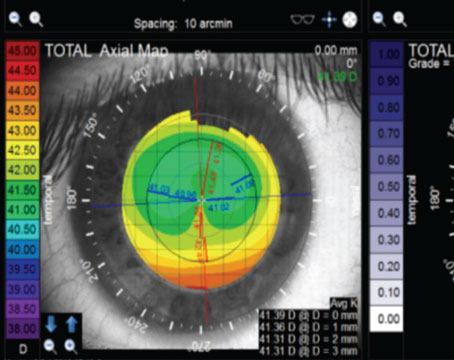
Current IOL technology still involves unwanted optical phenomena.Furthermore, surgeons must still estimate surgically-induced astigmatism, effective lens position and posterior corneal astigmatism. ASCRS points out that posterior corneal astigmatism is a significant knowledge gap in the field. According to the ESCRS 2018 Clinical Survey, only 65 percent of surgeons consider PCA in their toric power calculations.5 In the ASCRS 2018 Clinical Survey, 17 percent of respondents don’t think it’s clinically significant (versus 27 percent of non-U.S. respondents), 35 percent believe there’s no good way of measuring it and 29 percent don’t know how to calculate PCA or understand its significance.
As for intraoperative aberrometry, about 60 percent of respondents stated they have no plans to use it, and only 3 percent of respondents currently use it on all cataract patients.6
The Options: Modular IOLs
Modular IOLs include a base unit implanted in the capsular bag and an exchangeable optic. Changing out the optic to improve refractive accuracy requires an additional trip to the OR and a second incision. Modular IOL systems allow for adjustments of the optic throughout a patient’s life. Toric optics can be rotated and realigned and multifocals can be exchanged for monofocals if patients fail to neuroadapt.7
Modular IOLs tend to be bulkier than traditional IOLs because they’re a two-piece system, but surgeons can achieve a great deal of accuracy and predictability with modular IOLs because effective lens position isn’t much of an issue, says Dr. Tyson. “We fill the bag completely with a silicone substance. When the lens is replaced, we know exactly where it is, as opposed to a traditional IOL, which could be in one spot or another, depending on where it finally ends up.”
Several modular IOLs are in development or currently available, like the Juvene (LensGen, Irvine, CA), a biomimetic device with the ability to change curvature to mimic the eye’s natural lens, and the Harmoni Modular IOL (Alcon).
The Options: RxLAL
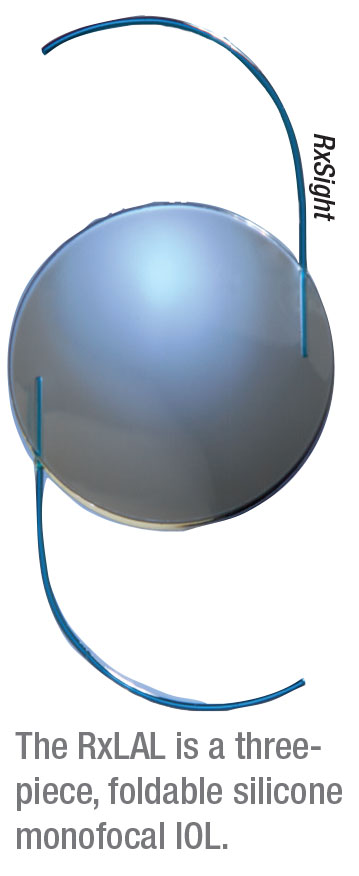 |
RxSight’s RxLAL is currently the only FDA-approved light adjustable lens on the market. Its slit lamp-based light delivery device technology is built to adjust its own specialized IOL—a three-piece foldable silicone monofocal light-adjustable lens that’s implanted through a 2.8-mm clear corneal incision with a proprietary injector.1 The overall diameter is 13 mm with a 6-mm optic, squared posterior optic edges, round anterior edges, and blue poly(methyl methacrylate) modified-C haptics with posterior optic-haptic 10-degree angulation. The IOL is available in powers from +10 to +30 D; in 1-D increments from +10 to +15 D and +25 to +30 D; and in 0.5-D increments from +16 to +24 D.2 The IOL can be modified up to a total of 3 D of cylinder and 2 D of sphere.2
Vance Thompson, MD, of Vance Thompson Vision in Sioux Falls, South Dakota, one of the FDA-monitored sites for the RxLAL, says the light adjustable lens is ideal for those who aren’t candidates for multifocality but want a premium lens, as well as for those who don’t wish to risk glare and dysphotopsias and those who desire precision monovision or precise distance vision with reader glasses.
“Currently, we estimate the effective lens position and incisional healing in our calculations,” Dr. Thompson says. “In addition to those two big variables, our inability to precisely measure posterior corneal astigmatism makes cataract surgery less accurate than we would like it to be. LASIK is often used for fine-tuning, but there are a lot of patients who’d rather have their optic fine-tuned than their cornea. Now, when we explain to patients why implants aren’t as accurate as LASIK, we can offer them a new implant where final effective lens position and final astigmatism won’t matter once healing has taken place, because for the first time ever, we can customize the power of the implant inside their eye to their desired vision for the remainder of their life.”
The photoreactive silicone of the RxLAL has two unique features, explains Dr. Miller. “The first is the mobile molecules. You can think of the lens as ‘half-baked’—it’s not completely polymerized in the manufacturing process, so there’s some silicone material that’s not locked in. Most of the time, when you bake silicone, you polymerize the entire thing and lock in the refraction, but for the RxLAL, about 10 percent of the lens isn’t locked, and that 10 percent has a photosensitizer attached to it, so that when UV light hits it, it polymerizes. The second special feature is the heavy UV-blocking back layer. You don’t want to shine intense UV light into the eye while treating this lens and cause retinal damage.”
The light adjustments are done with a specific wavelength of UV light (365 nm).2 Each light treatment lasts approximately 20 to 30 seconds, depending on the type of treatment, while the final lock-in adjustment treatment is longer. “It’s important that patients remain still and look straight ahead,” Dr. Miller notes.
“The lens is implanted like any standard cataract lens,” he continues. “It’s silicone, so it’s very springy inside the eye and opens up quickly. Once the lens finds a stable place in the eye a few weeks after surgery, the patient is placed in front of the light delivery device for adjustments and the final lock-in.”
Doctors tend to feel comfortable with the RxLAL because it’s implanted just like any other IOL, says Dr. Thompson. Similarly, the light adjustments function a bit like LASIK. “In laser vision correction, if we want to increase the power of the cornea, we treat the outside part of the cornea to bring more curvature to the center,” he says. “With a light adjustable lens, to increase power, or lessen hyperopia or increase myopia, you illuminate the center of the lens by photopolymerizing the macromers in the center. When the unpolymerized macromers diffuse from the periphery to establish equilibrium, you get an increase in curvature in the center. If you want to decrease power, or lessen myopia, you would treat the outside portion of the lens and photopolymerize those macromers so the unpolymerized macromers in the center will migrate toward the periphery, for a negative lens effect.
“You can also do this in a toric fashion,” Dr. Thompson adds. “It’s very specific math. Anything you can mathematically describe, you can do with light adjustability in a very accurate fashion. Once you achieve the desired power and the patient decides that’s the vision they want, you irradiate the whole lens equally to consume all of the unpolymerized macromers and polymerize the lens. The lock-in is a power-neutral treatment and doesn’t change anything.”
Light Treatments
The RxLAL is FDA-approved for three or four light treatments over a one-to-two-week period 17 to 21 days after surgery.8 The RxLAL recipient is also required to limit his or her UV light exposure for the duration of the fine-tuning phase by wearing polarized UV-blocking glasses both indoors and outdoors to ensure the adjusted refraction isn’t affected by ambient UV light.
“It’s very important that patients wear their UV protective glasses, which come in both clear and sunglass options,” says Dr. Thompson. “We start the adjustments at three weeks postop. Typically it’s three adjustments, at least 48 hours apart, so you can pretty much do a full adjustment with a Monday, Wednesday, Friday schedule. Then there are two lock-ins in the following week, and it’s finished.”
Setting patient expectations is important for these adjustment visits—which some surgeons worry could be onerous—since these visits aren’t brief. At each exam, patients will undergo refraction and measurements before the adjustments and dilation for five visits. “You’re doing two- or three-hour visits, and you want to plan accordingly,” Dr. Thompson says. “At the same time, patients are getting the vision they want for the rest of their life with a procedure that doesn’t touch the cornea, and without the risks associated with LASIK or PRK. It’s amazing when you hit your true refractive endpoint.”
Benefits & Results
Surgeons familiar with the technology say that, in addition to the ability to fine-tune the postop refraction, the RxLAL offers some other benefits in terms of the mechanics of the procedure and the results.
• Short learning curve. Compared to PRK and LASIK, adjusting the RxLAL has a relatively small learning curve. “One of the things that intimidates doctors first getting involved in the premium lens journey is having a patient with leftover correction who isn’t fully satisfied and needs some fine-tuning on the cornea,” Dr. Thompson says. “[Laser refractive surgery] is a whole other discipline that a lot of doctors may not want to add, along with the expensive technology. With the RxLAL, it’s just your typical cataract surgery and typical postop care. Setting up a patient for the light-delivery device with a focusing lens on the cornea looks a lot like you’re getting ready to do a YAG laser. You center the beam, enter the correction into the computer and deliver it.”
• Precision. Yassine Daoud, MD, chair of ophthalmology at Howard County General Hospital and assistant professor of ophthalmology at Johns Hopkins University School of Medicine remarks that the RxLAL’s FDA clinical results were fairly comparable to the accuracy we see in LASIK and PRK. The Phase III FDA clinical study for the RxSight in subjects with pre-exisitng corneal astigmatism included 600 patients, and 91.8 percent of patients achieved a result within 0.5 D of the target. “This is remarkable,” he says. “That’s 20 percent more within half a diopter [compared to the benchmark outcomes of 75 percent within 0.5 D].” All of the patients in the RxLAL study saw 20/40 or better postop uncorrected. This is comparable to surgeons’ results from LASIK in studies such as the FDA’s PROWL-I and -II.9
• Long-term results. While the RxLAL has been available in the United States only since 2017, it’s been available in Mexico and Europe since 2008. A study published this year in the Journal of Cataract and Refractive Surgery of a seven-year follow-up and clinical evaluation of the RxLAL after cataract removal found that the 61 patients (103 eyes) with the lens had stable refraction, good visual acuity and no IOL-associated pathologies. Additionally, the UV light exposure from adjustment and lock-in treatments wasn’t found to cause any additional endothelial damage.2 Rabbit models irradiated at one, two, three and five times the expected maximum UV irradiation doses have shown no retinal toxicity after near-UV light exposure up to five times, which is the expected maximum light treatment dosage for adjustment and lock-in of the RxLAL.10
RxLAL Limitations
RxSight says it launched the RxLAL in about 30 sites across the United States. To date, the company says the light adjustable lens accounts for about half of the premium procedures performed at the sites. In addition to the usual issues with selling patients on premium lenses and their increased cost, surgeons note a couple other issues that might slow down widespread use of the lens.
• All those postop visits. One of the reasons posited as to why more surgeons aren’t implanting the lens is that many of them worry that the number of follow-up treatments and time investment for patient and physician may be burdensome. “Our current IOL formulas achieve very reasonable outcomes,” Dr. Daoud says. “So why would a heavy-volume surgeon or any clinical specialist want to offer a procedure that may not be covered by insurance or would require a patient to wear sunglasses for a few weeks or return for four or six additional visits to fine-tune their prescription? In the meantime, we have ways of correcting significant residual refractive error with LASIK or PRK.”
• Dilation requirements. “You need to be able to dilate to 7 mm for the adjustment,” Dr. Thompson says. “And that’s to give you a little bit of insurance, if you will, because the beam we’re using to make the adjustment is 5.5 mm in diameter. So if the optic is perfectly centered on the pupil, 5.5 mm is all you need, but not everybody’s lens is centered perfectly in their pupil. We like them to be dilated to 7 mm so we can ensure that we’re going to be able to light-adjust the whole optic.
“Sometimes, if there’s dilation fatigue, we use stronger drops or a pledget soaked in dilating drops,” says Dr. Thompson. “But if we got them to dilate to 7 mm in their consult, we’ll get them to dilate to 7 mm again; we just might have to work harder at it. I wouldn’t recommend using the RxLAL in a patient if you can’t dilate them pharmacologically to 7 mm. They wouldn’t be a good candidate.”
A possible solution would be to decrease the treatable area to 5 mm, suggests Dr. Miller. “If they made a 6-mm lens with a central 5-mm treatable area, we could treat more patients who have smaller pupils or dilation problems. There wouldn’t be as many molecules to move around, so you wouldn’t get quite the same amount of change in lens power and you might lose a diopter or so, but there’d be many more small-pupil patients for whom you could implant the lens and offer treatment.”
Future RxSight Developments
The current LAL technology is a one-time adjustment that’s locked in, but a continuously adjustable option is possible. “It’s called two-photon technology,” Dr. Miller explains. “Right now, patients need to wear UV-blocking glasses so the atmospheric UV light doesn’t affect the lens in their eye and adjust it in a random fashion. With two-photon technology, there would be two very specific wavelengths of light that hit the lens at the same time, which are, from my understanding, not available in sunlight, so patients wouldn’t have to worry about refractive effects on their lens.
“In this scenario, you could implant someone with a LAL and bring them in for adjustment, adjust them, and then leave the rest of the molecules in the lens untouched and in reserve for a future treatment, if need be,” he continues. “The current FDA approval is for the adjustments and permanent lock-in procedure, but future iterations of the RxLAL could include a continuously adjustable version.”
The Options: Perfect Lens
 |
Perfect Lens is a specialized femtosecond laser that can modify a standard hydrophobic acrylic lens that’s already implanted inside the eye. Toricity, asphericity, spherical aberration and multifocality can be achieved in a brief office procedure, says the company. Additionally, the Perfect Lens technology can manufacture IOLs with customized prescriptions for patients ex vivo.
“Every year we do a survey from ASCRS and ESCRS, and what we’ve found is that the third most common reason for requiring an IOL exchange is incorrect lens power,” says Nick Mamalis, MD, ASCRS president and professor at the University of Utah School of Medicine. He’s currently researching for Perfect Lens. “Even with improvements in measuring and calculating the implants, we still end up with refractive surprises. Perfect Lens will be a good way of correcting misses without having to exchange an IOL or put in a piggyback lens.”
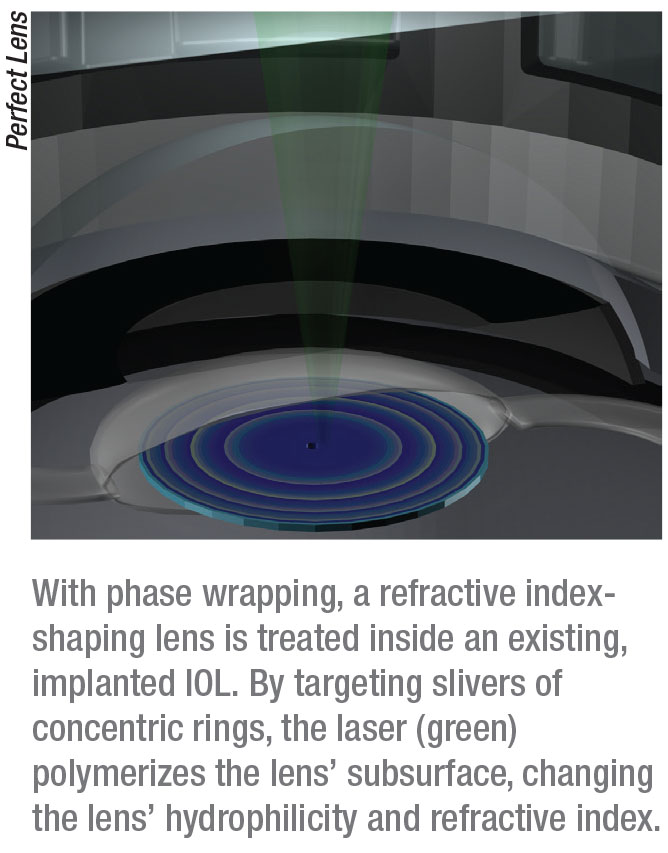
Use of femtosecond lasers to change refractive indices of materials has been studied for years.11,12 Along with ophthalmic inventor Stephen Q. Zhou, Perfect Lens executive vice president, COO and physicist Ruth Sahler and vice president and physicist Josef Bille discovered a process by which existing molecules within a polymeric material become hydrophilic inside an intraocular lens.13 When immersed in an aqueous medium and exposed to femtosecond laser radiation, polymeric material gains the ability to undergo a hydrophilicity-based refractive index change.14
The Perfect Lens technology has mainly been tested on hydrophobic acrylic, since it’s the most widely-used material in lenses in the United States, but it could in theory work on hydrophilic acrylic, says Dr. Mamalis. At present Perfect Lens doesn’t work on silicone, but Dr. Chu says it could be made to. “Right now, most of the work has been done on acrylics,” he says.
Dr. Mamalis explains how the Perfect Lens laser technology works. “Perfect Lens is a type of femtosecond laser, but it has very low power and a very fine focus. The laser creates a focal change in the lens’ hydrophilicity, so it doesn’t change the surface of the lens, it changes its subsurface (50 microns below the surface),” he says. “Changing the hydrophilicity changes the refractive index of the lens itself in the focal area. We do this with a technique called phase wrapping. Instead of changing the entire curvature of the lens, we have concentric rings of phase wrapping where a tiny change in the polymer itself creates a significant change in the power of the whole lens. So we’re only treating a very small portion of the lens at a time, just underneath the surface.”
Dr. Chu explains that treating the inside of the lens in different patterns modifies refractive error, astigmatism and multifocality. “It all depends on the pattern,” he says. “One of the benefits is that this procedure doesn’t affect the cornea. Your patient lies down and there’s a cone that engages the eye. The laser is focused precisely into the lens. Performing a Perfect Lens procedure is very similar to LASIK in that it’s kind of a one-shot procedure. There aren’t any additional follow-up visits for fine-tuning adjustments.”
An in vivo Perfect Lens treatment is a very brief procedure. “You dock the laser to the eye as if you were going to laser for cataract surgery, but achieving the amount of correction takes less than a minute or so,” says Dr. Mamalis. “Maybe up to a minute and a half. It’s not a long procedure. Theoretically it could be done in an outpatient surgical suite; you wouldn’t have to go to the main operating room. The greatest patient benefit is the fact that you could correct their vision without having to resort to a secondary surgery. This would eliminate the need for IOL exchange, piggyback IOLs, or having to do a LASIK or PRK on the cornea to correct vision.”
“I think the idea of a patient being able to ‘try on multifocality’ or ‘try on reading vision’ is pretty attractive,” Dr. Chu says. “If a patient tries a multifocal lens, it’s nice for him or her to know that there’s a technology that could be used to modify the multifocality without having to go back inside the eye and to the OR.”
Perfect Lens can lock-in a customized refraction for a patient, but that doesn’t mean the patient must keep that vision for life. In theory, Perfect Lens technology might be able to modify a lens up to 20 times, says Dr. Miller. “Light is applied to only a very thin sliver of the lens,” he says. “The treatment changes the structure of the acrylic molecules and thus the hydrophilicity of the material to either attract or repel more water in an infinitesimally small portion of the lens. At a later date, if a patient develops a refractive error, you could simply treat a different sliver of the lens—though you might have to keep track of which portion you’ve already treated, since you can’t treat the same sliver twice. To add or take away multifocality, you simply do the inverse of what you did previously, just like putting a +2 D lens in front of an eye with a -2 D lens. Since the average person lives 10 to 11 years after cataract surgery, you wouldn’t need to re-treat the lens too often. About two or three treatments would be good for life, if they’re needed at all.”
“On the bench and in the laboratory, we’ve been able to change the lens up to several diopters,” Dr. Mamalis says. “The adjustments made are within a tenth of a diopter of the intended correction.15 It’s very precise.” For the experimental study of femtosecond laser-created refractive lenses, the Perfect Lens study group used a standard hydrophobic model (EC-1Y), a femtosecond laser, an acoustic-optic modulator, beam-shaping optics, a scan system and an objective lens to create the refractive index change within the IOL. Building a refractive index shaping lens within an IOL using a femtosecond laser lets the IOL’s refractive properties be altered.15 Studies on rabbit models, specifically pigmented rabbits, showed no signs of retinal toxicity or corneal or endothelial damage.16 Perfect Lens is approaching human trials soon.
Will Biometry Still Matter?
With new technology for modifying refraction postoperatively and potentially eliminating refractive surprises, some wonder what effect this will have on the perennial cycle of innovation in preop biometry, but surgeons say that biometry is still key to accurate IOL implantation. “We might be reaching the limits of what biometry can do,” notes Dr. Chu. “Biometry has improved so much recently.”
“Biometry won’t become obsolete because we still need to get into the general ballpark for IOL power,” Dr. Tyson says. “You have to know where to shoot so you can minimize the amount of adjustment afterward.”
“Postoperative lens adjustments will complement biometry,” adds Dr. Mamalis. “It’s not like you’re going to put a 20-D lens in everybody and just correct it. Get as close as you can with biometry, and if there’s a significant refractive error left after the eye’s healed from surgery, then this technology could adjust that.”
Dr. Miller predicts a slow end to biometry innovation if technologies like RxLAL and Perfect Lens come into wide use. “I don’t think the light adjustable lens is going to be the end, since it’s not continuously adjustable right now. For the Perfect Lens, if this can be turned into a continuous treatment throughout a patient’s life, it’ll depend on how much lens change can be achieved. Super-accurate formulas would then become superfluous—just get it close enough and adjust from there once the patient has reached refractive stability. Biometry just won’t need to be super accurate.” REVIEW
Drs. Tyson and Daoud have no financial disclosures. Dr. Miller has no financial relationships but notes that he was an investigator for RxSight (when it was Calhoun Vision). Drs. Mamalis and Chu are on the Perfect Lens scientific advisory board. Dr. Thompson discloses relationships with RxSight, Alcon and Johnson & Johnson.
1. Chang D. Disruptive innovation and refractive IOLs: How the game will change with adjustable IOLs. Asia-Pacific J Ophthalmol 2019;8:6:432-435.
2. Schojai M, Schultz T, Schulze K, et al. Long-term follow-up and clinical evaluation of the light-adjustable intraocular lens implanted after cataract removal: 7-year results. J Cataract Refract Surg 2020;46:8-13.
3. Lundström M, Dickman M, Henry Y, et al. Risk factors for refractive error after cataract surgery: Analysis of 282,811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J Cataract Refract Surg 2018;44:447-452.
4. Simon SS, Chee YE, Haddadin RI, et al. Achieving target refraction after cataract surgery. Ophtahlmol 2014;121:440-444.
5. ESCRS Clinical Results Survey: 2018 Results. Accessed March 3 2020. https://www.eurotimes.org/wp-content/uploads/2019/11/Clinical-Survey-Results-2018-12pp-Supplement-press.pdf.
6. ASCRS Clinical Results Survey: 2018 Results. EyeWorld Supplements. Accessed March 3 2020. file:///Users/cleonard/Downloads/ascrs-clinical-survey-2018.pdf.
7. Werner L. The Harmoni Modular IOL System. Cataract and Refractive Surgery Today 2018. Accessed March 4 2020. https://crstoday.com/articles/2018-may/the-harmoni-modular-iol-system/.
8. FDA approves first implanted lens that can be adjusted after cataract surgery to improve vision without eyeglasses in some patients. FDA.gov Press Release. Accessed 2 March 2020. https://www.fda.gov/news-events/press-announcements/fda-approves-first-implanted-lens-can-be-adjusted-after-cataract-surgery-improve-vision-without.
9. Eydelman M, Hilmantel G, Tarver ME, et al. Symptoms and satisfaction of patients in the Patient-Reported Outcomes With Laser in situ leratomileusis (PROWL) Studies. JAMA Ophthalmol 2017;135:1:13-22.
10. Werner L, Chang W, Haymore J, et al. Retinal safety of the irradiation delivered to light-adjustable intraocular lenses evaluated in a rabbit model. J Cataract Refract Surg 2010;36:8:1392-7.
11. Ohmachi Y, Igo T. Laser induced refractive-index change in As–S–Ge glasses. Appl Phys Lett 1972;20:12:506–508.
12. Ding L, Blackwell R, Kunzler JF, et al. Large refractive index change in silicone-based and non-silicone-based hydrogel polymers induced by femtosecond laser micro-machining. Opt Express 2006;14:24:11901–11909.
13. Sahler R, Zhou SQ, Bille JF. Hydrophilicity alteration system and method. US Patent 9186242B2 (2015).
14. Bille J, Engelhard J, Volpp H-R, et al. Chemical basis for alteration of an intraocular lens using a femtosecond laser. Biomed Opt Express 2017;8:3:1390-1404.
15. Sahler R, Bille JF, Enright S, et al. Creation of a refractive lens within an existing intraocular lens using a femtosecond laser. J Cataract Refract Surg 2016;42:8:1207-1215.
16. Werner L, Ludlow J, Nguyen J, et al. Biocompatibility of intraocular lens power adjustment using a femtosecond laser in rabbit model. J Cataract Refract Surg 2017;43:8:1100-1106.