Rainbow glare is an infrequent side effect of LASIK with flaps created in a raster-type pattern, such as those created by the IntraLase. Even when it does occur, patients often don't notice it. However, in some cases the rainbow glare will be bothersome and surgeons will have to address it with the patient. Here's an update on the mechanism behind rainbow glare, the situations that might make it more pronounced and some strategies for managing it.
A Persistent Case
Two years ago,
Though the patient's eyes appeared fine the following day, he complained about a rainbow-colored glare that mainly occurred when viewing light sources. "His vision was good but the rainbow glare was quite distressing to him," says Dr. Melki. "We treated him for dry eye, mild haze and found nothing unusual in terms of ocular findings. We thought it was something that was going to improve with time but it persisted for him." The patient is still bothered by the glare two years later, never underwent an excimer ablation and is hesitant to undergo any further laser surgery.
Breaking Down the Rainbow
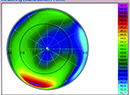
Cleveland Clinic surgeon Ronald Krueger has published on rainbow glare, and his theory is that it's a function of the way the laser creates its cut. "Rainbow glare is primarily caused by the perfect placement of the femtosecond laser spots in an array pattern that sets up a constructive interference that leads to a splitting of the light into colors," explains Dr. Krueger. "Because the pattern is in this perfect array, there's a geometry to it that looks like something along the lines of a square or a rectangle, with streams of light shooting out in multiple colors. It's kind of like a starburst array, with the colors proceeding like those of a rainbow, with red colors closest to the point light source and blue colors farther away. A patient who notices it will see it most prominently in the dark when looking at a pinpoint light source, such as oncoming headlights while driving at night."
Dr. Krueger says it's interesting that there was a component of this phenomenon in the development of the Accufocus corneal inlay for presbyopia. "When the company first put the inlay together, it put all these holes in the lens that were in a perfect array," he says. "This created glare phenomena because of the constructive interference. The designers then changed it to a random array of holes and the glare phenomenon went away. It's a physical phenomenon in which a random pattern makes it so that it's not optically constructive to the point of creating a distortion. If it's in a regular pattern, however, you're going to get distortion."
Improvements in laser technology may greatly minimize the occurrence of rainbow glare, however. Dr. Krueger published a retrospective study in which he analyzed the complaints of rainbow glare from two groups of patients: one that was treated with older IntraLase technology and another that was treated with a laser with newer software. In group 1, the newer-laser group, 90.2 percent of patients were contacted postop, and 37 patients (69 eyes) reported symptoms of rainbow glare around lights, for an incidence of 19.07 percent. In group 2, the newer-tech group, 88.6 percent of patients were contacted, and two of them (four eyes) reported similar symptoms, for an incidence of 2.32 percent. He found that spacing in the array was approximately 9 µm, which corresponded to the measurement of the older laser's spot and line separation.1 Dr. Krueger notes that he was specifically asking patients about it, so for most it was something they didn't actively complain about.
 Recently, however, Perry Binder, MD, medical director for Abbott Medical Optics, presented a poster at the 2010
Recently, however, Perry Binder, MD, medical director for Abbott Medical Optics, presented a poster at the 2010
Dr. Krueger says it's important to make sure your laser is in alignment to help reduce the risk of rainbow glare. "I've found that if your laser is a little out of alignment, you'll have to use higher energies to get the effect you want," he says. "And it's going to cause a little bit more of a broader burst that's more likely to result in rainbow glare. Lower energies and tighter spacings might make it a little less noticeable."
A Course of Action
Though newer laser technology may minimize the problem further, there's always a chance some patient will complain of rainbow glare postoperatively. Here's what surgeons recommend doing in response.
"I tell patients that it's a side effect of IntraLASIK and it's usually not visually disturbing," says Dr. Krueger. "It's often something they may just notice and wonder about rather than actively complain about. If you explain that it's just an optical effect from some of the pulses and that it, hopefully, will go away with the passage of time, they'll usually go with the flow and say, 'OK.' "
Being able to treat the patient with the excimer, rather than leaving the flap unlifted, may make a difference, as well. Dr. Melki believes that's what occurred with his patient. "I think what made it more pronounced for the patient was the fact that we didn't treat him with the excimer," avers Dr. Melki. "When the excimer treats the femtosecond's raster pattern left over in the stromal bed from flap creation, the pattern isn't as prominent anymore, and you don't have as much rainbow glare. But because this patient's flap wasn't lifted, this resulted in the glare he was noticing.
"If the patient who is bothered by rainbow glare has already had an excimer ablation, your options are limited," Dr. Melki continues. "In that case, make sure to rule out the usual suspects for glare first, such as dry eyes or large pupils. For the latter, try constricting the pupils with Alphagan or pilocarpine. But if the patient has
any residual refractive error, I'd do a wavefront measurement and then a treatment. For the retreatment, if you haven't lifted the first flap, you can consider recutting a new flap at a deeper plane. If the flap's been lifted previously, though, I'd much rather do a surface ablation treatment with adjunctive mitomycin-C."
1. Krueger RR,