Whether you are a seasoned orbitofacial surgeon or a comprehensive ophthalmologist, repair of blepharoptosis can be a challenging endeavor. Often surgical technique is felt to be at the forefront of a satisfactory surgical outcome, but meticulous preoperative evaluation and planning is paramount to achieve successful results. Before undertaking repair of a ptotic eyelid, the authors employ an algorithm when evaluating patients.
Select Your Patient
A well-considered battery of questions might reveal a systemic etiology of their blepharoptosis.1 We routinely question the patient with regards to onset and progression of his blepharoptosis. Does the patient have dysphagia, diplopia, and diurnal variation of his ptosis or extremity weakness? A positive answer to any of these may raise the possibility of myasthenia gravis. Is there a history of dry eye syndrome or connective tissue disorders? Ptosis repair can certainly increase or initiate dry eye symptoms, a possibility which must be discussed with the patient. Is there a history of healing abnormalities that can result in exuberant scarring? Are the expectations of the patient unrealistic? Has the patient had previous eyelid surgery and if so, was he satisfied with the outcome? We have found a comprehensive history to be invaluable in selecting surgical candidates and minimizing unfavorable outcomes.
Evaluate Your Patient
All patients should routinely have their visual acuities, pupillary function and extraocular motility documented. A usual array of eyelid vital signs should be measured including the margin reflex distances, levator function, palpebral fissure and lid crease height. In addition, you should carefully look for lagophthalmos and perform a Schirmer's 2 tearing test in the standard fashion, and done with topical anesthetic. Any evidence of lagophthalmos or decreased tear production warrants discussion with the patient concerning the risk of dry eye symptoms following surgery.
Furthermore, the presence of lagophthalmos may necessitate lower lid repositioning during surgery, since elevation of the eyelid can exacerbate the degree of lagophthalmos. A floppy eyelid that has gone unnoticed can prove to be a challenging obstacle during ptosis repair. Recognizing this syndrome prior to surgery can facilitate necessary planning of a canthopexy, Sires technique2 or resection.
Technique
Although a myriad of surgical techniques has been described in the literature, the external levator advancement is likely the most commonly performed technique. The external levator advancement is performed on patients who demonstrate good to excellent levator function. An eyelid crease incision is fashioned 9 to 10mm above the upper eyelid lash line in women and at 7 to 8mm in men. These measurements may vary depending on the ethnic ancestry of the patient.
When creating these markings, we make certain the eyelid is on stretch and the patient is looking down to avoid misplacement of the incision. Observation of the eyelashes beginning to roll outward before marking our incision site is always made.
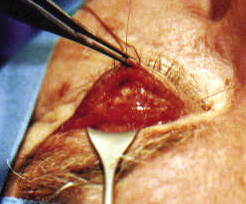
 |
| Figure 1: Left upper eyelid following removal of excess skin. Note the traction suture allowing for additional lid stretch during dissection. |
Before scrubbing, hang a good picture of the patient where you can see it to help guide your surgery.
We routinely employ the use of traction suture placed through the meibomian gland of the upper eyelid margin. Stretching the skin so it becomes taut is necessary to ensure a good incision. Watch the depth of your incision to avoid breeching the orbicularis, septum or levator. Identify and incise the orbicularis to clearly expose the orbital septum. The orbital septum should be grasped and pulled straight up to prevent inadvertent damage to deeper structures. The septum should be opened for the length of the wound to expose the preaponeurotic fat pad. If you do not identify this landmark, stop and ask yourself where you are. Gentle pressure on the eye can often accentuate the appearance of the fat pad. Once identified, the fat pad should be dissected off the levator aponeurosis while it lies posteriorly to the fat pad.
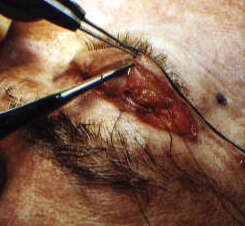
 |
| Figure 2: Tarsal levator suture. |
Now it is time to elevate that lid! There is a wide and abundant variety of opinions regarding suture material. In our minds it is not the suture material but the placement of the suture that counts. Of course you would choose not to use an 8-0 or 9-0 suture, but a 5-0 or even 6-0 suture that is double- armed certainly suffices. Where do you place the suture through the tarsus? Not an easy question to answer. What has worked best for us is to gently grasp and elevate the tarsus while asking the patient to open his or her eyes. Assess the contour and if necessary, regrasp the tarsus at a different point and reassess. Once you are satisfied with the contour of the eyelid, pass one end of your suture in a partial-thickness fashion through the tarsus. Make sure you get a good bite of tarsus.
My fellowship preceptor said it best: "no wimpy bites." After passing your suture, the eyelid should always be everted to ascertain whether the suture has passed fully through the tarsus. If it has, it must be removed and repassed to prevent corneal irritation and patient discomfort.
Then pass the two arms of your suture through the posterior surface of your levator aponeurosis, at a level depending on the amount of lift needed. Tie a temporary but firm knot, which shores up the aponeurosis and tarsus. Ask the patient to open his eyes and assess contour and height. If too high or too low then release the knot and reposition your levator aponeurosis bites. If the contour is unsatisfactory, the suture must be completely removed and repositioned within the tarsus. The eyelid peak is usually nasal to the pupil and the lid height should sit at the limbus.
We often ask the patient to sit up for a final inspection of the eyelid position. In unilateral cases, positioning the lid for symmetry is important.
 |
| Figure 3: Passing of suture through skin and levator complex to achieve supratarsal fixation for a more defined lid crease. |
Correction of blepharoptosis can be an exigent endeavor in even the most proficient hands. Proper planning and surgical technique are paramount to pleasing outcomes for both the surgeon and the patient. Also remember that results that do not look good at the end of a case are not likely to miraculously improve in the future. Being your own harshest critic is something we find useful in refining and achieving improved outcomes.
Dr. Cohen is a fellow at the Institute for Craniofacial and Reconstructive Surgery, Providence Hospital, Southfield, Mich. Contact him at ajcohenmd@ prodigy.net. Dr. Mercandetti is in private practice and a consultant in eyelid and facial plastic surgery in Sarasota, Fla.
1. Cohen AJ, Mercandetti, M. Ptosis, Adult. In: Ophthalmology/Lid. eMedicine:[serial online] 2001. Available at http://www.e.Medicine. com/ ophthalmology.
2. Periman LM, Sires BS. Floppy eyelid syndrome: a modified surgical technique. Ophthal Plast Reconstr Surg 2002 Sep;18(5):370-2.



