|
Why Surgeons Do It
Surgeons who perform simultaneous, bilateral cataract surgery say it offers patients a number of benefits.
Toronto, Ontario, surgeon Steve Arshinoff says that, many years ago, he would usually only do SB cataract surgery on certain patients for whom two trips to the OR would be difficult, such as someone with Down’s syndrome. In 1998, however, he performed his first SB case on someone who simply wanted it done for convenience’s sake. He agreed to do it, and the patient signed a special consent form for it. “On the day of her surgery I operated bilaterally on her and did the first eyes of maybe 15 other people,” Dr. Arshinoff recalls. “The next day in the office she was ecstatic, much more so than her fellow postop patients, because she could see well out of both eyes. The others had had one eye done and had the issues involved with waiting for the second eye to be done. When I realized how happy she was, I thought that maybe I’d loosen my criteria and do a few more people if they wanted to have it done.” Now, 17 years and nearly 5,000 bilateral cases later, he performs it on 80 to 90 percent of his patients and has become one of the co-founders of the International Society of Bilateral Cataract Surgeons.
Dr. Arshinoff says the postop vision benefits really become important for patients with high refractive errors. “Let’s say you have someone who has a refractive error of +8 D or -8 D,” he says. “When you correct that in only one eye, he is really incapacitated until the second eye is done because he sees double. So, for all those types of patients, rather than try to compromise and make them highly myopic or highly hyperopic, you can aim for any refractive error you think is best for them by doing bilateral surgery. If you implant multifocal lenses, you have fewer problems because, when you’re done, both of the eyes can immediately see close and at distance; you don’t have to worry about the patients comparing an eye with a multifocal to one without it. It’s not that a multifocal IOL is bad—it’s just different and it takes time to adapt. And people adapt to things better when their entire system is adapting to it, not just half of it.”
Some patients need to travel a long distance for cataract surgery, and making that trip twice, in addition to all the extra follow-up visits for each eye, can be a hardship that many acknowledge is one of the main reasons for doing SB. Surgeons say, however, that this convenience can be enjoyed by any patient, not just rare hardship cases. Amarillo, Texas, surgeon Sloan Rush acknowledges the benefits of SB surgery, and is a member of the ISBCS. To help gauge the surgery’s beneficial effect on the patient experience, he recently performed a prospective study of SB surgery vs. sequential cataract surgery. “With the surgeries separated, our patients averaged 7.1 visits to my office,” he says. “With simultaneous, bilateral surgery, they averaged 3.3 visits. That’s a significant feature for our patient population, more than half of whom travel from more than 60 miles away. In fact, the total distance traveled was 522 miles for the simultaneous surgery patients vs. 969 miles for the sequential ones, a difference that was statistically significant. Recovery time was much quicker also; simultaneous surgery patients recovered their best-corrected vision in 3.3 weeks, compared to 5.9 weeks for sequential patients.”
Linköping, Sweden, surgeon Björn Johansson says doing the second eye on the same day as the first helps the surgeon manage the second case. “Should there be any small thing that makes the surgery more difficult than standard, it’s actually better to do the second eye immediately,” he says. “This is because my plan for surgery can be refined based on the result of the first surgery. Of course, you could note the difficulty in the patient record to help plan a second surgery several weeks later, but I’ve found that most of the time it’s an advantage to have the first surgery on your mind when you immediately carry on with the second eye, as long as there hasn’t been a significant complication with the first. For a significant complication, you have to postpone the second eye’s surgery.”
As with any surgery, SB has contraindications. “We ask patients to sleep on their backs for the first couple of days,” says Dr. Arshinoff. “This is to avoid lying on their eyes. However, some can’t sleep on their backs because of arthritis, so we’ll do one eye at a time. We’re also concerned about people who appear to not be very clean and not able to take care of themselves. And if there are any concerns with the retina, lens, cornea or anything else, or they have a chronic infection of the conjunctiva or lids, we’re more careful.”
Dr. Johansson says it takes meticulous patient selection. “You need to be aware of any factors that increase the risk for a complication,” he says. “This includes endothelial dystrophy or diabetic retinopathy with central changes. Also, be aware of the potential for patient noncompliance with postop care. And if you suspect addiction or dementia, it’s still possible to proceed but make sure there’s a network of care around the patient.”
Why Surgeons Are Wary
Putting financial issues aside, from a patient-care standpoint surgeons’ primary concerns with SB cataract surgery revolve around the surgery’s ability to cause a problem for both eyes, and to lose the benefit of using the first eye’s outcome to plan the second eye’s surgery.
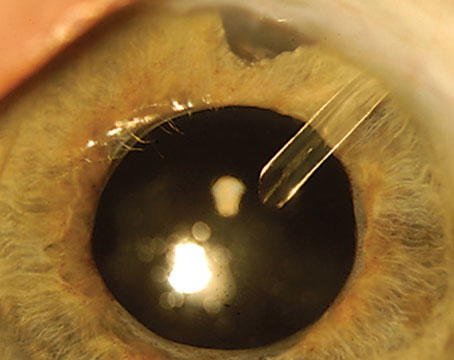
“One of the fears we all have is the fear of potential bilateral endophthalmitis,” says Nick Mamalis, MD, professor of ophthalmology and visual sciences at the University of Utah School of Medicine. “This would be a potential disaster. Fortunately, the reported incidence of bilateral endophthalmitis is very low when proper techniques for preoperative patient preparation and intraoperative/postoperative antibiotics are used. Another area of concern is toxic anterior segment syndrome. This is an issue because when TASS occurs it tends to cluster in a surgical center or an operating room. The problem with TASS is you don’t know it has occurred until the next day. TASS clusters have been caused by all kinds of things, including inadequate instrument cleaning and sterilization, endotoxin contamination and products that are mislabeled or mixed incorrectly. So, theoretically, there’s a small risk you could get bilateral TASS in a patient. Again, it’s not been reported, but is a theoretical concern. Even if you treated each eye as a separate procedure during a simultaneous, bilateral case, if there were a problem with TASS in your facility, from such causes as improper flushing of handpieces or inadequate sterilization, you could end up with a bilateral case of TASS. If it were significant TASS where you’ve got corneal edema and/or glaucoma, that would be difficult to treat.”
SB surgery proponents say they completely understand a surgeon’s concern about bilateral complications, but are quick to point out that if certain strict surgical protocols are followed, the data shows that bilateral complications appear to be exceedingly rare. According to a paper on bilateral complications co-authored by Dr. Arshinoff, there have only been four documented incidences of bilateral complications of SB cataract surgery since 1952, and in each of those, some aspect of the aseptic protocol advocated by the ISBCS wasn’t followed properly.1 In the study, the researchers surveyed the members of the ISBCS about the incidence of postop endophthalmitis and any bilateral endophthalmitis. In 95,606 cases, there were no instances of bilateral infection. The overall rate of postoperative endophthalmitis occurring in just one eye after SB surgery was 1:5,759, which, the researchers said, compared favorably with 1:1,977 in the European studies of intracameral antibiotics and 0.028 percent in a large retrospective U.S. study using topical antibiotics.2,3 With intracameral antibiotics, the rate of infection for the ISBCS surgeons went down to 1:14,352.1
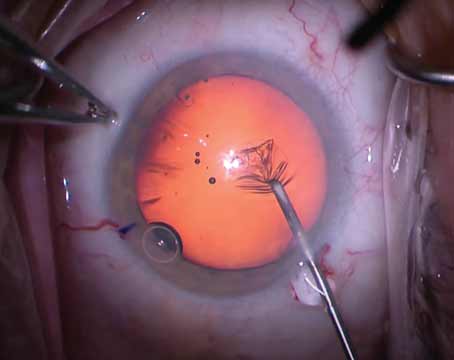
The aseptic protocol referred to in the study, and which SB surgery proponents advocate, basically comes down to treating each eye of the same patient as if it is an entirely separate surgical event. “This means a new surgical drape for the patient, new gowns for the surgeon and nurse, new prep and cleaning of the skin, new supplies, new handpieces, new instrument tray, et cetera,” says Dr. Johansson. “When we first started doing the procedure, we had the patient enter the room and have his first eye done. We’d then do a second patient’s surgery, then bring the first patient back in to do his second eye. We did this for two to three months, just to make everyone aware that the surgeries are meant to be separate.” Surgeons will even use BSS and viscoelastic from different lots or manufacturers just to be sure.
Another objection raised about SB surgery is that it doesn’t allow the surgeon any time to learn from the first eye to improve the refractive outcome on the second. One study that looked at this issue found that by accounting for part of the first eye’s deviation of the postop spherical equivalent refractive error from that predicted by the intraocular lens formula, the surgeon might be able to improve the refractive outcome of the second eye.4 The study noted, however, that since IOLs are made in 0.5-D increments, this might mitigate any beneficial effect of adjusting for the first eye’s error, since it would usually be smaller than 0.5 D. Dr. Arshinoff says newer lens formulas and biometry technology make it more difficult to squeeze any improvement out of the second eye if you wait between surgeries. “A study found that, if you look at different methods, the advantage for correcting for the second eye based on the first decreases as you use better and better techniques,”5 he says. “Basically, if you do things accurately the first time, there’s no benefit from correcting for the first eye’s error because there’s almost no error.”
Intracameral Antibiotics
The use of intracameral antibiotics is one of the underpinnings of SB surgery but, since this method isn’t widely used in the United States, it represents yet another hurdle. (For an in-depth discussion of new trends in antibiotics, see the feature article on p. 28.) Neal H. Shorstein, MD, an ophthalmologist and associate chief of quality with Kaiser Permanente health system in Walnut Creek, Calif., says the results of a study he performed, however, show intracameral is worth pursuing.
In the study, Dr. Shorstein and his colleagues used different antibiotic techniques in three different time periods. In 2007, cataract patients received postop antibiotic drops. In 2008 and 2009, in addition to the drops, they received intracameral cefuroxime, unless contraindicated. Then, in 2010 and 2011, all patients received intracameral cefuroxime, moxifloxacin or vancomycin, with the addition of topical drops left up to the surgeon. Ultimately, the rates of endophthalmitis were 3.13:1,000 in 2007, 1.43:1,000 in 2008/2009, and 0.14:1,000 in 2010/2011.6 There was one case of endophthalmitis in 2,038 patients without a posterior capsule rupture who received only intracameral and no topical antibiotic (0.49:1,000). “With the advent of intracameral antibiotics, and with the marked reductions in endophthalmitis that we’ve seen at Kaiser Permanente, I think this opens the door, on a relatively short timeline, to start thinking about bilateral, same-day surgery,” Dr. Shorstein says.
Financial Roadblocks
Even if the complication data eventually won the hearts and minds of surgeons in the United States, SB cataract surgery would come to a hard stop as far as reimbursement is concerned. To put it simply: Surgeons lose money every time they do it because the Centers for Medicare & Medicaid Services only pays half for the second eye if it’s done in a simultaneous fashion.
“In the United States, it’s ridiculous to pay 50 percent to the surgeon and the ambulatory surgery center for the second eye,” argues Dr. Arshinoff. “When you do two eye surgeries like this, it’s not as if you’re doing the patient’s cataract and then doing a combined cataract and filtration procedure, in which you use the same instrument and just change two more surgical steps. With simultaneous, bilateral surgery, you’re changing all of the drapes, all of the instruments, using a different OVD—the costs are double. Furthermore, when the patient comes back for postop visits, he incurs more costs to the health-care system; no matter how it’s structured, someone is paying.”
|
“We recommend that if you do the surgeries on the same day Medicare pays you 190 percent,” Dr. Rush continues. “This is because you’re still providing postop care, though with fewer visits, so maybe the physician should be willing to take a small hit there. Based on Medicare’s reimbursement for a unilateral, non-complicated cataract in 2013—$629.91—our suggestion would save Medicare $62.99 for each patient that underwent bilateral, same-day surgery. When this is added to the $81.59 saved from eliminating the intermediate exam, the total potential savings to Medicare is $144.58.”
One situation in the United States where economics isn’t an issue with SB surgery is in the Kaiser Permanente health system, especially in sections of Colorado and California. Kaiser Permanente’s Dr. Shorstein says his system’s surgeons are doing more and more SB surgery, with one surgeon’s practice in particular doing between 40 and 50 percent of his 1,000 annual cases in this manner. The reason it’s economically viable at Kaiser Permanente is because it’s an integrated system in which individual physicians don’t contract with Medicare, but instead are reimbursed by the health system, allowing them to perform the surgery they feel is best, with proper informed consent. “In our integrated health-care organization, there are none of the disincentives that are in place in the private sector in which bilateral, same-day surgeries aren’t reimbursed fully,” says Dr. Shorstein. “So, if the patient desires to have both eyes done on the same day as a matter of convenience and rapid recovery, the barriers to that really aren’t there in our organization.”
With so many cases being done on an institutional level, surgeons would be eager to hear about the results of Kaiser Permanente’s SB surgeries. Dr. Shorstein says that data is on its way. “We’re looking at data such as bilateral complications right now,” he says. “We have a team at my local hospital performing a failure modes and effects analysis. The FMEA is looking at all our processes in the clinic and the OR in order to identify any potential failures in the system of bilateral, same-day cataract surgery. We hope to report our findings in a study this year. Three of us at my hospital have been doing it for 12 to 18 months in a very controlled way. This is because with bilateral, same-day surgery there are a number of areas that can be potentially more prone to a mistake than with separate-day surgeries. When both eyes are done on the same day, you have two lenses in the OR, a sheet of paper with different lenses circled for each eye and extra data on each eye floating around that could potentially be confused. It’s been a fairly exhaustive process to try to uncover every conceivable pitfall in the system, since we anticipate ramping up our bilateral cataract surgery offerings.”
Dr. Arshinoff says he thinks surgeons could be successful with SB surgery if they gave it a chance and reimbursement issues fell into place. “There’s always an argument about why not to do a procedure,” he says. “And then, one day, you do a procedure such as bilateral, same-day surgery on the worst patients, such as someone with Down’s syndrome who’s confined to his bed, and find out that he does OK. But that type of patient is the one who probably had the highest risk. So if you can do him, why can’t you do everybody? The truth is you can.” REVIEW
1. Arshinoff S, Bastianelli P. Incidence of postoperative endophthalmitis after immediate sequential bilateral cataract surgery. J Cataract Refract Surg 2011;37:2105-2114.
2. ESCRS Endophthalmitis Study group. Prophylaxis of postoperative endophthalmitis following cataract surgery: Results of the
ESCRS multicenter study and identification of risk factors.
J Cataract Refract Surg 2007; 33:978–988.
3. Wykoff CC, Parrott MB, Flynn HW Jr., et al. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital (2002-2009). Am J Ophthalmol 2010;150:392–398.
4. Covert DJ, Henry CR, Koenig SB. Intraocular lens power selection in the second eye of patients undergoing bilateral, sequential cataract extraction. Ophthalmology 2010;117:1:49-54.
5. Olsen T. Use of fellow eye data in the calculation of intraocular lens power for the second eye. Ophthalmology 2011;118:9:1710.
6. Shorstein NH, Winthrop KL, Herrinton LJ. Decreased postoperative endophthalmitis rate after institution of intracameral antibiotics in a Northern California eye department. J Cataract Refract Surg 2013;39:1:8-14.