Safety Signals
Some of the largest studies in femtosecond cataract have focused on the safety of the procedure.
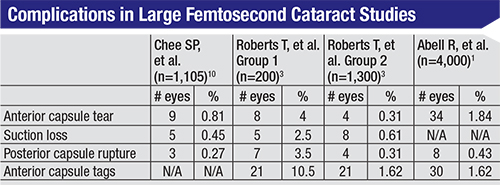
In one of the few prospective, comparative studies of femtosecond cataract surgery vs. conventional surgery, surgeons from Tasmania performed femtosecond surgery on 1,852 eyes (the study group) and conventional surgery on 2,228 eyes (the controls). The researchers reported 34 tears in the anterior capsule (1.84 percent) in the study group vs. five in the control group (0.22 percent), a difference that was statistically significant (p=0.0001).1 They noted that one case of anterior capsule tear in each group extended to the posterior capsule, necessitating an anterior vitrectomy. There were 21 incomplete capsulotomies in the laser group (1.13 percent) vs. none in the conventional patients, as well as 30 anterior capsulotomy tags (1.62 percent) with laser compared to 1 with conventional (0.004 percent; p=0.0001). The surgeons mention that just over half of the anterior radial and posterior capsular tears occurred in the later cases, which was one of the reasons why they didn’t show a learning-curve effect during the study.
 |
Tim Roberts, MBBS, MMed, consultant ophthalmic surgeon at the Royal North Shore Hospital, University of Sydney, believes that the paper by [the Tasmanian] group is important as it has “focused attention on the laser settings used and surgical techniques employed during laser cataract surgery.” Dr. Roberts adds that, “From a surgeon’s perspective, I believe the important question is not whether there are ultrastructural differences between manual and laser-cut capsulotomies, but what the clinical implication, if any, is of these differences.” He points out that his group and others have found very low rates of anterior tears. “When you look at papers such as that by the Moorfields’ group2 and our own study,3 you see other groups with large numbers aren’t finding those high rates,” he says.
In Dr. Roberts’ study, he and his co-authors prospectively analyzed 1,500 femtosecond cataract cases, which they broke into two groups: 200 cases to get a sense of the initial skill level’s impact on results; and then 1,300 to determine if experience with the procedure improved outcomes.
In the first group, the complication rates were higher. Eight cases (4 percent) had anterior radial tears, 21 (10.5 percent) had anterior capsule tags, seven (3.5 percent) had posterior capsule tears and four (2 percent) had posterior lens dislocation. Twenty-six patients (13 percent) had to have manual corneal incisions rather than laser-made cuts because the latter were impossible to make or could be made but not opened.
In the second group in Dr. Roberts’ report, the rates went down: four (0.31 percent) had anterior radial tears; 21 (1.62 percent) had anterior capsular tags; four (0.31 percent) had a posterior capsule tear; and 25 (1.92 percent) needed their incisions done manually. There were no cases of posterior lens dislocation. “What our study and others are suggesting is that with the significant improvements in hardware and software that have occurred—and the surgeons learning more about the procedure—the femtosecond surgeon can expect a much shorter, predictable learning curve,” says Dr. Roberts.
Taking a broad view of the literature, in 2013 the Veterans Administration commissioned a task force to do a meta-analysis of the available peer-reviewed reports on femtosecond cataract surgery and then make a recommendation about whether the VA should implement it in its hospitals. The researchers whittled 468 papers down to 16 that met their validity criteria.
|
Another safety parameter that is emerging is the potential reduction in ultrasound energy needed to remove the cataract when a femtosecond laser is used to segment the nucleus. In a study co-authored by Dr. Reddy, surgeons randomized patients to femtosecond cataract surgery or conventional phaco. Fifty-six eyes had the laser and 63 underwent conventional surgery. The researchers found that the mean effective phaco time was significantly lower in the laser group (5.2 ±5.7 seconds) compared to the manual (7.7 ±6 seconds; p=0.025). There was also a significant difference in the mean phaco energy between the groups (13.8 ±10.3 percent in laser vs. 20.3 ±8.1 percent for manual; p<0.001). However, the safety results of each procedure were equal, with no adverse events in either at one day postop.9 The 4,000-eye study from Tasmania also found that effective phaco time was statistically significantly lower in laser patients, but didn’t find an increased risk of complications that would be associated with this increased time.1
Dr. Reddy says that the exact measurement of phaco time from surgeon to surgeon, as well as its effect on outcomes, isn’t cut-and-dried, however. “I found that femtosecond cataract helped with regard to reduced effective phaco time,” he says, “but, as a surgeon, I can’t say there’s a significant difference between the two modalities. Some doctors have a habit of continuing the energy in between one fragment to another and others don’t. It’s a factor that’s very surgeon-dependent.”
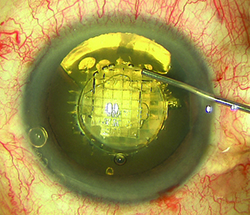
The Capsulotomy
One particular aspect of femtosecond cataract surgery that’s gotten a lot of analysis in the literature is the creation of the capsulotomy.
No one disputes the femtosecond laser’s ability to create a precise, very circular rent in the capsule, and studies have proven how accurate it can be.4,5 Studies have even shown this may help with positioning an intraocular lens postop.6 Controversy has begun, however, after one recent study reported laser capsulotomies may have some weak points that could lead to tearing.7
The tearing paper was a prospective analysis of 804 patients undergoing femtosecond cataract surgery and 822 undergoing conventional phaco. In it, the researchers found a statistically significant increased rate of anterior capsule tears in the laser group (15; 1.87 percent) when compared to the conventional group (1; 0.12 percent). In seven cases, the anterior tear extended to the posterior capsule. The researchers examined tissue samples on scanning electron microscopy and found irregularities at the margin of the capsules, as well as apparently misplaced laser pits in normal segments of the tissue.7 The pits are described as sitting 2 to 4 µm apart at locations 10 to 100 µm radial to the capsule edge. The researchers said that, in some cases, the anterior capsulotomy integrity appeared to be compromised by “postage-stamp” perforations and aberrant laser pulses that may occur due to patient eye movement. They also acknowledged, however, that the surgeon learning curve may be to blame for some of the increased complication rates with the laser procedure.
Dr. Roberts says rates such as these may be outliers, and haven’t been his experience. “We published our safety study of 1,500 patients two years ago and a follow-up study of another 3,000 patients is in press,” he says. “Our anterior capsular tear rate is 0.2 percent now. Other papers, such as that by Julian Stevens at Moorfields which had 0.1 percent, aren’t finding a high rate such as this.”
Hyderabad’s Dr. Reddy says he was involved in an animal model study with Heidelberg, Germany’s, Gerd Auffarth, MD, where they specifically looked at capsulotomy strength in porcine corneas. “We stretched capsulotomies created manually and by a laser,” he says. “The study showed the laser capsulotomies were as good, if not better, than manual ones. Also, if the laser edge is weak from a clinical point of view, then there should be tears in every case, because as we operate we’re pulling fragments through that capsulotomy and we catch the edge as we do it, but there aren’t.”
In the study from Moorfields, surgeons retrospectively reviewed 1,000 laser capsulotomies performed over a period of about a year. They found complete 360-degree capsulotomies in 998 cases (99.8 percent).8 In the two incomplete capsulotomies, one was due to the laser activation having to be aborted, and the second had a tissue tag that became a tear, leading to a 0.1-percent rate of tearing.2
Dr. Reddy adds that there are certain patients with an unusual capsule/zonule configuration who will be easier to operate on using a femtosecond laser, and where the laser capsulotomy would be preferable. “Whenever the anterior zonules are inserting into the anterior capsule, there are some aberrations in some patients,” Dr. Reddy explains. “Some of them get inserted a little more proximal toward the center. So, when you try to do a manual capsulorhexis, these fibers will catch it and from then on, it will be a struggle for the surgeon. But when you do a laser capsulotomy, it cuts all these microscopic fibers, so you’ll never have that problem.”
Visual Results
In terms of refractive results, published studies show femtosecond and conventional surgery both produce very good outcomes.
“As to whether there’s a difference in visual outcomes between conventional and femtosecond cataract surgery, the short answer from our report is no,” says Dr. Gleitsmann. “Of the studies we looked at, and translating all acuities into decimal equivalents, the visual outcomes were no different between those two groups. To make a long story short, the outcomes are so good for conventional surgery that it’s pretty hard to improve on them. Also, the numbers themselves for visual acuity are actually kind of rough. For instance, if someone says, ‘My results are 20/20,’ and someone else says, ‘Mine are 20/18,’ it really isn’t clinically significant.”
|
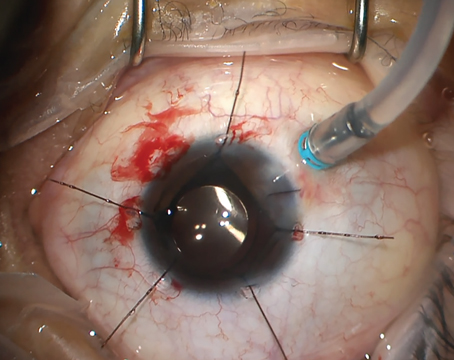
A group from Europe performed a prospective, randomized study of the effects on surgically induced astigmatism of a laser-created entry wound vs. a manual one, since induced astigmatism could affect postop vision. They performed a 2.8-mm clear corneal incision in 20 eyes of 20 patients using a disposable keratome and a 2.8-mm, biplanar clear corneal tunnel in 20 eyes of 20 patients using a femtosecond laser. They found no significant difference in SIA (0.47 ±0.13 D for the laser vs. 0.41 ±0.14 D for the manual incisions; p=0.218), or any difference in induced higher-order aberrations. However, the axis deviation from the planned axis was significantly smaller in the laser group (4.47 ±2.59 degrees vs. 7.38 ±4.72 degrees; p=0.048).11
Challenging Cases
Though there haven’t been studies specifically designed to analyze femtosecond cataract surgery in difficult cases (such as pseudoexfoliation or patients with brunescent lenses), the gestalt that has emerged from the literature is that the laser may put less stress on ocular structures.12
“In our paper, complications didn’t arise in any of these complex cases,”3 says Dr. Roberts. “In fact, we have found that the laser is particularly beneficial in these cases as the capsulotomy is consistently round and intact, eliminating the risk of the manual capsulotomy tearing out when the zonules are weak. Also, a pre-fragmented nucleus allows you to do much less manipulation in the bag—with lower phaco power and time—reducing the risk of zonular dialysis.”
Research shows, however, that surgeons may have to exercise care when using the femtosecond laser for cataract surgery in patients sensitive to intraocular pressure changes, due to the increase in intraocular pressure that occurs during the suction during preop laser docking. A prospective study from Hong Kong used a handheld applanation tonometer to measure intraocular pressure during femtosecond cataract surgery with the Victus in 41 eyes of 35 patients. The mean IOP went from 17.2 mmHg pre-suction to 42.1 mmHg during suction, then back down to 13.8 mmHg after suction. The mean suction duration was 216 seconds. They found the increase was statistically significant compared to pre-suction levels (25 ±11.3 mmHg; p<0.01), and concluded that surgeons should proceed with caution in patients with ocular conditions that are vulnerable to IOP fluctuations.13
Though there is currently a lot of equivalence between laser cataract surgery and conventional phaco in the literature, Dr. Roberts says he expects laser technology to improve. “At a recent Academy meeting, I went to a review of corneal laser surgery,” he says. “During the session, an interesting comment was made that it’s taken many years and many major upgrades to both hardware and software to get where we currently are in terms of the powerful lasers used for corneal grafts and refractive procedures. So, the question becomes: Is the current evidence-based literature what one would expect for laser cataract surgery as a new and evolving technology that has the potential to make surgery more accurate, safer and predictable? I’d argue that it is.” REVIEW
1. Abell RG, Darian-Smith E, Kan JB, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: Outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg 2015;41:1:47-52.
2. Day AC, Gartry DS, Maurino V, Allan BD, Stevens JD. Efficacy of anterior capsulotomy creation in femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2014;40:12:2031-4.
3. Roberts TV, Lawless M, Bali SJ, et al. Surgical outcomes and safety of femtosecond laser cataract surgery: A prospective study of 1500 consecutive cases. Ophthalmology 2013;120:2:227-33.
4. Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg 2009;25:12:1053-60.
5. Friedman NJ, Palanker DV, Schuele G, Andersen D, Marcellino G, Seibel BS, et al. Femtosecond laser capsulotomy. J Cataract Refract Surg 2011;37:1189–1198.
6. Kránitz K, Takacs A, Miháltz K, Kovács I, Knorz MC, Nagy ZZ. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorhexis parameters and their effects on intraocular lens centration. J Refract Surg 2011;27:8:558-63.
7. Abell RG, Davies PE, Phelan D, Goemann K, McPherson ZE, Vote BJ. Anterior capsulotomy integrity after femtosecond laser-assisted cataract surgery Ophthalmology 2014;121:1:17-24.
8. Auffarth GU, Reddy KP, Ritter R, Holzer MP, Rabsilber TM. Comparison of the maximum applicable stretch force after femtosecond laser-assisted and manual anterior capsulotomy. J Cataract Refract Surg 2013;39:1:105-9.
9. Sándor GL, Kiss Z, Bocskai ZI, Kolev K, Takács AI, Juhász E, Kránitz K, Tóth G, Gyenes A, Bojtár I, Juhász T, Nagy ZZ. Comparison of the mechanical properties of the anterior lens capsule following manual capsulorhexis and femtosecond laser capsulotomy. J Refract Surg 2014;30:10:660-4.
10. Chee SP1, Yang Y2, Ti SE3. Clinical Outcomes in the first 2 years of Femtosecond Laser-assisted Cataract Surgery. Am J Ophthalmol 2015 Jan 26. [Epub ahead of print]
11. Nagy ZZ, Dunai A, Kránitz K, et al. Evaluation of femtosecond laser-assisted and manual clear corneal incisions and their effect on surgically induced astigmatism and higher-order aberrations. J Refract Surg 2014;30:8:522-5.
12. Hatch KM, Talamo JH. Laser-assisted cataract surgery: Benefits and barriers. Curr Opin Ophthalmol 2014;25:1:54-61.
13. Baig NB, Cheng GP, Lam JK, et al. Intraocular pressure profiles during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2014;40:11:1784-9.