Usually, minimal connective tissue remnants do not affect vision, although, if symptomatic, mydriatic agents may occasionally mitigate a partially obstructed aperture. Larger membranes may disrupt the visual axis, resulting in either visual symptoms or amblyogenic opacities requiring surgical excision or laser lysis.
In each of the following three cases of clinically significant persistent pupillary membranes. the membrane was crucial to the clinical management.
Background
During the first year of life, most PPMs undergo atrophy and require no treatment. Membranes persisting after one year are less likely to regress spontaneously, increasing the risk of deprivational amblyopia. A 1.5-mm pupillary opening is necessary for adequate retinal stimulation and visual cortex development.
Thick, fibrotic membranes may also require surgical excision. Surgery is generally performed in the first weeks or months of life, with good visual prognosis and consists of excision of the pupillary membrane using Vannas or vitreous scissors. Older patients with thin, sparse membranes may be candidates for Nd:YAG laser membrane lysis.
Visual impairment caused by pupillary membranes can increase as the membrane progresses, and surgical excision returns visual function to baseline, demonstrating that pupillary membranes may not always be amblyogenic in earlier years, as shown by the multi-line visual improvement showed on our second case.
 |
Pupillary membranes are not all dense, fibrotic or evident. In case number three, it appeared as though the vitreous had prolapsed into the anterior chamber, which was compatible with an inferior lens subluxation. Careful slit lamp examination showed that the strands originated at the pupil margin and the zonular apparatus, although stretched, had no structural gaps, revealing the presence of a misleading pupillary membrane. This clinical finding modified the surgical plan and avoided an unnecessary anterior vitrectomy. Accurate recognition and understanding of PPM’s clinical implications can guide the clinical management of complex anterior segment cases.
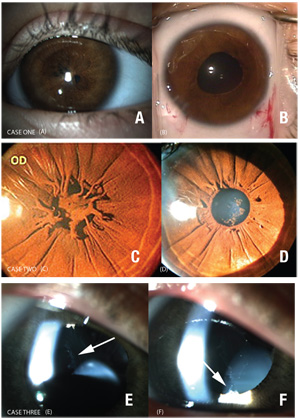
Case One
|
Case Two
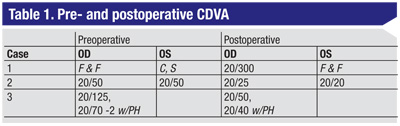
A 23-year-old male presented with progressively decreasing vision and a corrected distance visual acuity (CDVA) of 20/50 in both eyes. Biomicroscopy revealed a network of thick and pigmented strands over both pupils, attaching at the collarette, with apparent apposition to the clear crystalline lens (See Figure 1C). The potential acuity meter tested 20/30 for both eyes.
After surgical excision, vision improved to 20/20 on the left eye and 20/25 on the right eye, despite the presence of a few intralenticular blisters (See Figure 1D).
Case Three
A 28-year-old male was referred for surgical management of inferiorly subluxed microspherophakic lenses in both eyes with a CDVA of 20/70 with pinhole. Slit lamp examination of the right eye revealed a subluxed and mobile microspherophakic lens, moderate posterior subcapsular crystalline lens changes and a wispy greyish white rete over the stretched superior zonules protruding to the anterior chamber through the pupil (See Figure 1E, F). The “prolapsed” anterior chamber wisps appeared nearly identical to condensed anterior hyaloid gel, yet with scrutinizing inspection, attachments to the collarette and absence of zonular gaps confirmed a thin pupillary membrane as the entity.
The membrane was peeled at the time of capsulorhexis and phacoemulsification with a sutured capsular tension ring and in the bag IOL insertion was successfully performed.
This congenital anomaly may be frequently encountered in practice, but with succesful treatment, outcomes can be very favorable. REVIEW
Dr. Shah is a resident at William Beaumont Hospital. Dr. Perez is a fellow at University of Toronto - Toronto Western Hospital. Dr. Snyder is on the Board of Directors at Cincinnati Eye Institute and volunteer faculty at the University of Cincinnati. Both Drs. Marquez practice in São Paolo, Brazil.